Pennsylvania COBRA Continuation Waiver Letter
Description
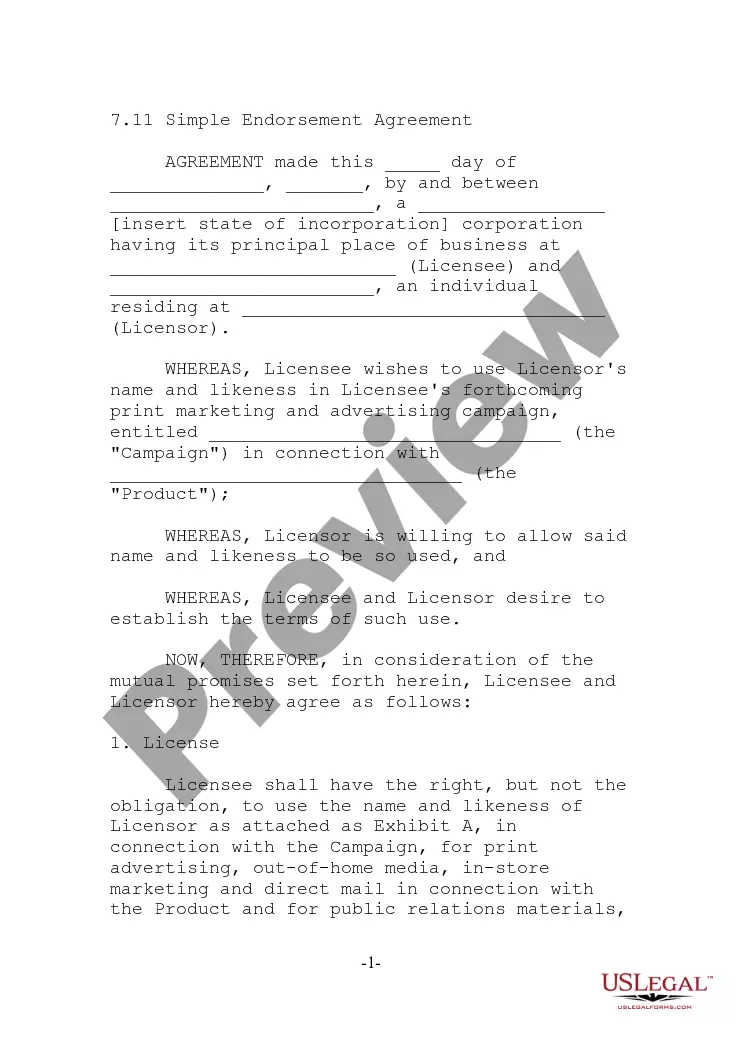
