Westminster Colorado Request for Utilization Review for Workers' Compensation is a formal process that allows employers or insurance carriers to seek a review of medical treatment plans or services being provided to an injured worker. This request ensures that the treatment being received is necessary, appropriate, and in line with the established medical guidelines for workers' compensation cases in Colorado. The primary purpose of the Utilization Review (UR) process is to evaluate the medical necessity and cost-effectiveness of the suggested treatment plan or medical services. This review helps to determine if the treatment aligns with the current best practices and guidelines for managing the injured worker's condition. The process aims to prevent unnecessary or excessive medical treatment that might delay the worker's recovery or inflate the cost of the claim. Submitting a Westminster Colorado Request for Utilization Review for Workers' Compensation involves compiling relevant medical documents, such as medical reports, treatment plans, and any supporting evidence. These documents outline the current treatment being provided to the injured worker. There are a few different types of Westminster Colorado Request for Utilization Review for Workers' Compensation, depending on the specific scenario: 1. Initial Treatment Request: This type of request is typically submitted at the beginning of the treatment process. It involves seeking review and approval for the initial treatment plan proposed by the medical provider. The goal is to ensure that the suggested treatments are necessary and appropriate for the worker's injury. 2. Treatment Modification Request: Sometimes, there is a need to modify or adjust the treatment plan during the worker's recovery process. This type of request seeks to review and approve changes made to the existing treatment plan, such as medication adjustments, therapy changes, or surgical interventions. 3. Treatment Continuation Request: In cases where the injured worker has been receiving ongoing treatment, a request for continuation review is filed. This request aims to review the necessity and effectiveness of the current treatment plan. It ensures that the treatments being provided are helping the injured worker improve their condition and are aligned with the best medical practices. By filing a Westminster Colorado Request for Utilization Review for Workers' Compensation, employers and insurance carriers can ensure that the proper care is being provided to injured workers while minimizing unnecessary medical expenses. This process helps maintain a balance between the injured worker's well-being and the cost management of workers' compensation claims.
Westminster Colorado Request for Utilization Review for Workers' Compensation
Description
How to fill out Westminster Colorado Request For Utilization Review For Workers' Compensation?
If you’ve already used our service before, log in to your account and save the Westminster Colorado Request for Utilization Review for Workers' Compensation on your device by clicking the Download button. Make certain your subscription is valid. Otherwise, renew it according to your payment plan.
