Service Agreement Provider Contract With Medicare In Clark
Description
Form popularity
FAQ
The CMS-1500 form is the official standard Medicare and Medicaid health insurance claim form required by the Centers for Medicare & Medicaid Services (CMS) of the U.S. Department of Health & Human Services.
Providers sending professional and supplier claims to Medicare on paper must use Form CMS-1500 in a valid version. This form is maintained by the National Uniform Claim Committee (NUCC), an industry organization in which CMS participates.
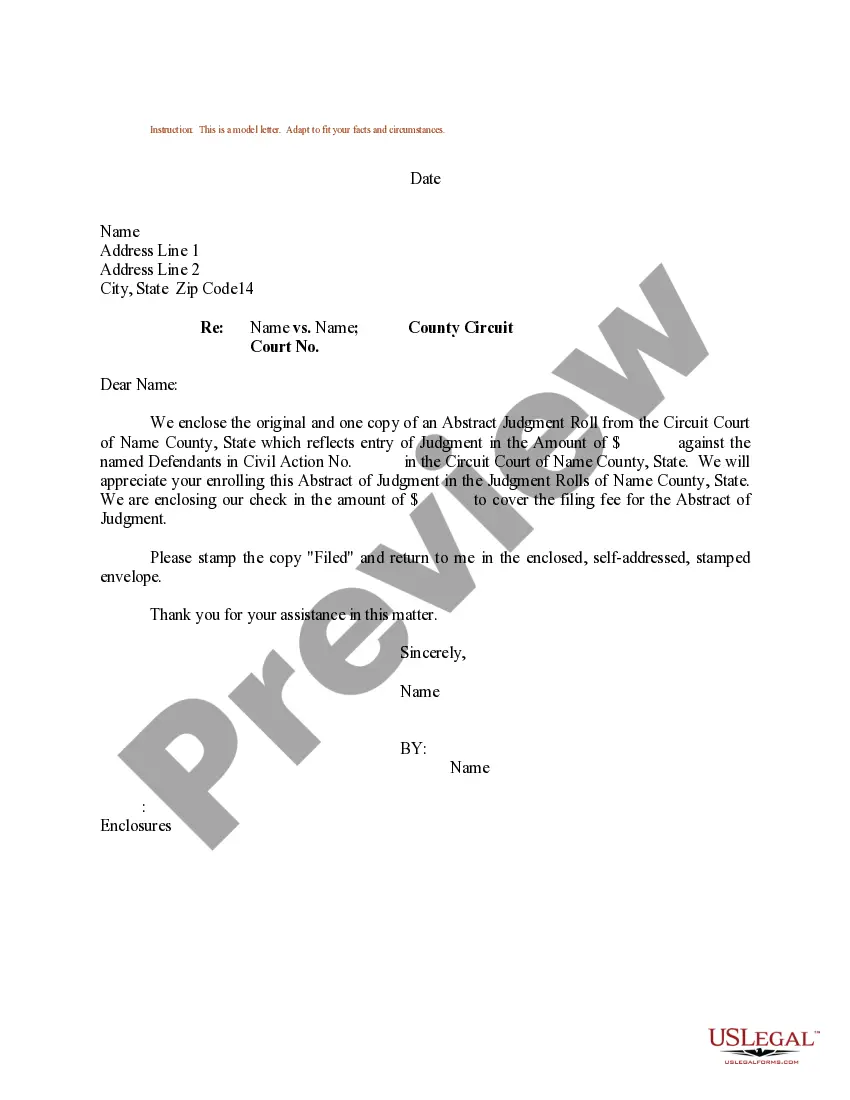
The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
Electronic Claims can be submitted in a single batch. To batch submit claims, navigate to Insurance > Pending Claims. From this view, you will see all of the services that are pending submission. From this screen, all pending claims can be selected at once by clicking the check box at the top left.
WHAT TO DO IF YOU'RE A NEW PHYSICIAN, PRACTITIONER OR SUPPLIER: If you choose to be a participant: Complete the blank agreement (CMS-460) and submit it with your Medicare enrollment application to your MAC.