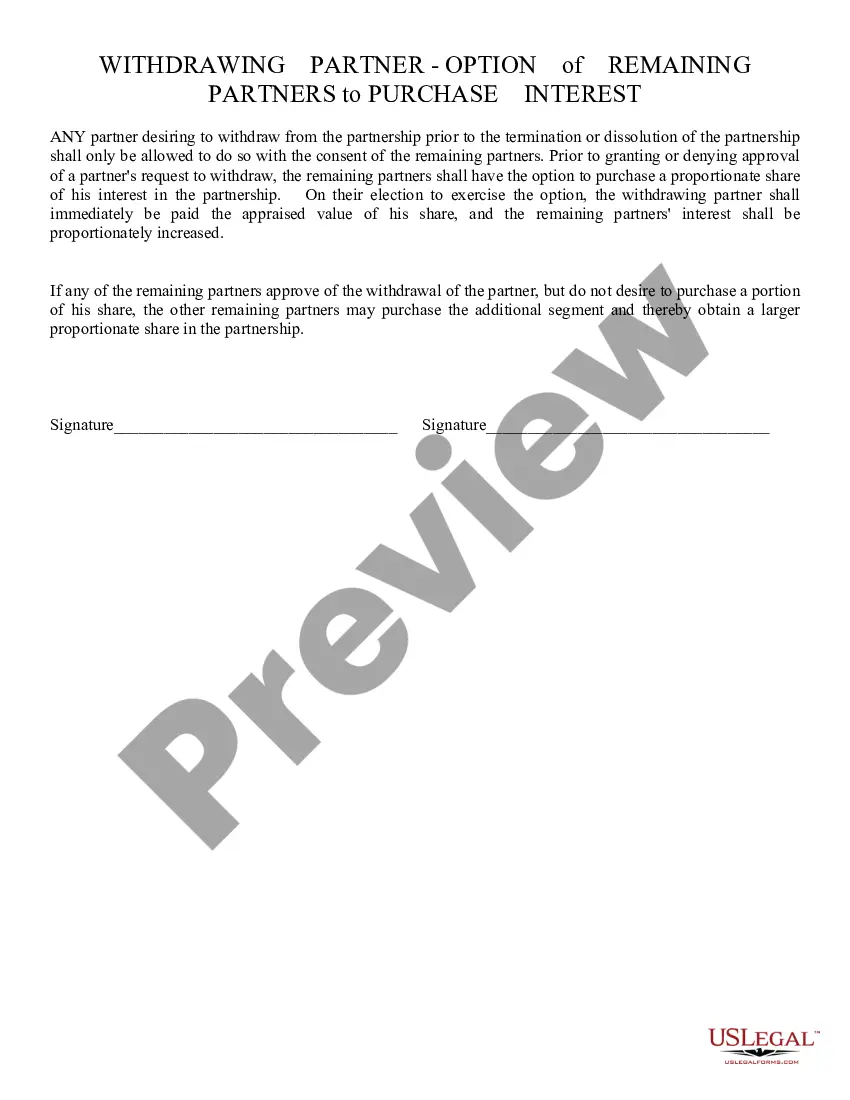
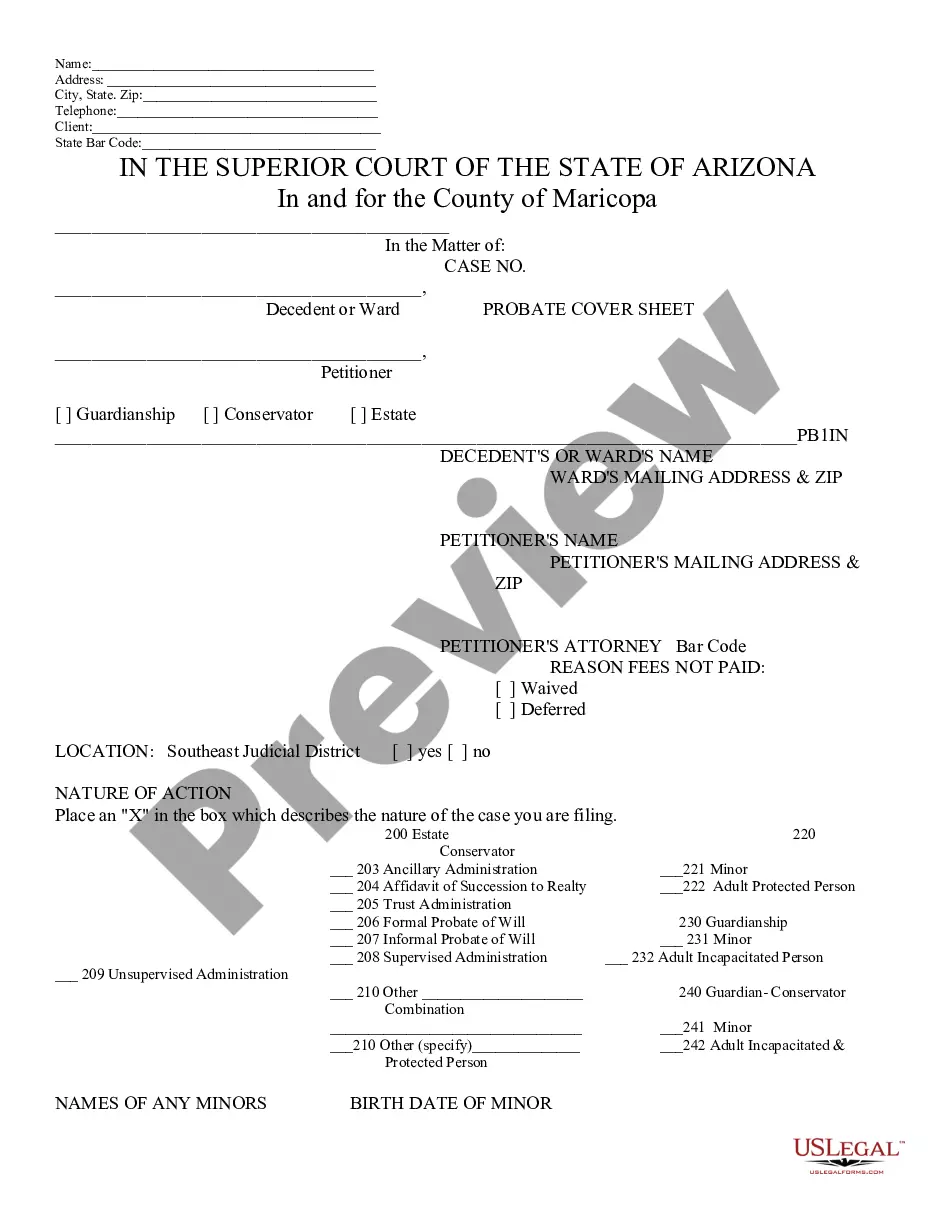