If this is your first experience with our service, adhere to these simple steps to obtain your document:
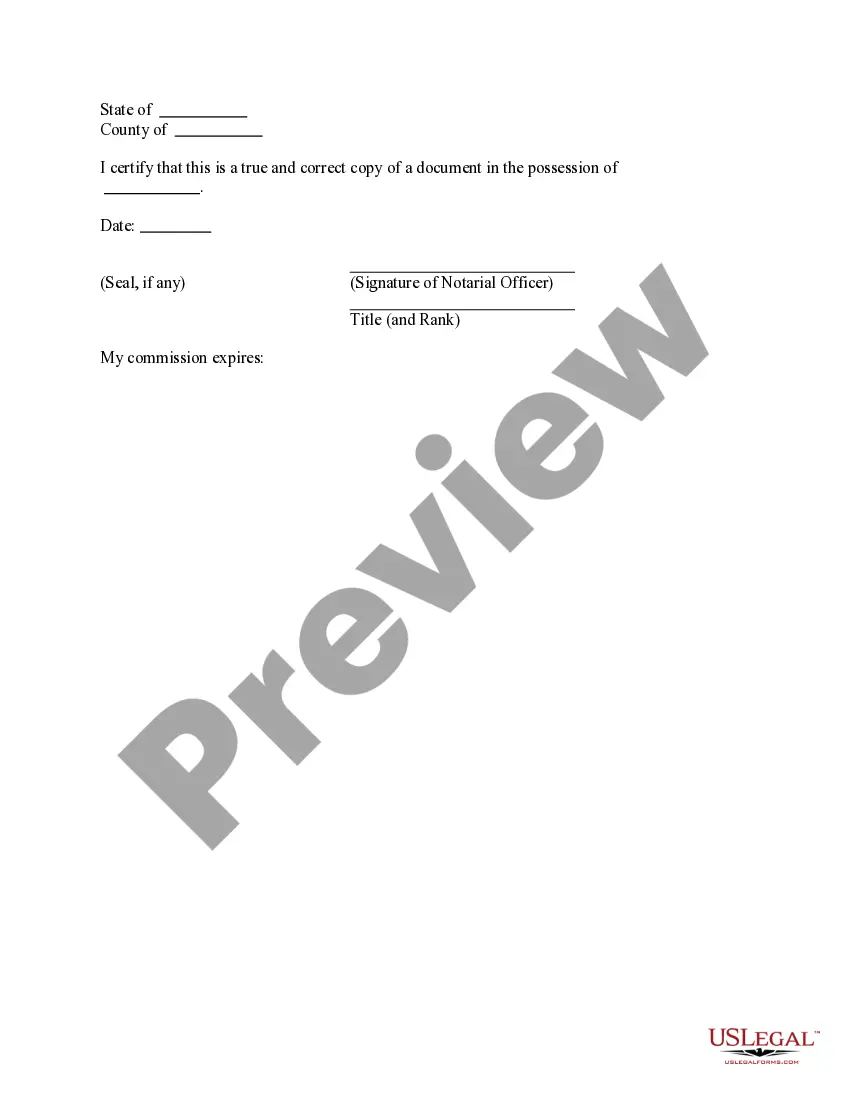
- Make sure you’ve found a suitable document. Read the description and use the Preview option, if any, to check if it meets your needs. If it doesn’t fit you, use the Search tab above to obtain the appropriate one.
- Buy the template. Click the Buy Now button and select a monthly or annual subscription plan.
- Register an account and make a payment. Use your credit card details or the PayPal option to complete the purchase.
- Obtain your Westminster Colorado Request for Utilization Review for Workers' Compensation. Select the file format for your document and save it to your device.
- Complete your sample. Print it out or take advantage of professional online editors to fill it out and sign it electronically.
You have constant access to every piece of paperwork you have bought: you can find it in your profile within the My Forms menu anytime you need to reuse it again. Take advantage of the US Legal Forms service to quickly locate and save any template for your individual or professional needs!
Form popularity
FAQ
The claims administrator must do the review and make a decision within five days of the date your doctor requested the treatment. If additional information is needed to make a decision, the claims administrator can have up to 14 days. Q.
(o) A utilization review decision to modify, delay, or deny a request for authorization of medical treatment shall remain effective for 12 months from the date of the decision without further action by the claims administrator with regard to any further recommendation by the same physician for the same treatment unless
An RFA is a form that the doctor is required to use to request treatment, diagnostic tests or other medical services for an injured worker. If the treatment request was first made verbally, it must be confirmed in writing.
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.
1 defines Request for Authorization as a written request for a specific course of proposed medical treatment. An RFA must meet both of the following criteria: Only for medical treatment and. Must be written.
Utilization review (UR) is the process used by employers or claims administrators to review treatment to determine if it is medically necessary. All employers or their workers' compensation claims administrators are required by law to have a UR program.
(o) A utilization review decision to modify, delay, or deny a request for authorization of medical treatment shall remain effective for 12 months from the date of the decision without further action by the claims administrator with regard to any further recommendation by the same physician for the same treatment unless
A UR program allows an employer or insurance company to review a treatment request made by an injured worker's physician to determine if the treatment is medically necessary. Following this review, the treatment request can be approved, denied, or modified.
Date of ?Receipt? of DWC Form RFA: According to California Code of Regulations, section 9792.9. 1 and Labor Code section 4610(g)(1), Utilization Review has five (5) business days to issue a decision.