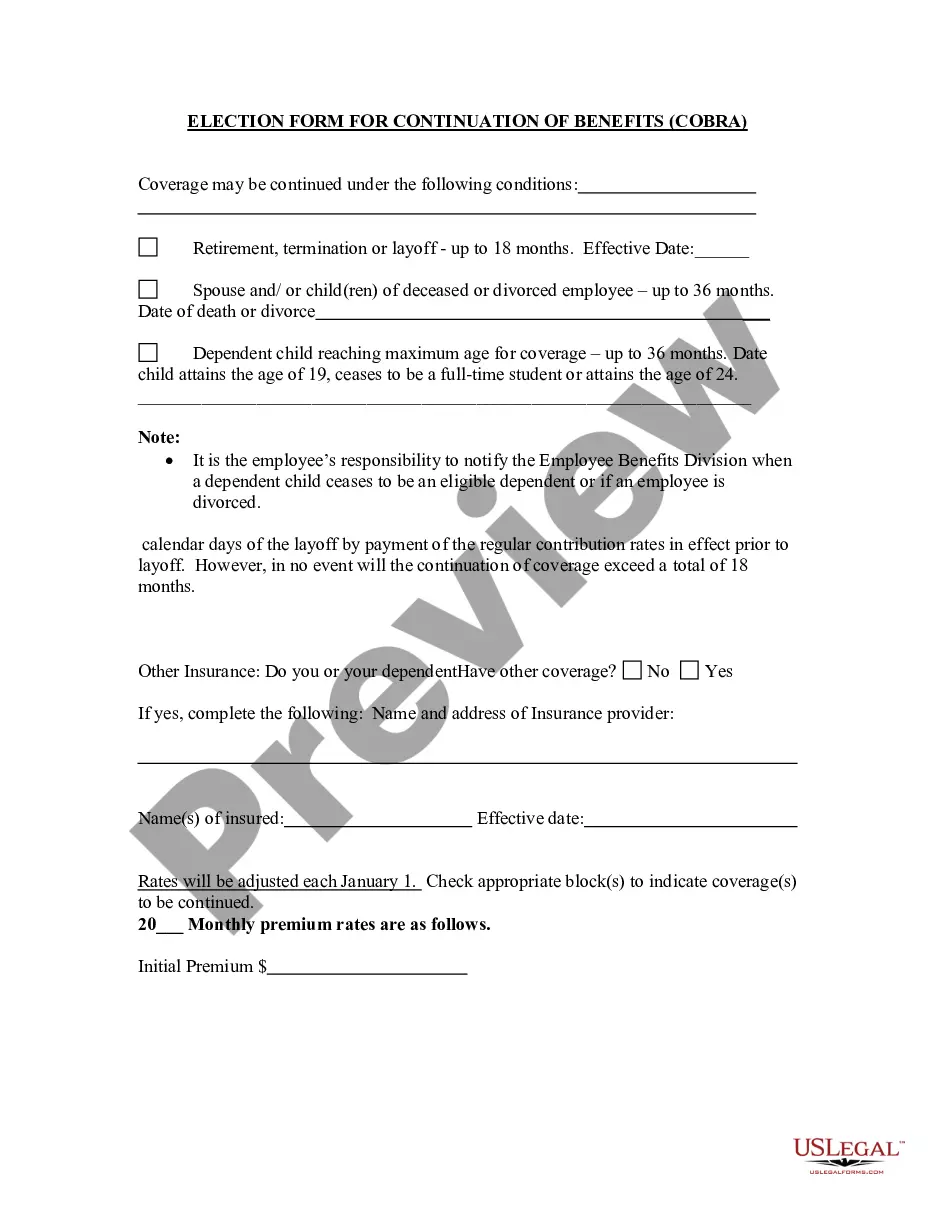
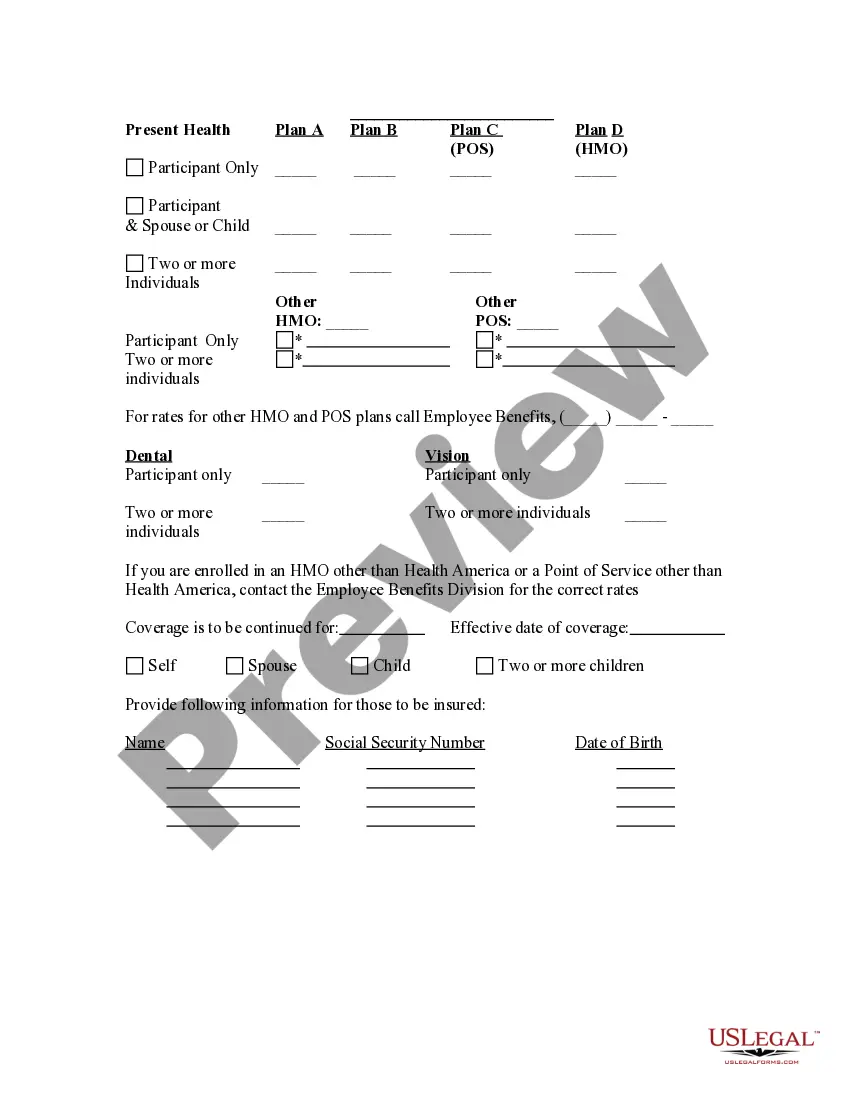
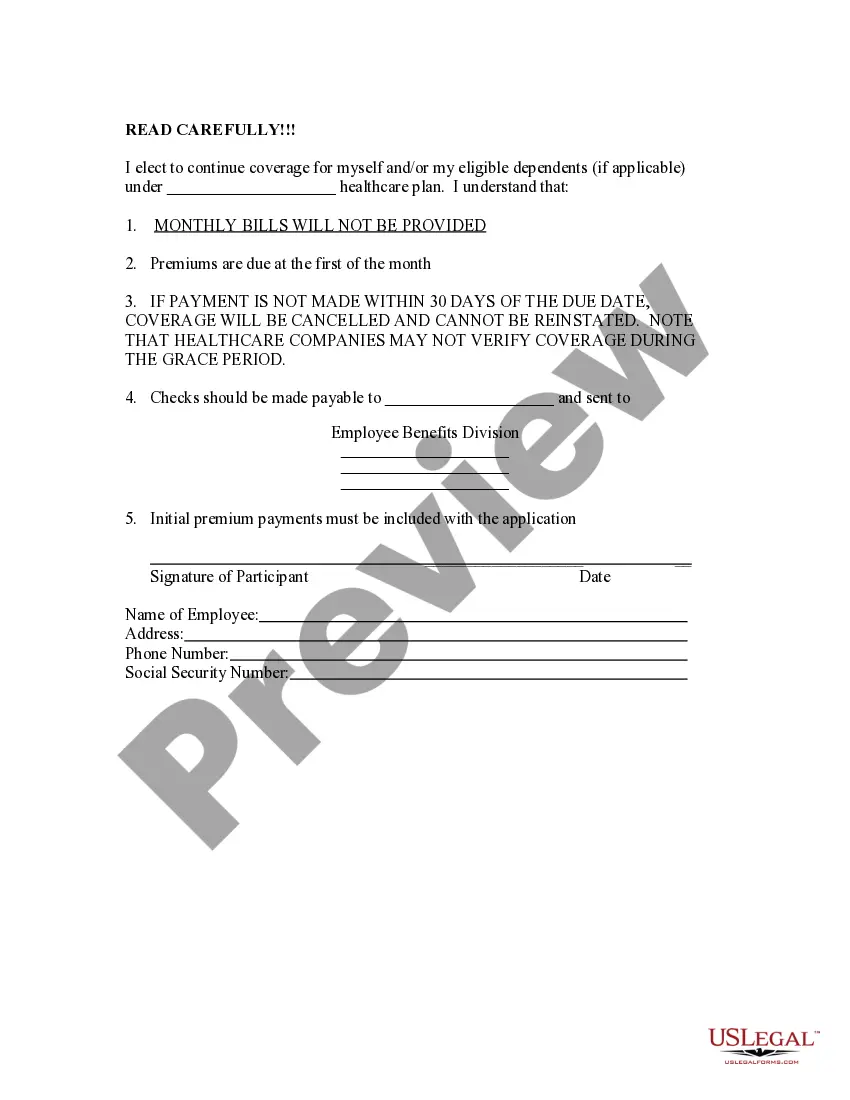
Tennessee Election Form for Continuation of Benefits - COBRA
Description
How to fill out Election Form For Continuation Of Benefits - COBRA?
