Washington Summary of Rights and Obligations under COBRA
Description
How to fill out Summary Of Rights And Obligations Under COBRA?
US Legal Forms - one of the largest collections of legal documents in the USA - provides a range of legal form templates that you can obtain or print.
By utilizing the website, you can access numerous forms for business and personal purposes, organized by categories, claims, or keywords.
You will find the latest varieties of forms such as the Washington Summary of Rights and Obligations under COBRA within moments.
Review the form's description to confirm you have chosen the correct template.
If the form does not meet your requirements, utilize the Search box at the top of the page to find one that does.
- If you already have a monthly subscription, Log In and obtain the Washington Summary of Rights and Obligations under COBRA from the US Legal Forms collection.
- The Download button will appear on each template you view.
- You can access all previously downloaded templates in the My documents section of your account.
- If you are looking to use US Legal Forms for the first time, here are some simple instructions to assist you in getting started.
- Ensure you have selected the correct form for your area/location.
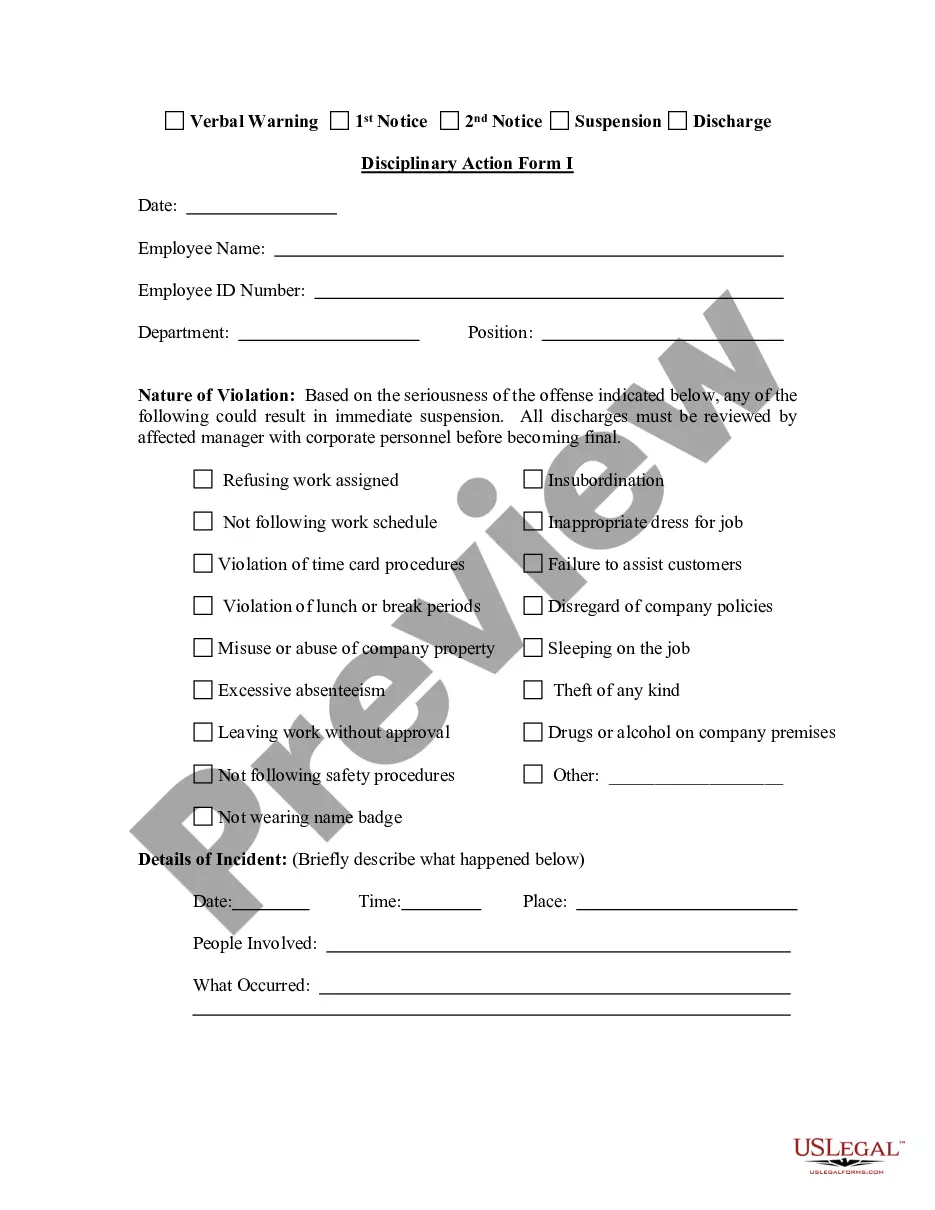
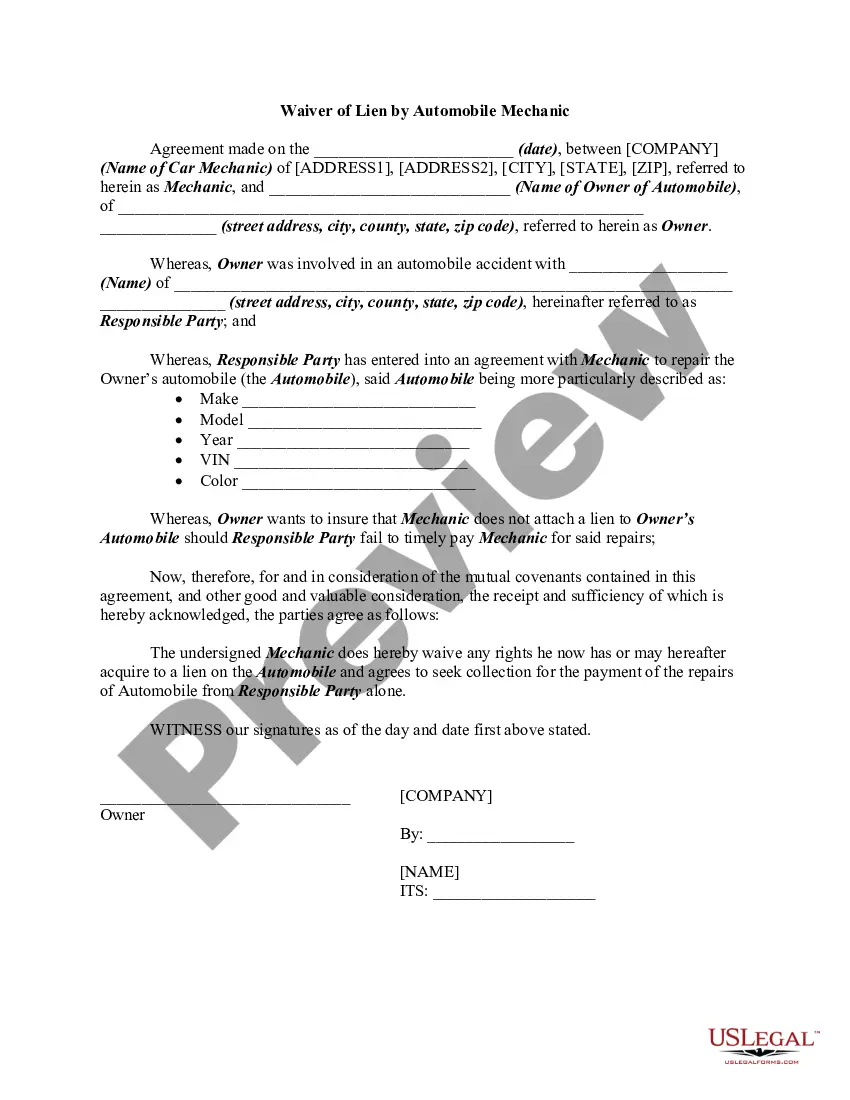
- Click on the Preview button to review the content of the form.
Form popularity
FAQ
In Washington, COBRA coverage typically lasts for 18 months, but it can extend to 36 months for certain qualifying events. This duration provides individuals with essential time to secure new employment or alternative health insurance. Understanding the Washington Summary of Rights and Obligations under COBRA helps you stay informed about your options. If you have further questions about your coverage timeline, USLegalForms offers comprehensive resources to assist you.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
Eligibility. You're eligible to continue your health coverage for up to 18 months if either of these occur: Your employment ends (unless it's due to gross misconduct)
Even if you enroll in COBRA on the last day that you are eligible, your coverage is retroactive to the date you lost your employer-sponsored health plan.
Eligibility. You're eligible to continue your health coverage for up to 18 months if either of these occur: Your employment ends (unless it's due to gross misconduct)
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a federal law passed in 1986 that lets certain employees, their spouses, and their dependents keep group health plan (GHP) coverage for 18 to 36 months after they leave their job or lose coverage for certain other reasons, as long as they pay the full cost
Key takeaway: Employers with 20 or more full-time employees must provide COBRA coverage. Employers with fewer than 20 employees are typically subject to state laws.
COBRA applies only to employers who had 20 or more workers in the previous year. State and local governments fall under COBRA, but federal plans and certain religious organizations do not. Federal employees have some similar rights under another law. Ask your human resource department for more information.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
For disabled QBs who receive an 11-month COBRA extension (29 months in total), you can charge up to 150% of the group rate. Many states have regulations that are similar to federal COBRA. These state regulations are known as mini-COBRA.