Tennessee General Notice of Preexisting Condition Exclusion
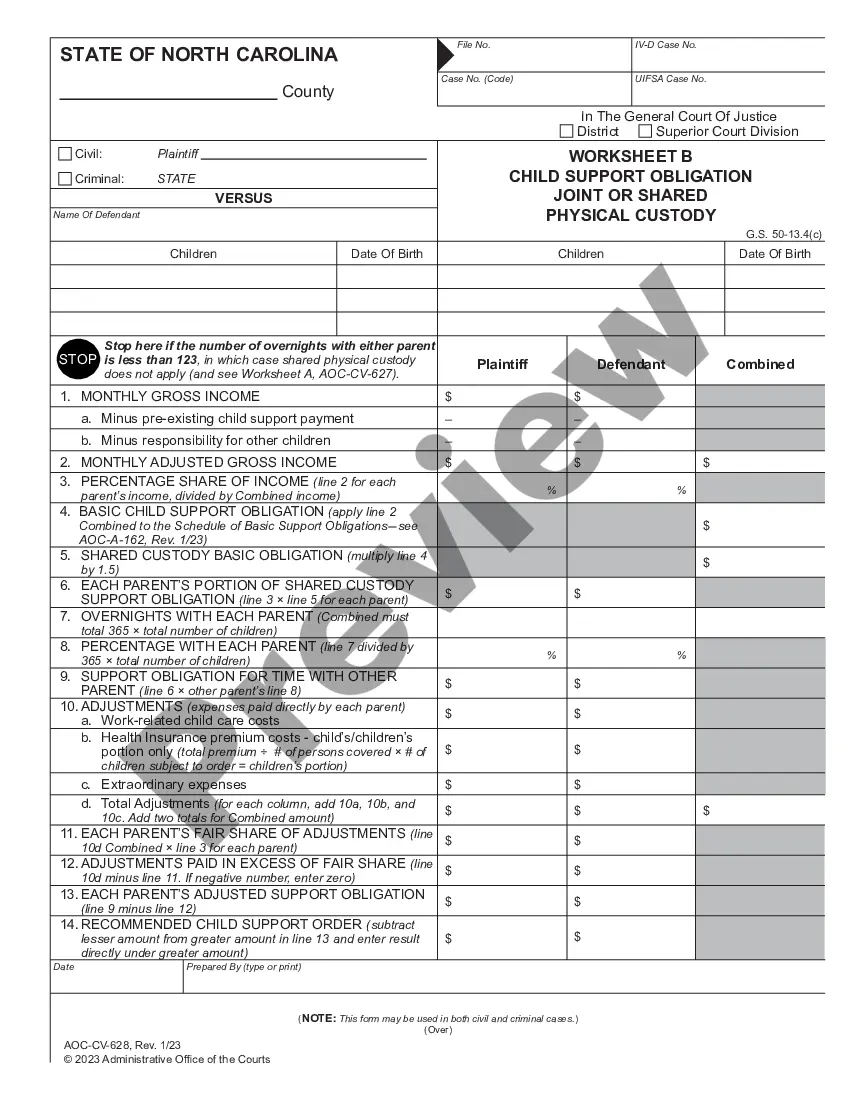
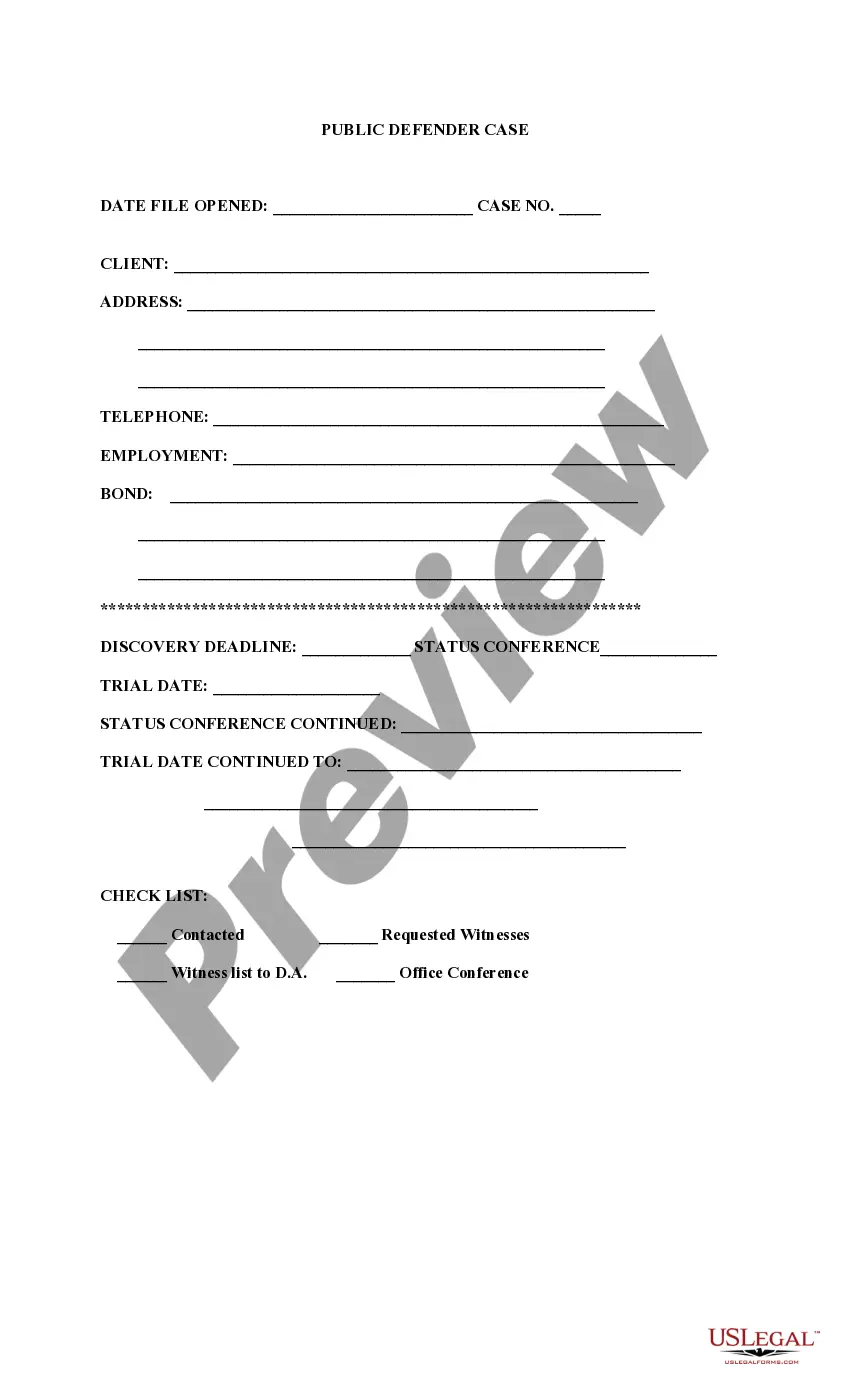
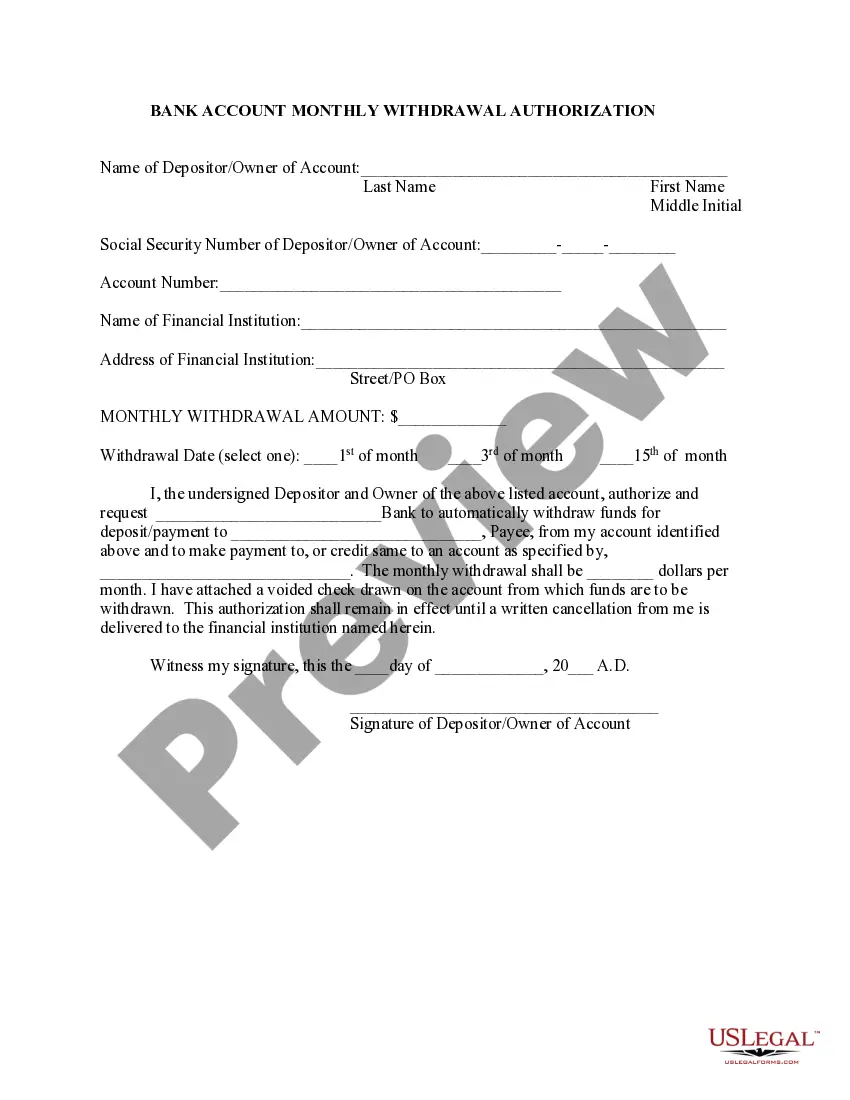
Description
How to fill out General Notice Of Preexisting Condition Exclusion?
Finding the right legal document format can be quite challenging.
Clearly, there are numerous templates accessible online, but how do you find the legal form you require.
Utilize the US Legal Forms website.
Firstly, ensure you have selected the correct form for your city/state. You can browse the template using the Review button and examine the form's description to verify it suits your needs.
- The platform provides a vast array of templates, including the Tennessee General Notice of Preexisting Condition Exclusion, which you can utilize for both business and personal purposes.
- All of the forms are vetted by experts and comply with state and federal regulations.
