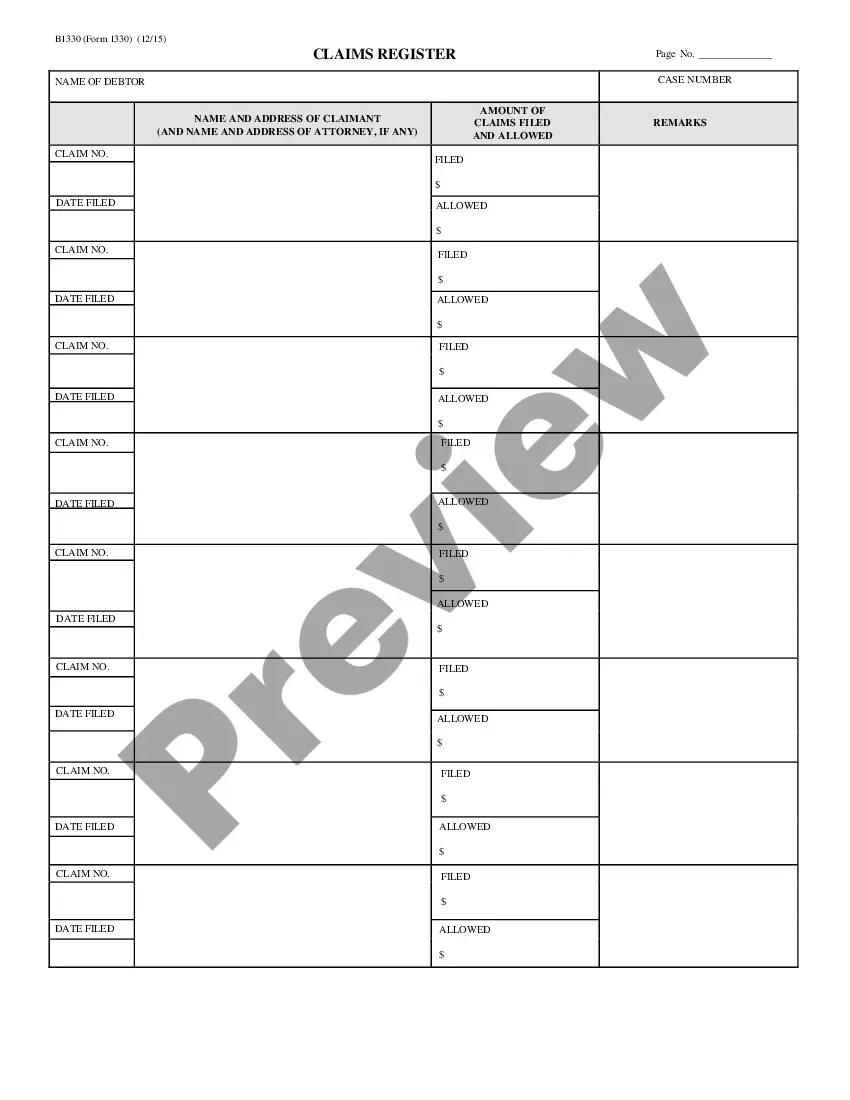
Arizona Claims Register - B 133
Description
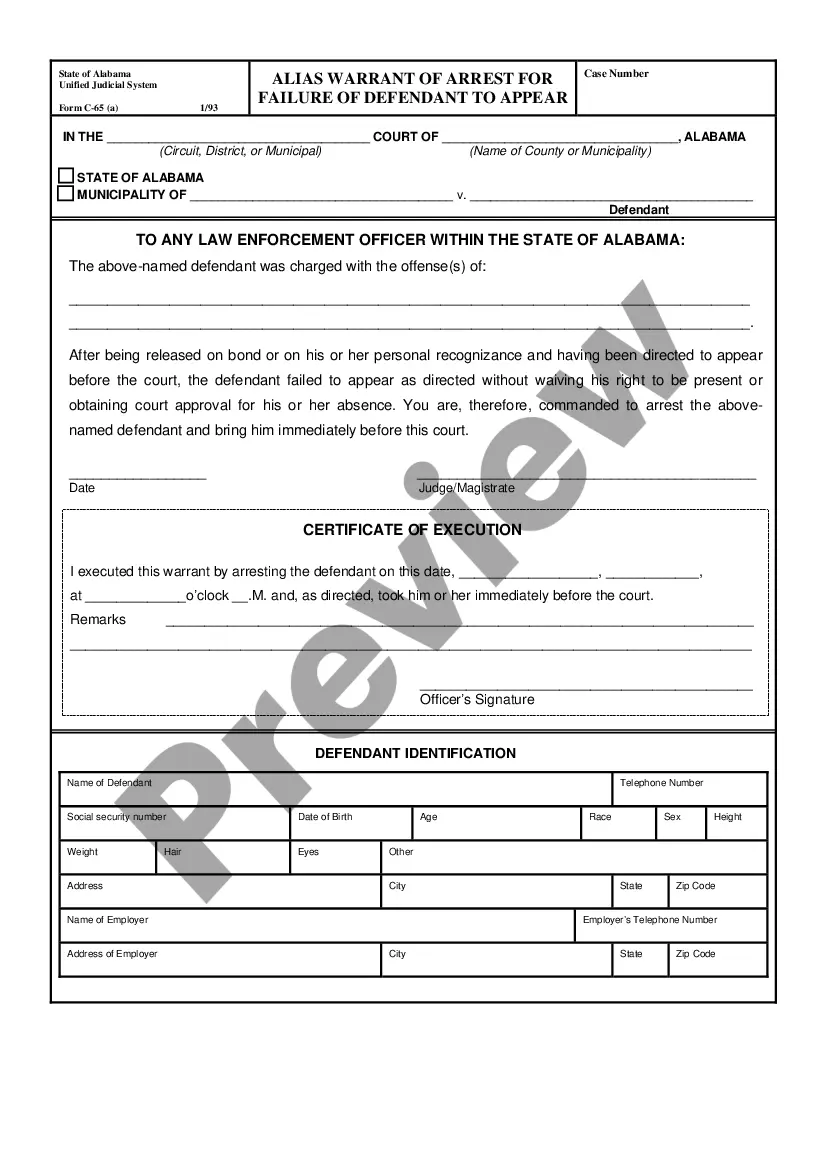
How to fill out Claims Register - B 133?
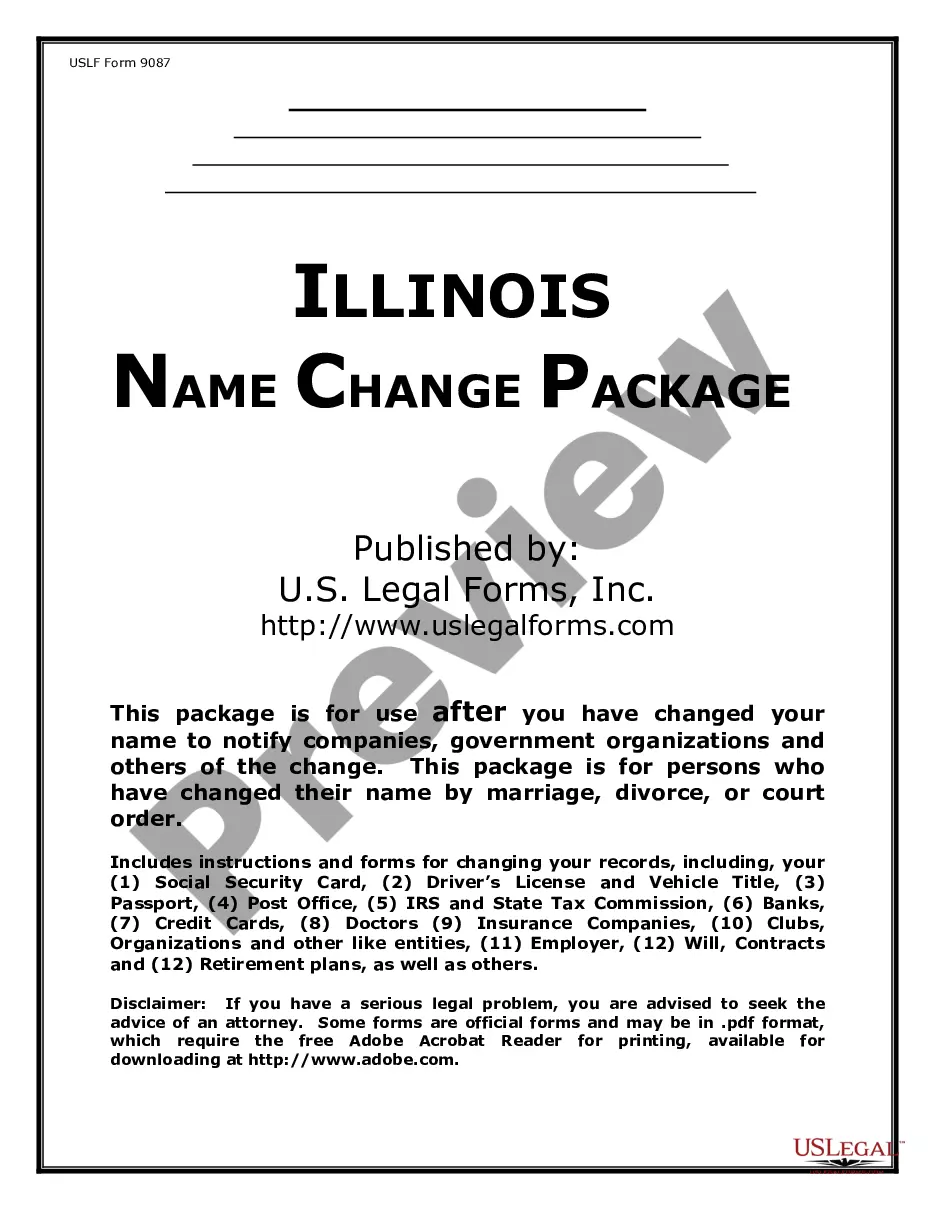
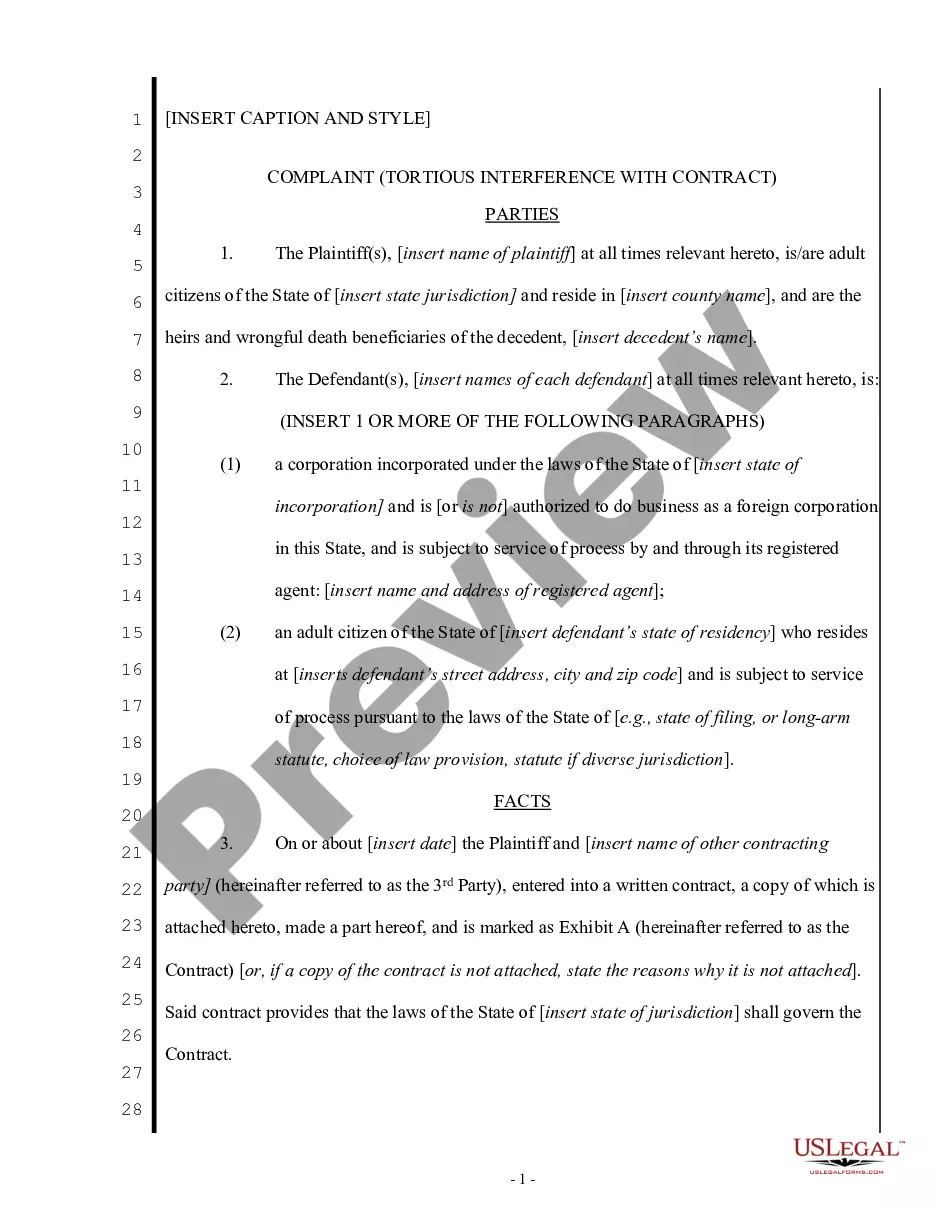
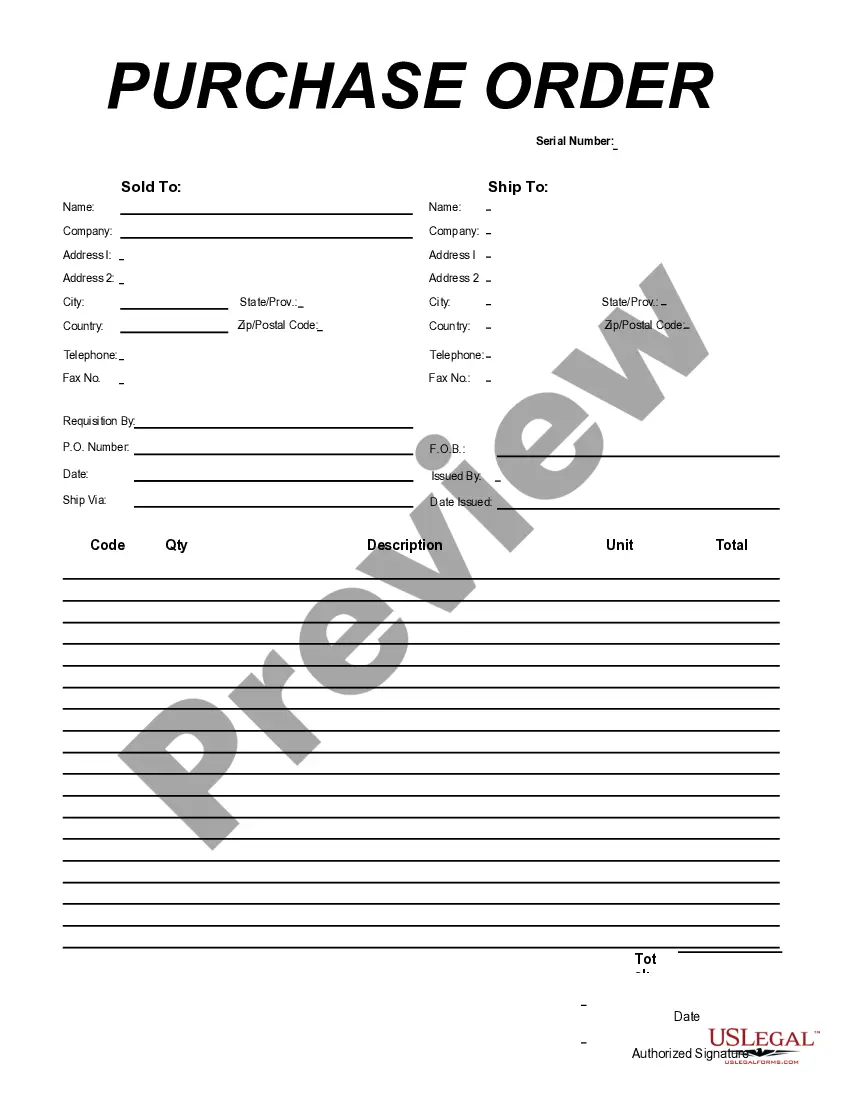
Choosing the best lawful file template can be quite a battle. Naturally, there are plenty of themes available on the net, but how would you discover the lawful kind you will need? Utilize the US Legal Forms site. The support offers 1000s of themes, including the Arizona Claims Register - B 133, which you can use for company and private requirements. All the forms are checked out by professionals and satisfy federal and state requirements.