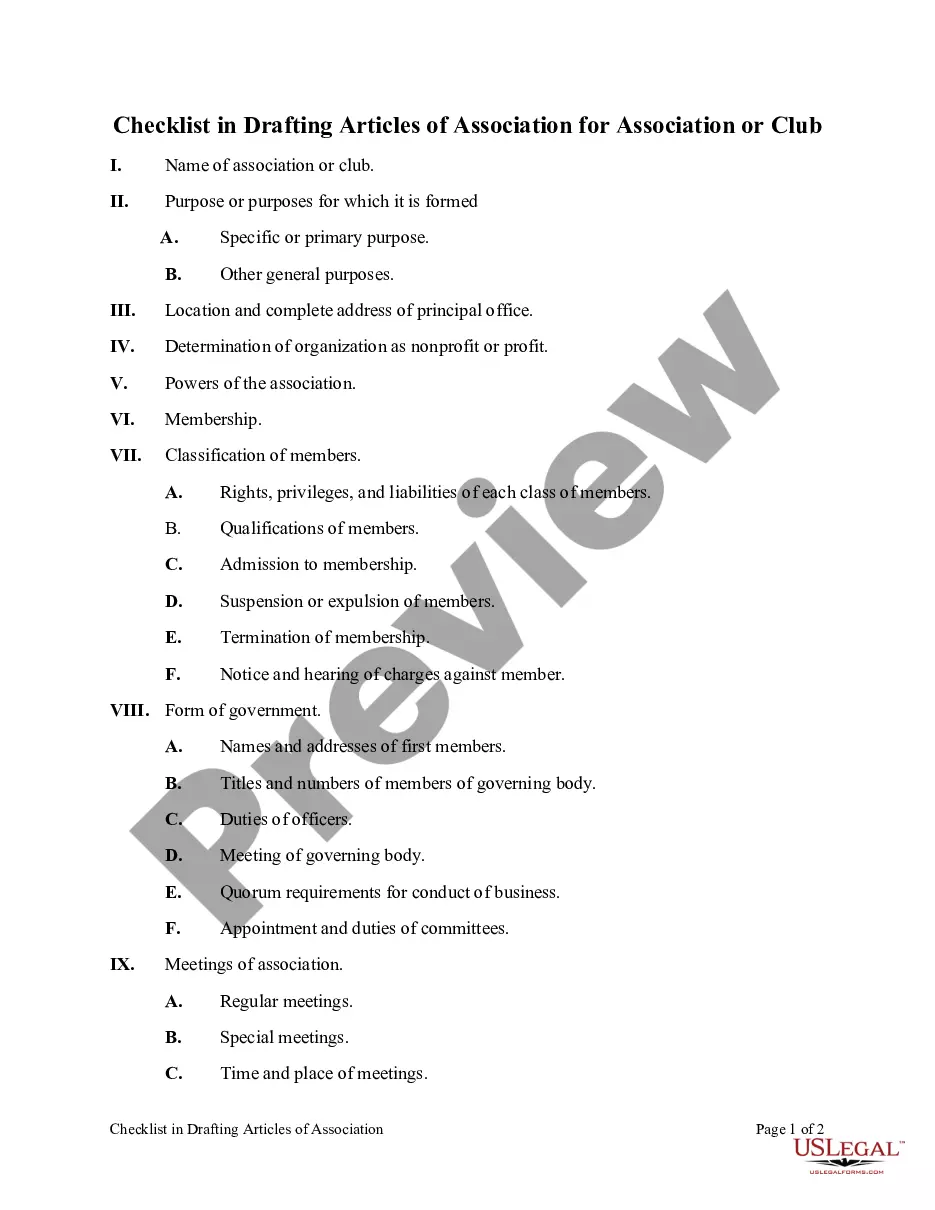
How to fill out COBRA Continuation Waiver Letter?
