Alaska Election Form for Continuation of Benefits - COBRA
Description
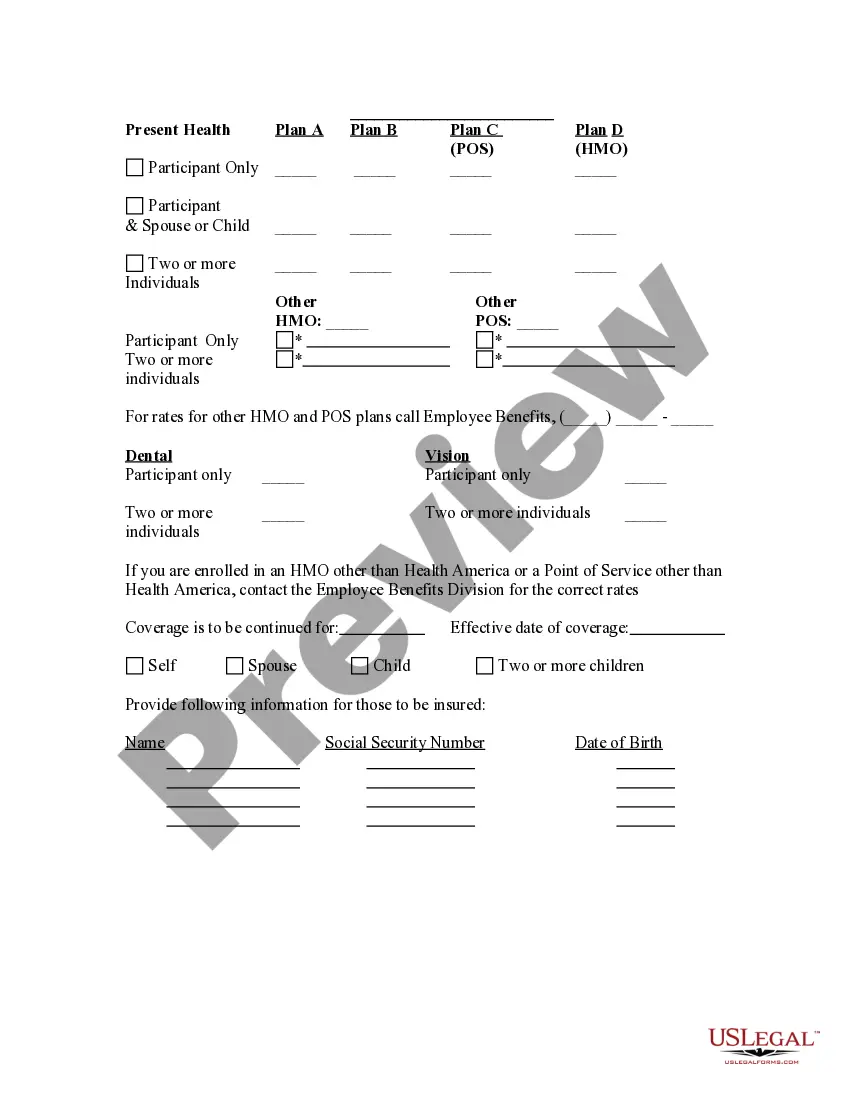
How to fill out Election Form For Continuation Of Benefits - COBRA?
You are capable of spending hours online searching for the legal document template that meets the federal and state requirements you need.
US Legal Forms offers thousands of legal forms that can be reviewed by experts.
You can easily obtain or print the Alaska Election Form for Continuation of Benefits - COBRA from the service.
First, ensure that you have selected the correct document template for the region/city of your preference. Review the form details to confirm you have chosen the right template. If available, take advantage of the Preview button to check the document template simultaneously.
- If you already possess a US Legal Forms account, you can Log In and then click the Download button.
- After that, you can complete, modify, print, or sign the Alaska Election Form for Continuation of Benefits - COBRA.
- Every legal document template you purchase is yours permanently.
- To retrieve another copy of the downloaded form, go to the My documents tab and click the relevant button.
