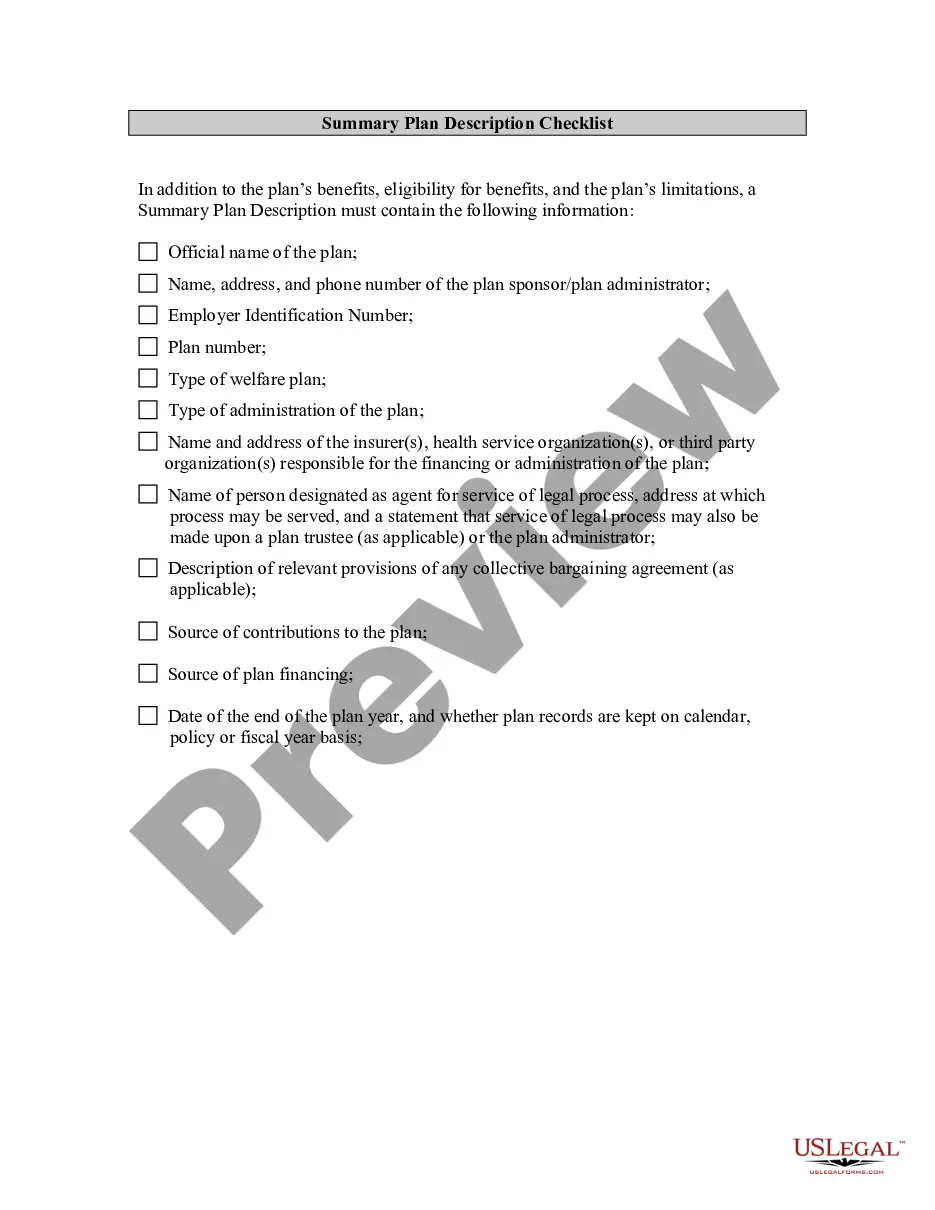
West Virginia Employee Benefit Plan Document Checklist
Description
How to fill out Employee Benefit Plan Document Checklist?
Finding the appropriate authorized document template can be challenging.
Clearly, there are numerous templates accessible online, but how do you locate the legal form you require.
Utilize the US Legal Forms website. The service provides thousands of templates, including the West Virginia Employee Benefit Plan Document Checklist, which can be utilized for both business and personal purposes.
You can review the form using the Review option and examine the form description to confirm it is correct for your needs.
- All forms are verified by professionals and comply with federal and state regulations.
- If you are already a registered user, Log In to your account and select the Download button to receive the West Virginia Employee Benefit Plan Document Checklist.
- Use your account to browse through the legal forms you have previously purchased.
- Go to the My documents section of your account and obtain another copy of the document you require.
- If you are a new customer of US Legal Forms, follow these simple instructions.
- First, verify that you have selected the correct form for your city/region.
Form popularity
FAQ
United Medical Resources, subsidiary and third party administrator for United Healthcare Services Incorporated, a medical insurance provider.
Applicability of this supplement. UMR is a wholly owned subsidiary of UnitedHealthcare, a part of UnitedHealth Group. UMR is a third-party administrator (TPA) and not an insurance company. UMR delivers solutions for self-funded employer groups to ensure claims are paid correctly according to the member's benefit plan.
UMR is the Claims Administrator for the Medicare Secondary Plan. For more information about this plan, contact UMR Member Services at 1-877-561-0366 or go online to .
After a national search, PEIA has selected UMR, a UnitedHealthcare (UHC) company, as our new third- party administrator (TPA), a move which will generate an estimated $9.2 million in first-year savings. UMR is the nation's largest TPA, servicing 2,800 customers and 4.5 million members.
Preferred Provider Benefit (PPB) Plan A has higher premiums but lower deductibles. PPB Plan B has lower premiums but higher deductibles.
PEIA PPB Plan A is PEIA's most popular plan. PEIA PPB Plan B is similar to the standard PPB Plan A, but offers lower premiums with higher deductibles, higher out-of-pocket maximums, a greater coinsurance requirement, and higher copayments for prescription drugs. The medical coverage is the same as in PPB Plan A.
As a UnitedHealthcare company, UMR has long been a pioneer in revolutionizing self-funding. We focus on delivering customer solutions that meet their goals and strategies.
UMR is PEIA's third-party administrator that handles medical claim processing, case management, utilization management, precertification, prior approval and customer service for the PEIA PPB Plans. Contact UMR for answers to questions about eligibility, benefits and networks.
PEIA's third-party administrator (TPA) transition from HealthSmart to UMR continues to move smoothly. UMR will take over as TPA for the PPB Plans and the Special Medicare Plan beginning July 1, 2019. PEIA will be serviced from the UMR Customer Service Center in downtown Charleston.