If you need to thorough, acquire, or print valid document templates, utilize US Legal Forms, the largest collection of legal forms, which are available online.
Employ the site's straightforward and user-friendly search to locate the documents you require. A range of templates for business and personal purposes are categorized by regions and states, or keywords.
Utilize US Legal Forms to obtain the Tennessee Election Form for Continuation of Benefits - COBRA within just a few clicks.
Every legal document template you obtain is yours indefinitely. You can access every form you saved in your account. Go to the My documents section and select a form to print or download again.
Act swiftly and download, and print the Tennessee Election Form for Continuation of Benefits - COBRA with US Legal Forms. There are thousands of professional and state-specific forms available for your business or personal needs.
- If you are already a US Legal Forms user, Log In to your account and click the Download button to find the Tennessee Election Form for Continuation of Benefits - COBRA.
- You can also access forms you previously saved in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the instructions below.
- Step 1. Ensure you have selected the form for the correct state/land.
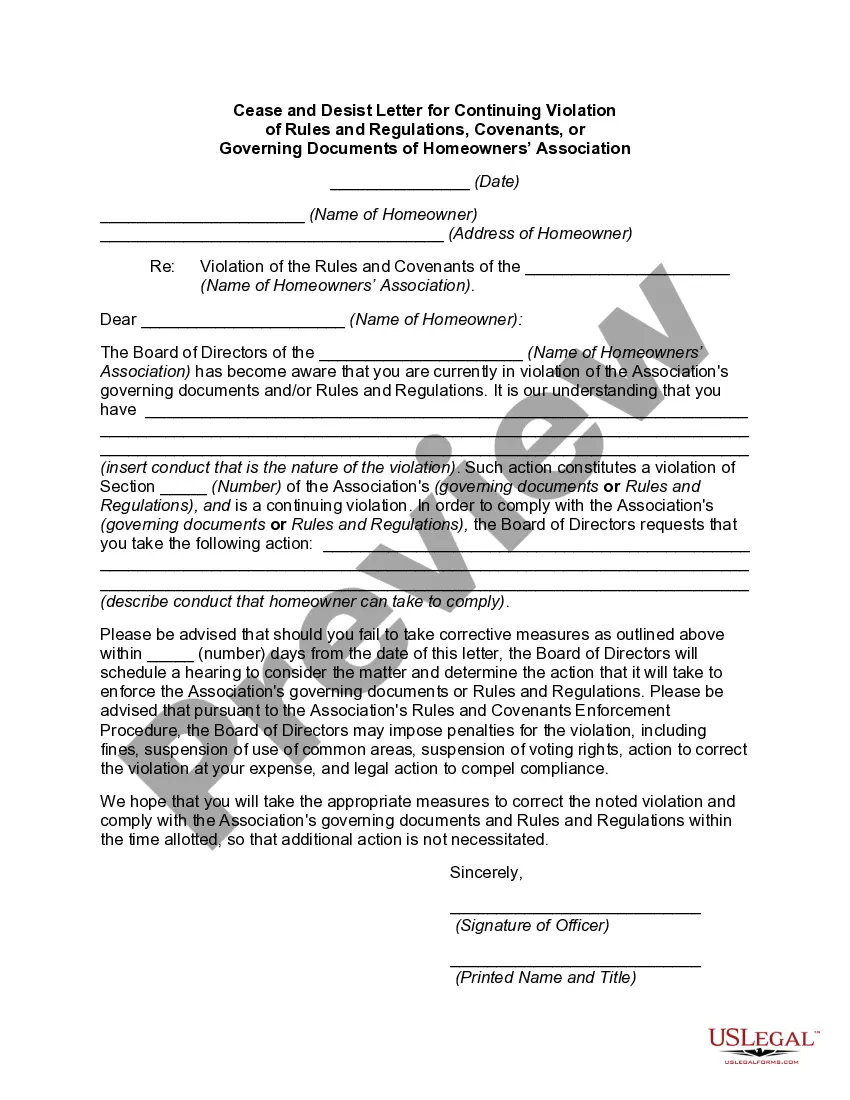
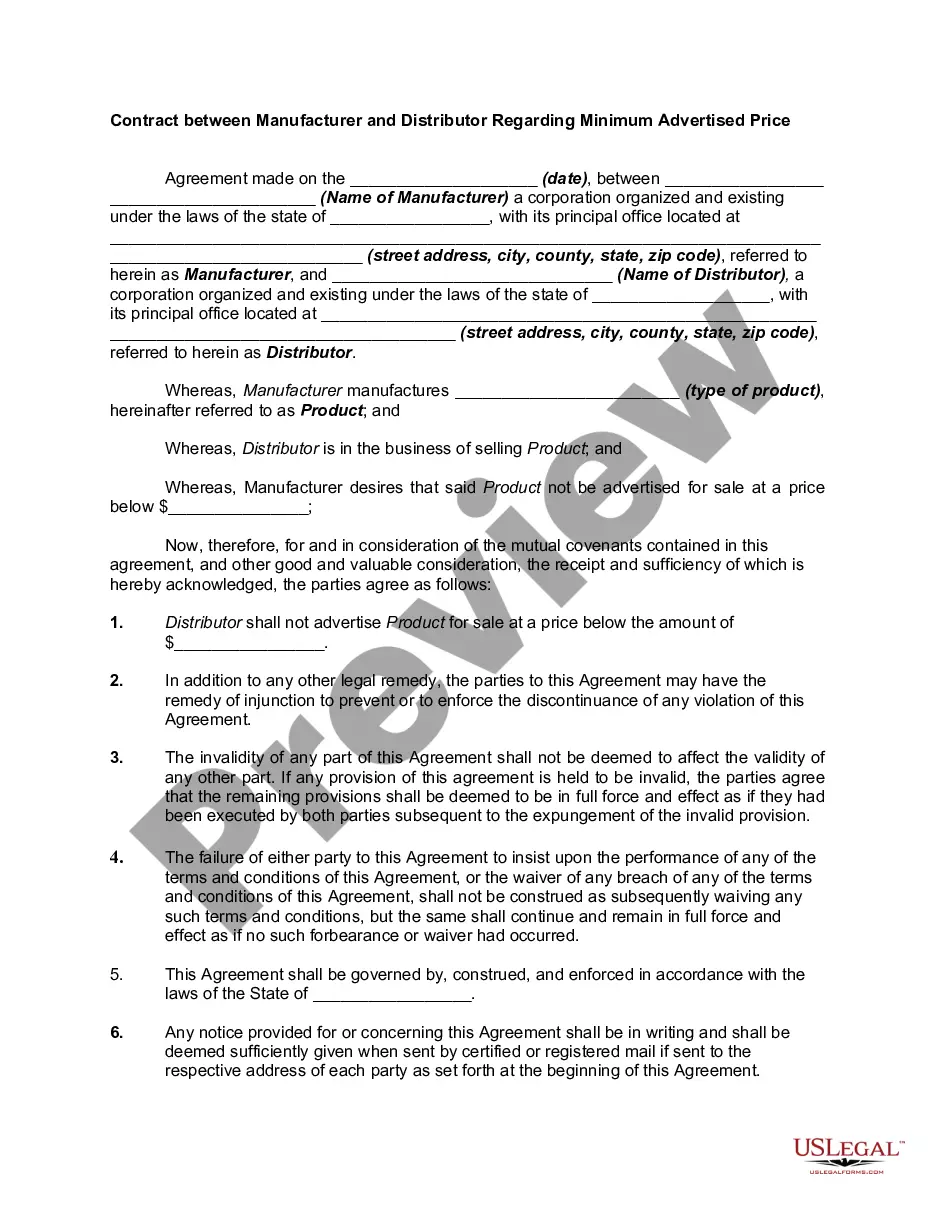
- Step 2. Use the Preview option to review the form's details. Remember to read the description.
- Step 3. If you are not satisfied with the form, utilize the Search field at the top of the screen to find other versions of the legal form template.
- Step 4. Once you have found the form you need, click the Download now button. Choose the payment plan you prefer and provide your details to register for an account.
- Step 5. Complete the transaction. You can use your credit card or PayPal account to finalize the purchase.
- Step 6. Select the format of the legal form and download it to your system.
- Step 7. Fill out, modify, and print or sign the Tennessee Election Form for Continuation of Benefits - COBRA.
Form popularity
FAQ
Although the earlier rules only covered summary plan descriptions (SPDs) and summary annual reports, the final rules provide that all ERISA-required disclosure documents can be sent electronically -- this includes COBRA notices as well as certificates of creditable coverage under the Health Insurance Portability and
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
You can reach Covered California at (800) 300-1506 or online at . You can apply for individual coverage directly through some health plans off the exchange.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Tennessee - Coverage can be extended for the remainder of the month in which it would have terminated, plus up to three additional months. An individual who loses access to group coverage during pregnancy can continue their coverage for at least the duration of the pregnancy plus six months.
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.
How to Administer Cal-COBRANotifying all eligible group health care participants of their Cal-COBRA rights.Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.More items...