When you are previously signed up, log in to the profile and click the Down load option to have the Arizona Claims Register - B 133. Utilize your profile to check through the lawful forms you may have acquired earlier. Check out the My Forms tab of the profile and obtain yet another backup of the file you will need.
When you are a new user of US Legal Forms, allow me to share basic guidelines that you should comply with:
- First, be sure you have selected the proper kind for your metropolis/region. You can check out the form making use of the Review option and study the form information to guarantee it is the best for you.
- In case the kind does not satisfy your requirements, utilize the Seach area to find the right kind.
- When you are certain the form is suitable, click on the Purchase now option to have the kind.
- Opt for the rates prepare you need and enter in the necessary information. Make your profile and buy the transaction utilizing your PayPal profile or bank card.
- Pick the document file format and download the lawful file template to the gadget.
- Comprehensive, revise and print and signal the acquired Arizona Claims Register - B 133.
US Legal Forms may be the greatest local library of lawful forms for which you can find numerous file themes. Utilize the company to download expertly-produced documents that comply with status requirements.
Form popularity
FAQ
Section 50 of the Medicare Claims Processing Manual establishes the standards for use by providers and suppliers (including laboratories) in implementing the Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131.
Under certain circumstances, it may be necessary to indicate that a procedure or service is significantly greater than usually required.
Confirm or update basic information like addresses, phone numbers, employer, and insurance plan at every patient encounter. Verify eligibility and authorization before the date of service ? These steps are critical for submitting clean claims yet account for about a quarter of all denials.
Medicare claim process You present your Medicare ID card to your health care provider. Your provider sends your claim to Medicare. Medicare pays first and sends payment directly to the provider. Medicare sends you a statement saying what you owe. You pay the balance to the provider directly.
First time submission must be received within 120 days from the date of service for participating providers and within 180 days from the date of service for non- participating providers.
Arizona Revised Statute §36-2903.01(K) prohibits providers from billing AHCCCS members, including QMB Only, for AHCCCS-covered services. With TPL, AHCCCS pays the difference between the AHCCCS Capped Fee- for-Service fee schedule and the total amount paid by all the coverage plans.
Modifier 51 is defined as multiple surgeries/procedures. Multiple surgeries performed on the same day, during the same surgical session. Diagnostic Imaging Services subject to the Multiple Procedure Payment Reduction that are provided on the same day, during the same session by the same provider.
What Is the Medicare Claims Processing Manual? The CMS Claims Processing Manual is part of the Internet-Only Manual (IOM) repository, which provides access to comprehensive information about CMS-administered programming.