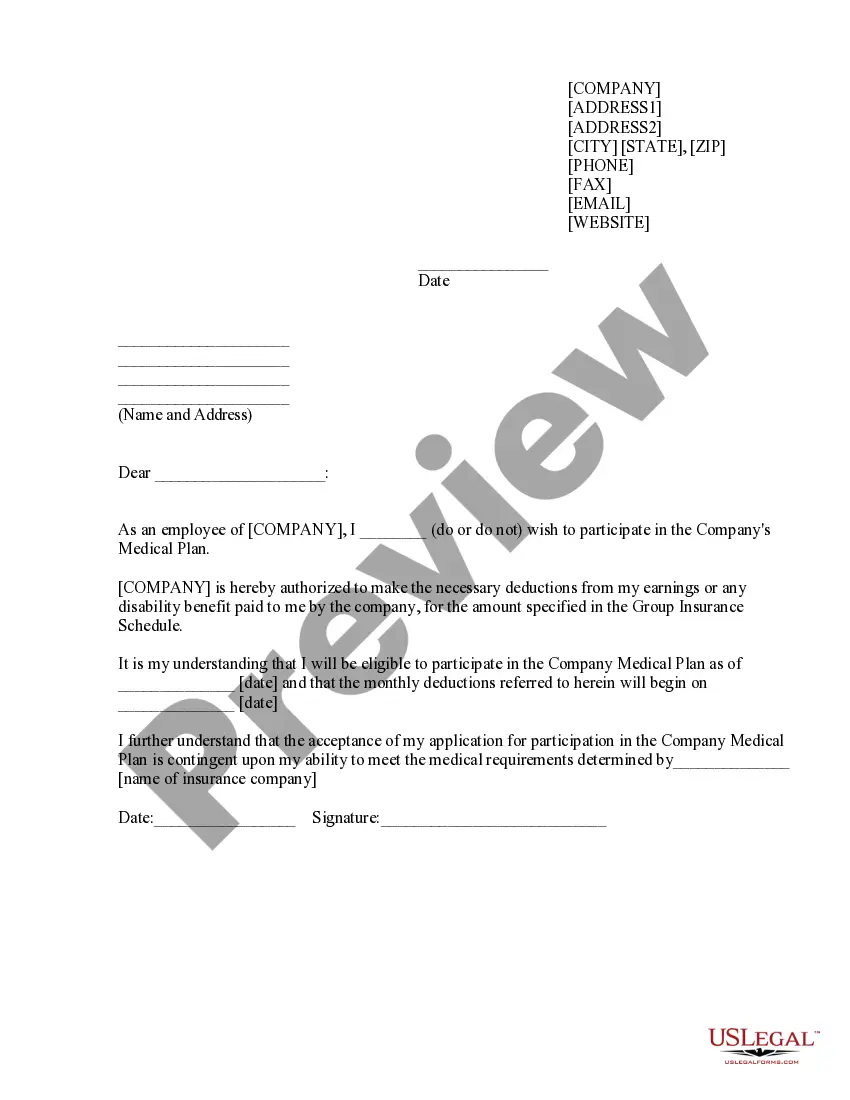
Wayne Michigan Sample Letter for Authorization to Participate in Medical Plan
Description
How to fill out Sample Letter For Authorization To Participate In Medical Plan?
Drafting documents for business or individual requirements is always a significant obligation.
When formulating an agreement, a public service application, or a power of attorney, it is essential to consider all federal and state regulations of the specific area.
Nonetheless, small counties and even municipalities also have legislative regulations that you must take into account.
Utilize the search tab in the page header to locate the document that meets your requirements.
- All these aspects contribute to making it challenging and time-intensive to create a Wayne Sample Letter for Authorization to Participate in Medical Plan without professional assistance.
- It is simple to avoid unnecessary expenses on attorneys for drafting your documents and generate a legally sound Wayne Sample Letter for Authorization to Participate in Medical Plan independently by utilizing the US Legal Forms web library.
- This is the largest online compilation of state-specific legal templates that have been professionally verified, ensuring their legitimacy when choosing a sample for your county.
- Former subscribers merely need to Log In to their accounts to download the required document.
- If you do not yet have a subscription, adhere to the step-by-step instructions below to acquire the Wayne Sample Letter for Authorization to Participate in Medical Plan.
- Review the page you have opened and verify if it contains the sample you are seeking.
- To achieve this, utilize the form description and preview if these options are available.
Form popularity
FAQ
How to Write a Pre-authorization Letter for a Medical Procedure The demographic information of the patient (name, date of birth, insurance ID number and more) Provider information (both referring and servicing provider)Requested service/procedure along with specific CPT/HCPCS codes. Diagnosis (ICD code and description)
The most common example is a cosmetic procedure, such as the injection of medications, such as Botox, to decrease facial wrinkles or tummy-tuck surgery. Many health insurance companies also will not cover procedures that they determine to be experimental or not proven to work.
What is a Prior Authorization? A prior authorization (PA), sometimes referred to as a pre-authorization, is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine, medical device or procedure.
The PATIENT NAME has a diagnosis of DIAGNOSIS and needs treatment with INSERT PRODUCT, and that INSERT PRODUCT is medically necessary for him/her as prescribed. On behalf of the patient, I am requesting approval for use and subsequent payment for the TREATMENT.
Unlike pre-certification, pre-authorization requires medical records and physician documentation to prove why a particular procedure was chosen, to determine if it is medically necessary and whether the procedure is covered.
A letter of medical necessity (LMN) is a letter written by your doctor that verifies the services or items you are purchasing are for the diagnosis, treatment or prevention of a disease or medical condition. This letter is required by the IRS for certain eligible expenses.
Proving Medical Necessity Standard Medical Practices.The Food and Drug Administration (FDA)The Physician's Recommendation.The Physician's Preferences.The Insurance Policy.Health-Related Claim Denials.
16 Tips That Speed Up The Prior Authorization Process Create a master list of procedures that require authorizations. Document denial reasons. Sign up for payor newsletters. Stay informed of changing industry standards. Designate prior authorization responsibilities to the same staff member(s).
How does prior authorization work? First, a healthcare provider determines that a patient needs a specific procedure, test, medication or device. The onus is on the provider to then check a health plan's policy rules or formulary to determine if a prior authorization is required for the prescribed course of treatment.
The most common example is a cosmetic procedure, such as the injection of medications, such as Botox, to decrease facial wrinkles or tummy-tuck surgery. Many health insurance companies also will not cover procedures that they determine to be experimental or not proven to work.