Here Denied Claim For Primary Eob In Houston
Description
Form popularity
FAQ
Nationwide, high-volume insurers with higher in-network denial rates across HealthCare states included Blue Cross Blue Shield of Alabama (35% for its 12 plans in that state), UnitedHealth Group (33% across 274 plans in 20 states), Health Care Service Corporation (29% across 915 plans in four states), Molina ...
How to Appeal a Denied Claim Step 1: Review Your Plan. Check your health plan documents or contact your health plan or employer for details on your plan's appeal process. Step 2: Submit Your Appeal. Step 3: Keep Copies. Step 4: Requesting an Independent Review.
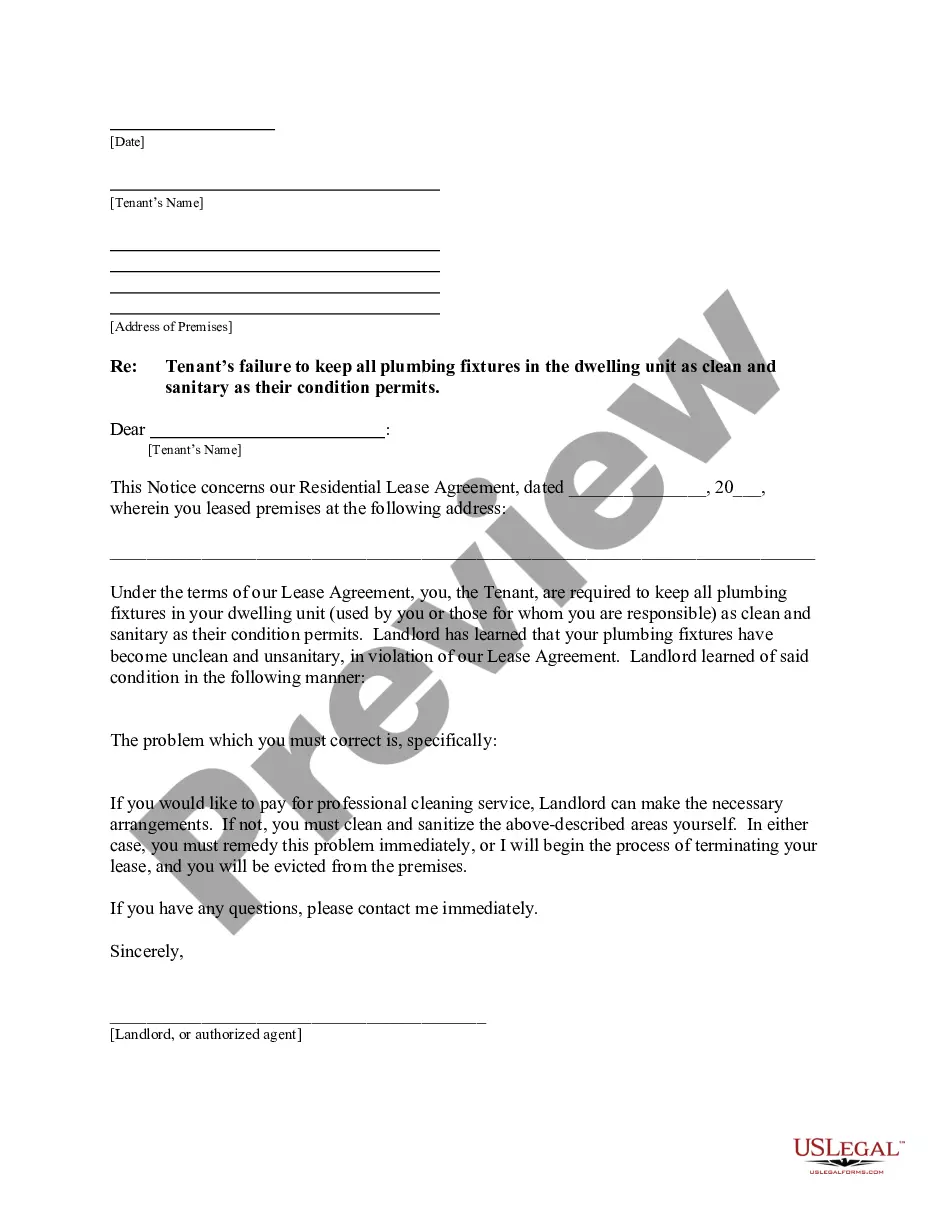
Claim denials often stem from poor communication between payer and provider systems, with the prior authorization process as a prime example. The process requires providers to seek agreement from the payer to cover a service or item before it is administered to the patient.
