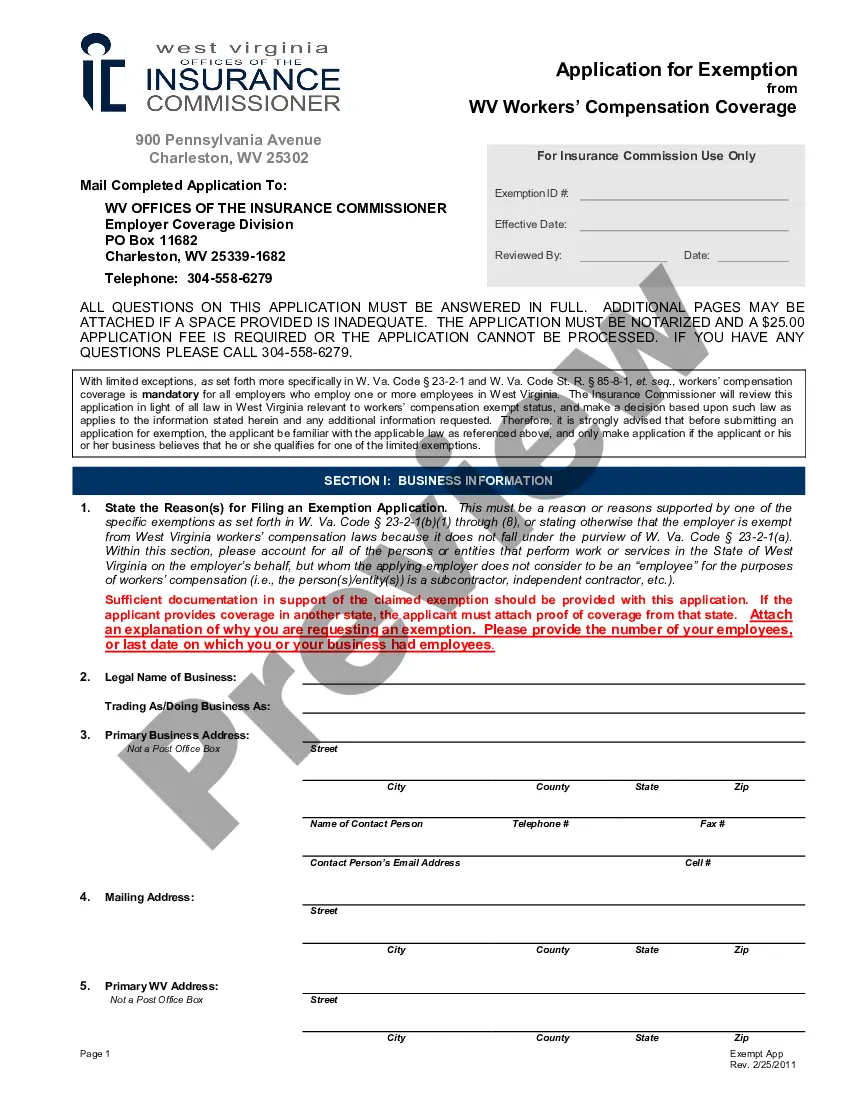
Official Workers' Compensation form in pdf format.
Nashville Tennessee Utilization Review Notification for Workers' Compensation is a vital process in the state of Tennessee to ensure fair and efficient utilization of medical treatments for injured employees. The utilization review is a systematic review of medical necessity, appropriateness, and efficiency of medical treatments for workers' compensation cases in Nashville, Tennessee. This process helps workers' compensation insurance providers determine if certain medical treatments are necessary, reasonable, and aligned with the official treatment guidelines. The utilization review notification in Nashville, Tennessee involves notifying all parties involved in the workers' compensation case about the review process. This includes the injured worker, their healthcare provider, the employer, and the insurance carrier. The notification ensures transparency and allows adequate time for all parties to provide relevant medical records, reports, documents, or testimony to support their perspective. The Nashville Tennessee Utilization Review Notification for Workers' Compensation aims to prevent unnecessary or inappropriate medical treatments while facilitating timely and effective care for injured workers. It helps in avoiding excessive financial burdens and ensures that resources are appropriately allocated. There are several types of Nashville Tennessee Utilization Review Notification for Workers' Compensation, including: 1. Initial notification: This is the first notification sent to all parties involved in the case, informing them about the utilization review process and their rights and responsibilities. 2. Request for medical records: In some cases, the utilization review process may require additional medical records or reports to make an accurate determination. This notification requests and provides a deadline for the submission of these records. 3. Final determination notification: Once the utilization review process is complete, a final determination notification is issued to inform all parties of the decision. This notification will outline the approved medical treatments or any modifications to the original treatment plan. 4. Appeal notification: If any party disagrees with the utilization review decision, they have the option to appeal. The appeal notification is sent to inform the relevant parties about the appeal process and the necessary steps to initiate an appeal. Overall, the Nashville Tennessee Utilization Review Notification for Workers' Compensation plays a crucial role in ensuring appropriate utilization of medical treatments and fostering efficient communication among all parties involved. It promotes fair resolutions, timely care, and cost-effectiveness in the workers' compensation system.