Here Denied Claim For Primary Eob In Contra Costa
Description
Form popularity
FAQ
Ways to File a Grievance or Appeal Call Member Services, Monday – Friday, 8am – 5pm at 1-877-661-6230 (Option 2) (TTY 711). If you have a clinically urgent issue, you can also reach our 24 Hour Nurse Advice Line at 1-877-661-6230 (Option 1).
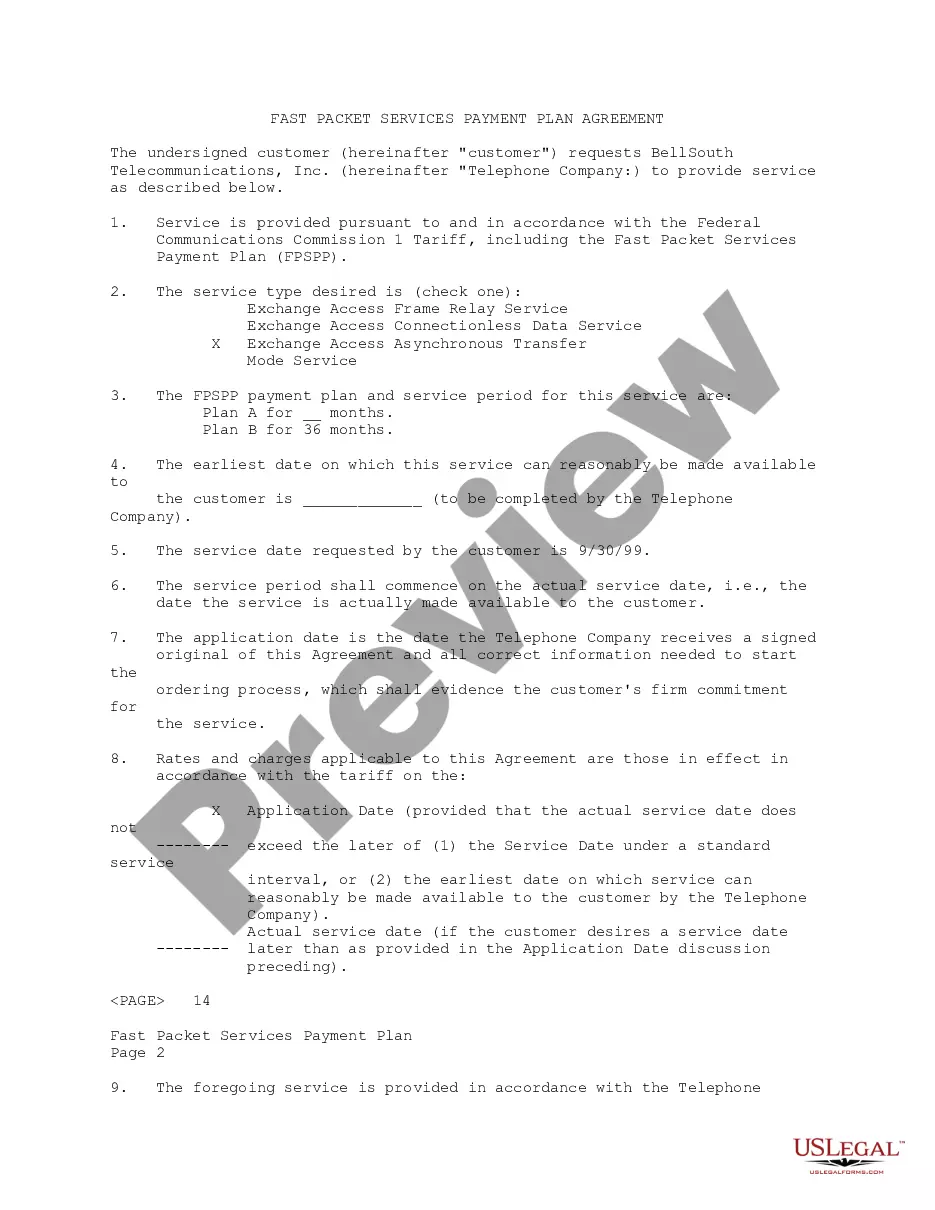
1. The Provider or his/her designee may request an appeal in writing within 365 days of the date of service 2. Detailed information and supporting written documentation should accompany the appeal 3. Providers may obtain assistance in filing an appeal by contacting Optima Health Provider Relations.
CCHP is the primary managed-care provider for Medi-Cal beneficiaries in Contra Costa and we also manage smaller plans for county employees and IHSS homecare workers. Our members have access to hundreds of family medicine doctors and specialists in our provider networks.
Timely filing is when an insurance company put a time limit on claim submission. For example, if a insurance company has a 90-day timely filing limit that means you need to submit a claim within 90 days of the date of service.
If you are: a person (this includes sole-proprietors) you may claim up to $12,500; if you are a Corporation, limited liability company or partnership, you may claim up to $6,250.
Submitting Claims The claim submission timeframe for Contra Costa Health Plan is 180 days from the date of service, or primary explanation of benefits (EOB), for both contracted and non-contracted providers. Claims received after 180 days will be denied for untimely filing.
CCHP is the primary managed-care provider for Medi-Cal beneficiaries in Contra Costa and we also manage smaller plans for county employees and IHSS homecare workers. Our members have access to hundreds of family medicine doctors and specialists in our provider networks.