- If you are already registered, Log In to your account and click the Acquire button to obtain the Tennessee General Notice of Preexisting Condition Exclusion.
- Use your account to review the legal forms you have previously acquired.
- Navigate to the My documents section of your account and download another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple steps for you to follow.
Form popularity
FAQ
existing condition exclusion can not be longer than 12 months from your enrollment date (18 months for a late enrollee). existing condition exclusion that is applied to you must be reduced by the prior creditable coverage you have that was not interrupted by a significant break in coverage.
Health insurance companies cannot refuse coverage or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
A late enrollee may be excluded from coverage for up to 12 months or may have a preexisting condition limitation apply for up to 12 months; however, in no case shall a late enrollee be excluded from some or all coverage for more than 12 months.
Provides comprehensive coverage modeled on the state employee health plan. There are no pre-existing condition clauses. Not a Medicaid program.
You can still get health insurance cover if you have pre-existing medical conditions, but it is unlikely your policy will provide cover for them. The type of underwriting of your health plan determines whether your pre-existing conditions will be covered in the future.
If you had a pre-existing condition exclusion period, you didn't have coverage for any care or services related to your pre-existing condition for a predetermined amount of time, despite paying your monthly premiums.
Protecting privately insured consumers with preexisting conditions means ensuring that those with health conditions are treated the same as those without health conditions in terms of access, affordability, and adequacy of coverage.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.