- If you are using the US Legal Forms site for the first time, follow the straightforward instructions below.
Form popularity
FAQ
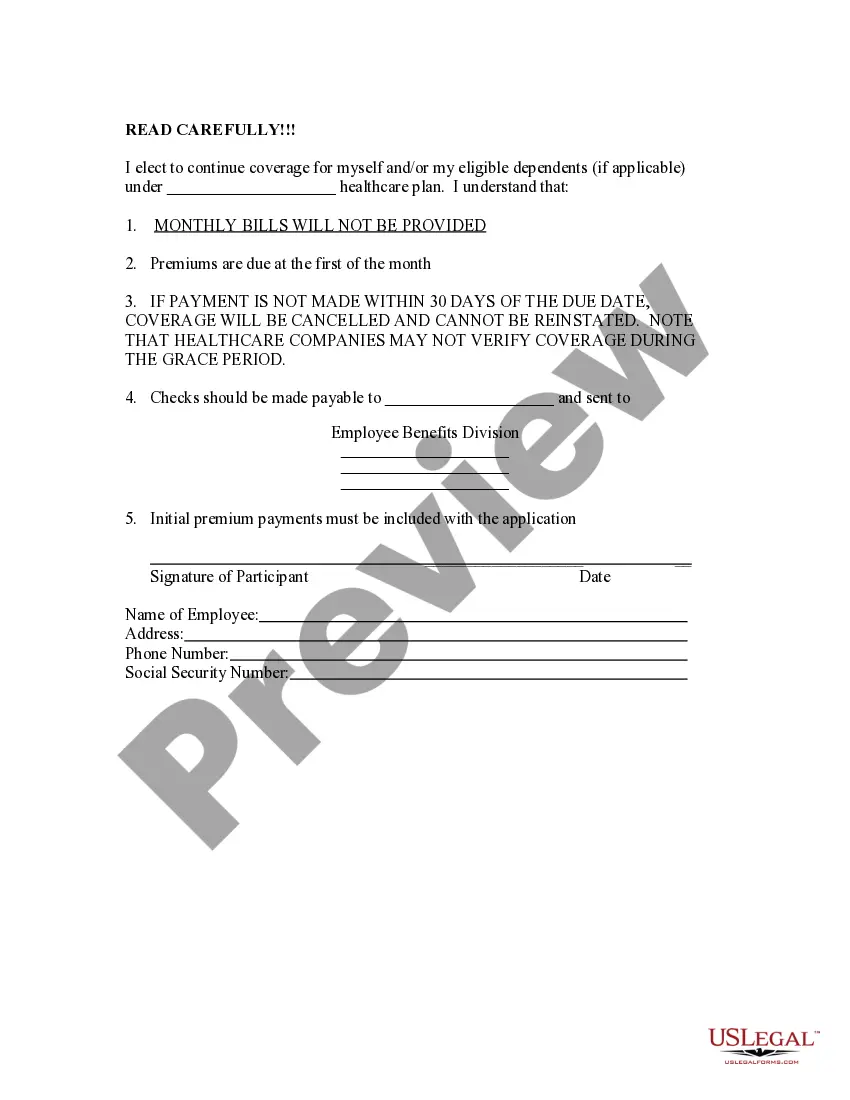
In calculating premiums for continuation coverage, a plan can include the costs paid by both the employee and the employer, plus an additional 2 percent for administrative costs.
COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
You'll have 60 days to enroll in COBRA or another health plan once your benefits end. But keep in mind that delaying enrollment won't save you money. COBRA is always retroactive to the day after your previous coverage ends, and you'll need to pay your premiums for that period too.
Q11: How long does COBRA coverage last? COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
Qualified beneficiaries must be given an election period of at least 60 days during which each qualified beneficiary may choose whether to elect COBRA coverage. This period is measured from the later of the date of the qualifying event or the date the COBRA election notice is provided.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
State continuation coverage refers to state laws that allow people to extend their employer-sponsored health insurance even if they're not eligible for extension via COBRA. As a federal law, COBRA applies nationwide, but only to employers with 20 or more employees.
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.