In summary, a provider, whether participating or nonparticipating in Medicare, is required to bill Medicare for all covered services provided. If the provider has reason to believe that a covered service may be excluded because it may be found not to be reasonable and necessary the patient should be provided an ABN.
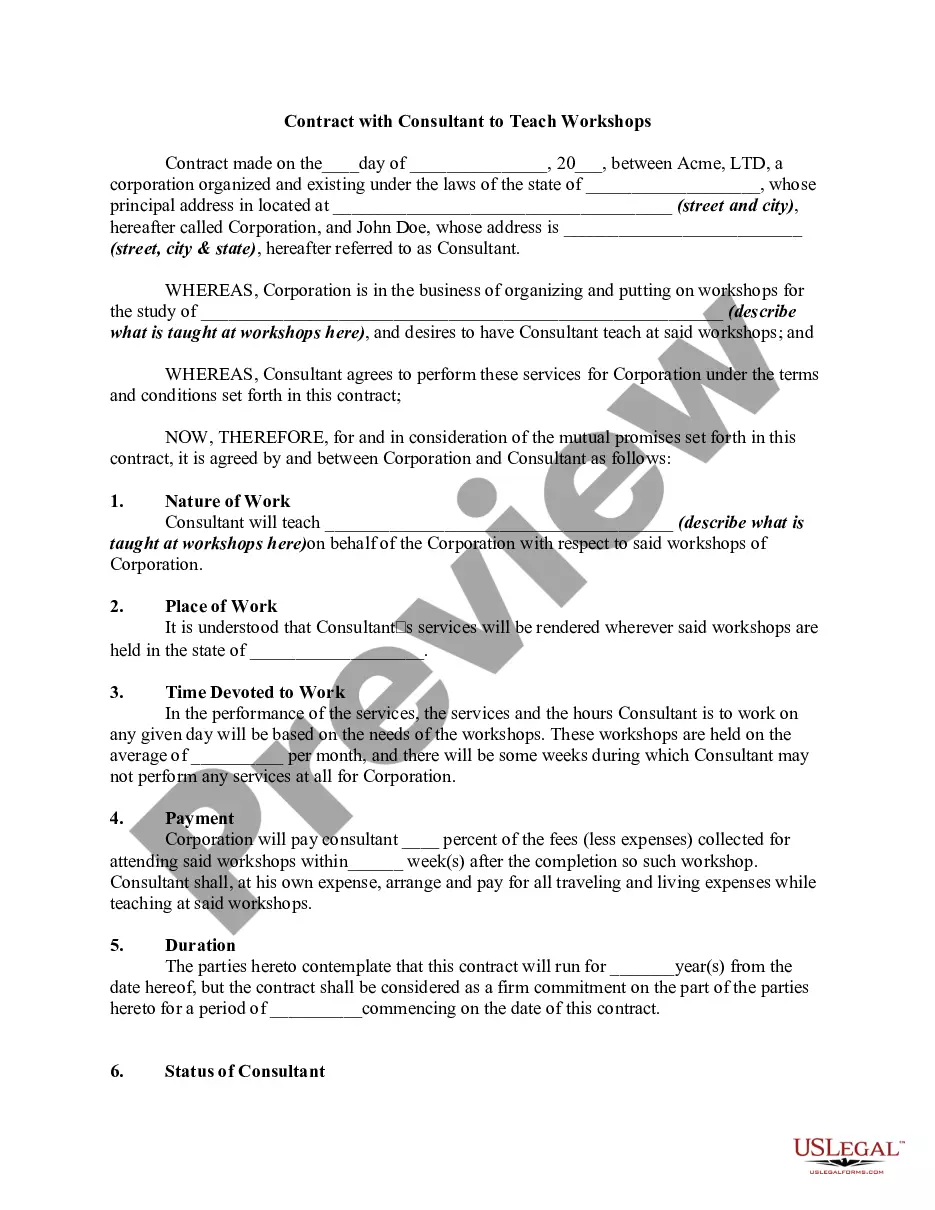
A private contract is an agreement between two or more people that creates obligations that can be enforced by law. It can be a written document or just a verbal agreement. The contract outlines what each person involved must do and what they will receive in return.