Pennsylvania Model COBRA Continuation Coverage Election Notice
Description
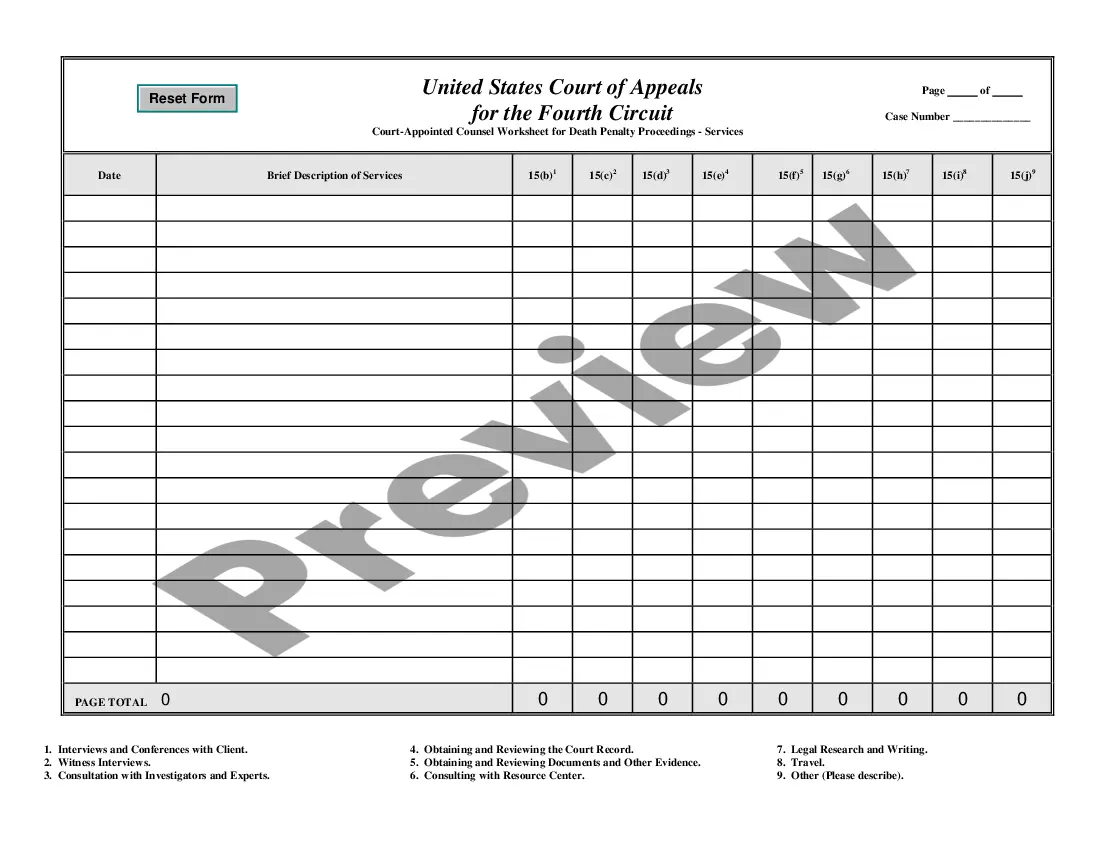
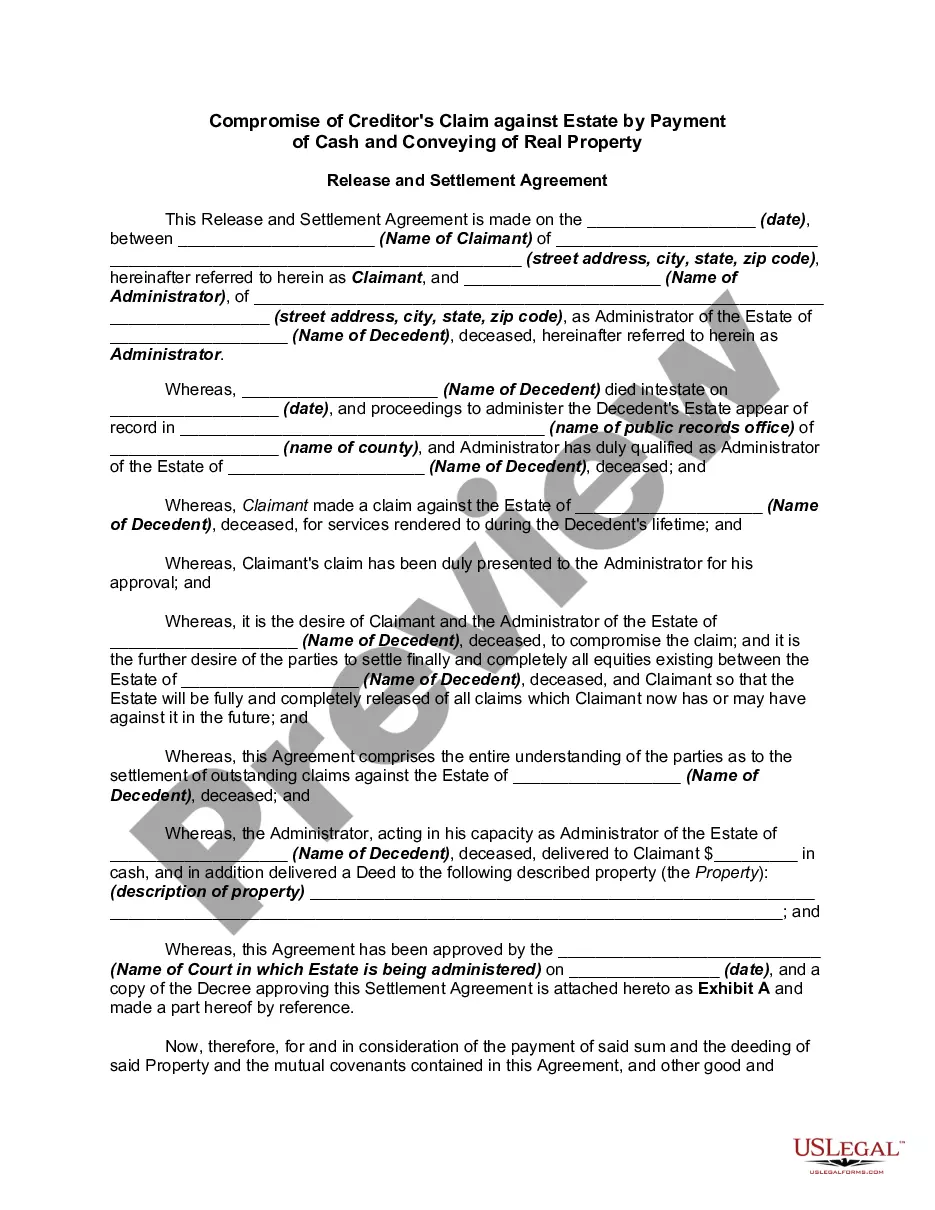
How to fill out Model COBRA Continuation Coverage Election Notice?
It is feasible to invest hours online searching for the legal document template that meets the state and federal requirements you desire.
US Legal Forms provides a vast array of legal documents that are evaluated by professionals.
You can obtain or print the Pennsylvania Model COBRA Continuation Coverage Election Notice from the service.
First, make sure you have selected the correct document template for the region/town of your choice. Review the document description to ensure you have selected the appropriate form. If available, utilize the Review button to look through the document template as well.
- If you already hold a US Legal Forms account, you can sign in and click the Download button.
- Subsequently, you can fill out, modify, print, or sign the Pennsylvania Model COBRA Continuation Coverage Election Notice.
- Each legal document template you acquire is yours permanently.
- To obtain another copy of any purchased document, navigate to the My documents tab and click the corresponding button.
- If this is your first time using the US Legal Forms website, follow the simple instructions below.