US Legal Forms - among the largest collections of legal forms in the country - offers a broad selection of legal document templates that you can download or create.
By using the website, you can access thousands of forms for business and personal purposes, categorized by types, states, or keywords. You can find the latest versions of forms such as the Pennsylvania COBRA Continuation Waiver Letter in a matter of minutes.
If you already have an account, Log In to download the Pennsylvania COBRA Continuation Waiver Letter from the US Legal Forms directory. The Download button will be visible on every form you view. You have access to all previously saved forms from the My documents section of your account.
Make modifications. Fill out, edit, print, and sign the downloaded Pennsylvania COBRA Continuation Waiver Letter.
Every template you added to your account has no expiration date and is yours permanently. Therefore, if you wish to download or print another copy, just go to the My documents section and click on the form you need.
- If you are using US Legal Forms for the first time, here are easy steps to get started.
- Ensure you have selected the correct form for your city/state. Click on the Preview button to review the form's details. Check the form summary to ensure you have chosen the right one.
- If the form does not meet your needs, utilize the Search field at the top of the page to find the one that does.
- If you are satisfied with the form, affirm your choice by clicking the Purchase now button. Then, select the payment plan you prefer and provide your information to create an account.
- Process the payment. Use a Visa or MasterCard or PayPal account to complete the transaction.
- Choose the format and download the form to your device.
Form popularity
FAQ
If you want to avoid paying the COBRA cost, go with a short-term plan if you're waiting for approval on another health plan. Choose a Marketplace or independent plan for broader coverage. Choose a high-deductible plan to keep your costs low.
Pennsylvania's Mini-COBRA applies to employees of smaller businesses (2-19 employees), though it only allows for 9 months of coverage.
You May Cancel COBRA At Any Time To cancel your your COBRA coverage you will need to notify your previous employer or the plan administrator in writing. After you stop your COBRA insurance, your former employer should send you a letter affirming termination of that health insurance.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Instead, Assistance Eligible Individuals do not have to pay any of the COBRA premium for the period of coverage from April 1, 2021 through September 30, 2021. The premium is reimbursed directly to the employer, plan administrator, or insurance company through a COBRA premium assistance credit.
COBRA costs an average of $599 per month. An Obamacare plan of similar quality costs $462 per monthbut 94% of people on HealthSherpa qualify for government subsidies, bringing the average cost down to $48 per month.
If you waive COBRA coverage during the election period, you must be permitted later to revoke your waiver of coverage and to elect continuation coverage as long as you do so during the election period. Then, the plan need only provide continuation coverage beginning on the date you revoke the waiver.
The federal COBRA law allows employees at larger businesses (20 or more employees) to purchase continuation health coverage after they leave employment for 18 months (or, in some cases, 36 months) after their employment ends.
COBRA Coverage PeriodsYou can cancel the COBRA coverage at any time within 18 months. You're not locked in. You will likely want to drop COBRA once you become eligible for a different health plan, such as if you get another job. If you stop paying premiums, COBRA coverage will end automatically.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.