When appealing against a guilty verdict a defendant might say: there was something unfair about the way their trial took place. a mistake was made in their trial. the verdict could not be sustained on the evidence.
Steps to Appeal a Health Insurance Claim Denial Step 1: Find Out Why Your Claim Was Denied. Step 2: Call Your Insurance Provider. Step 3: Call Your Doctor's Office. Step 4: Collect the Right Paperwork. Step 5: Submit an Internal Appeal. Step 6: Wait For An Answer. Step 7: Submit an External Review. Review Your Plan Coverage.
How to Appeal a Denied Claim Step 1: Review Your Plan. Check your health plan documents or contact your health plan or employer for details on your plan's appeal process. Step 2: Submit Your Appeal. Step 3: Keep Copies. Step 4: Requesting an Independent Review.
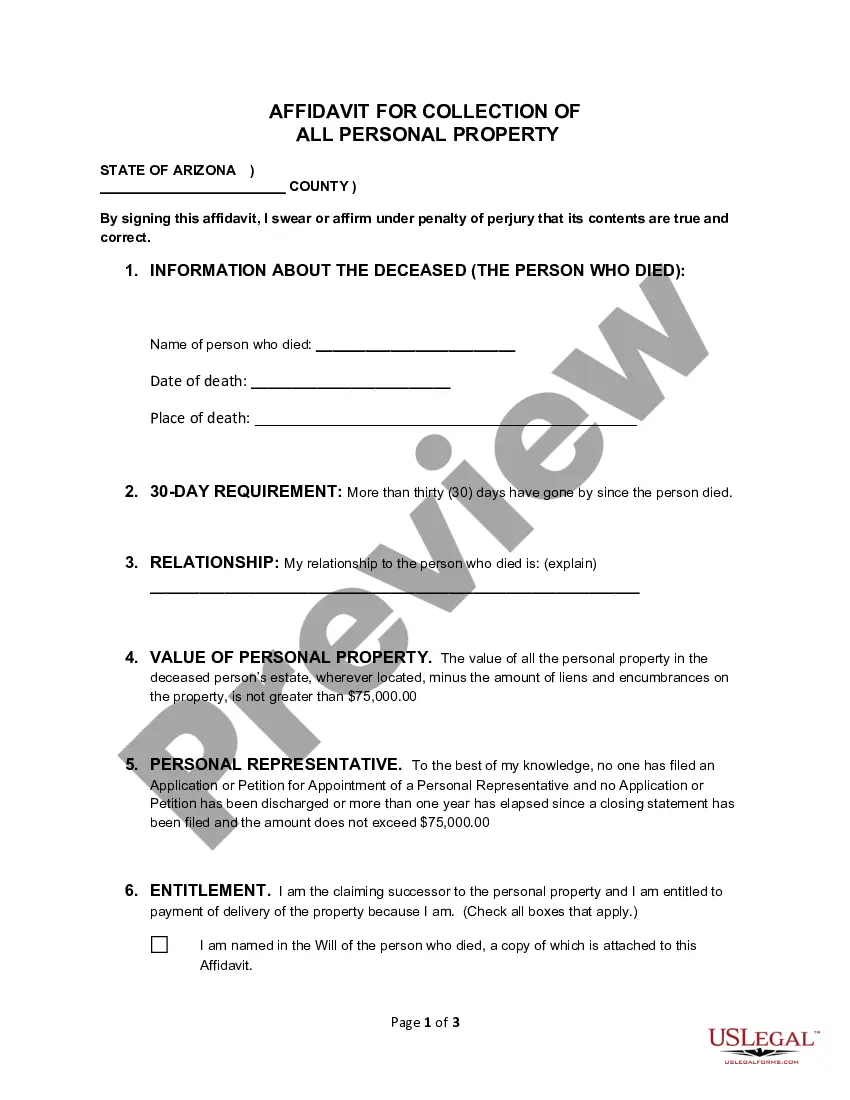
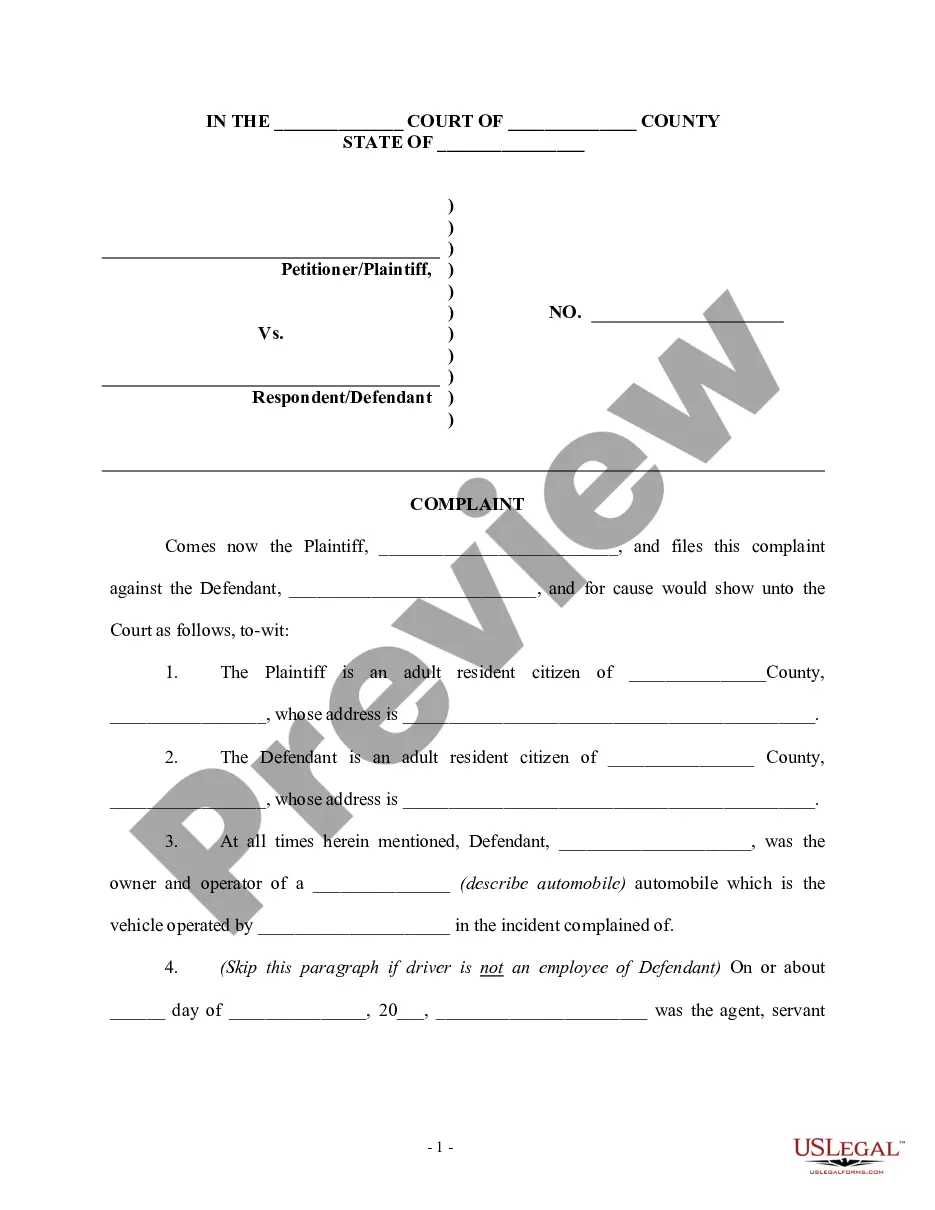
If your resubmitted claim is denied and you believe the denial was improper, you may appeal the decision ing to the carrier's guidelines. Make sure you know exactly what information you need to submit with your appeal. Keep in mind that appeal procedures may vary by insurance company and state law.
Insurance companies may deny various services or treatments for PI, but you have the right to appeal that decision, generally within 180 days of receiving the denial. The explanation of benefits (EOB) for the denied claim must provide information on how to appeal the decision and the amount of time you have to do so.
Consider appealing the decision. If you're denied life insurance on the basis of incorrect or insufficient information, you have the right to appeal the decision. You'll have the best chance of winning your appeal by submitting timely and complete information.