Form popularity
FAQ
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
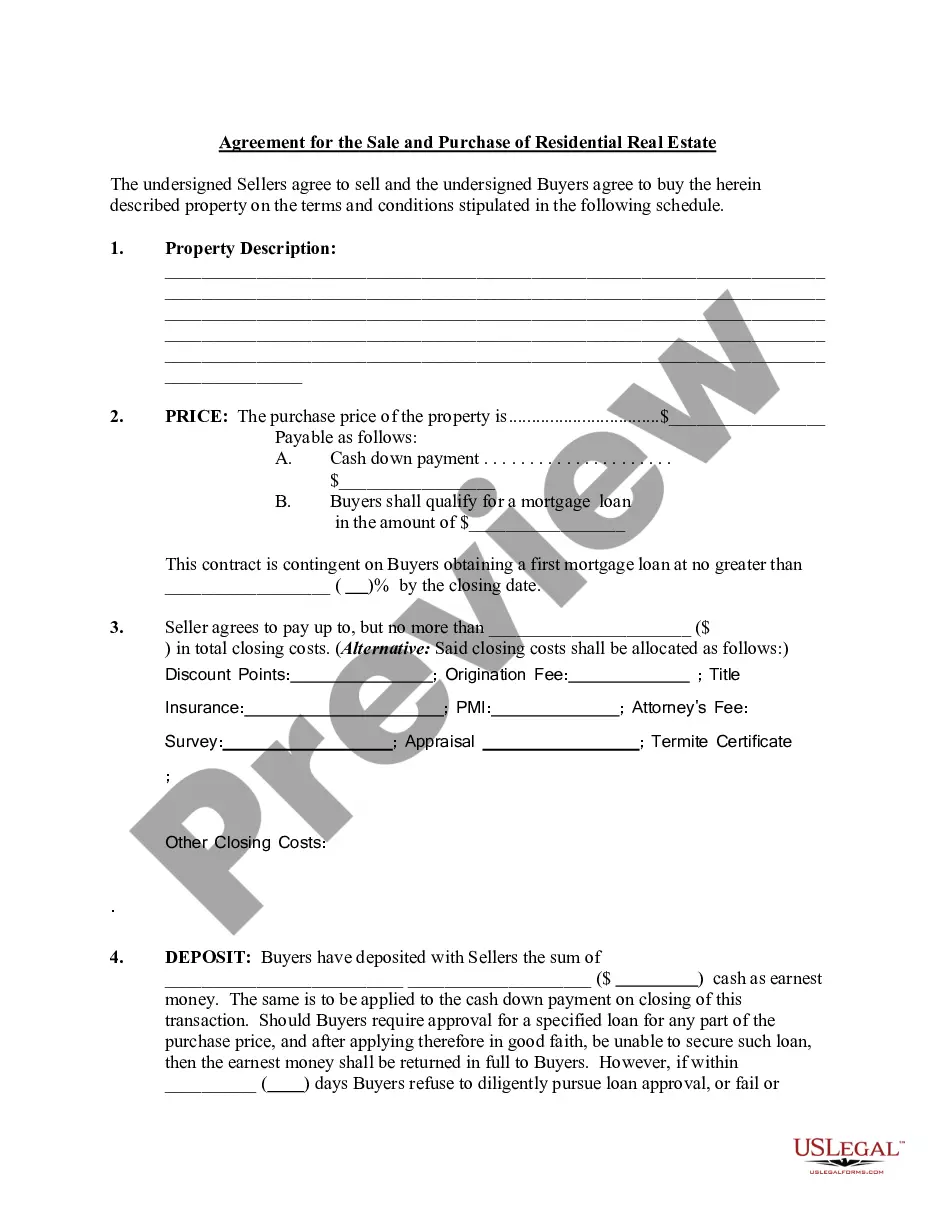
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
State continuation coverage refers to state laws that allow people to extend their employer-sponsored health insurance even if they're not eligible for extension via COBRA. As a federal law, COBRA applies nationwide, but only to employers with 20 or more employees.