Pennsylvania Sample COBRA Enrollment and / or Waiver Letter
Description
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
Locating the appropriate legal document template can be quite a challenge. Clearly, there is an abundance of templates available online, but how can you secure the legal document you require? Utilize the US Legal Forms website.
The service provides a wide variety of templates, including the Pennsylvania Sample COBRA Enrollment and/or Waiver Letter, which you can utilize for both business and personal purposes. All documents are vetted by professionals and comply with federal and state regulations.
If you are already registered, Log In to your account and click the Download button to access the Pennsylvania Sample COBRA Enrollment and/or Waiver Letter. Use your account to browse through the legal documents you have previously acquired. Visit the My documents section of your account to obtain another copy of the documents you need.
Fill out, amend, print, and sign the downloaded Pennsylvania Sample COBRA Enrollment and/or Waiver Letter. US Legal Forms is the largest repository of legal documents where you can find a variety of document templates. Utilize the service to obtain professionally-created paperwork that adheres to state requirements.
- If you are a new user of US Legal Forms, here are simple steps for you to follow.
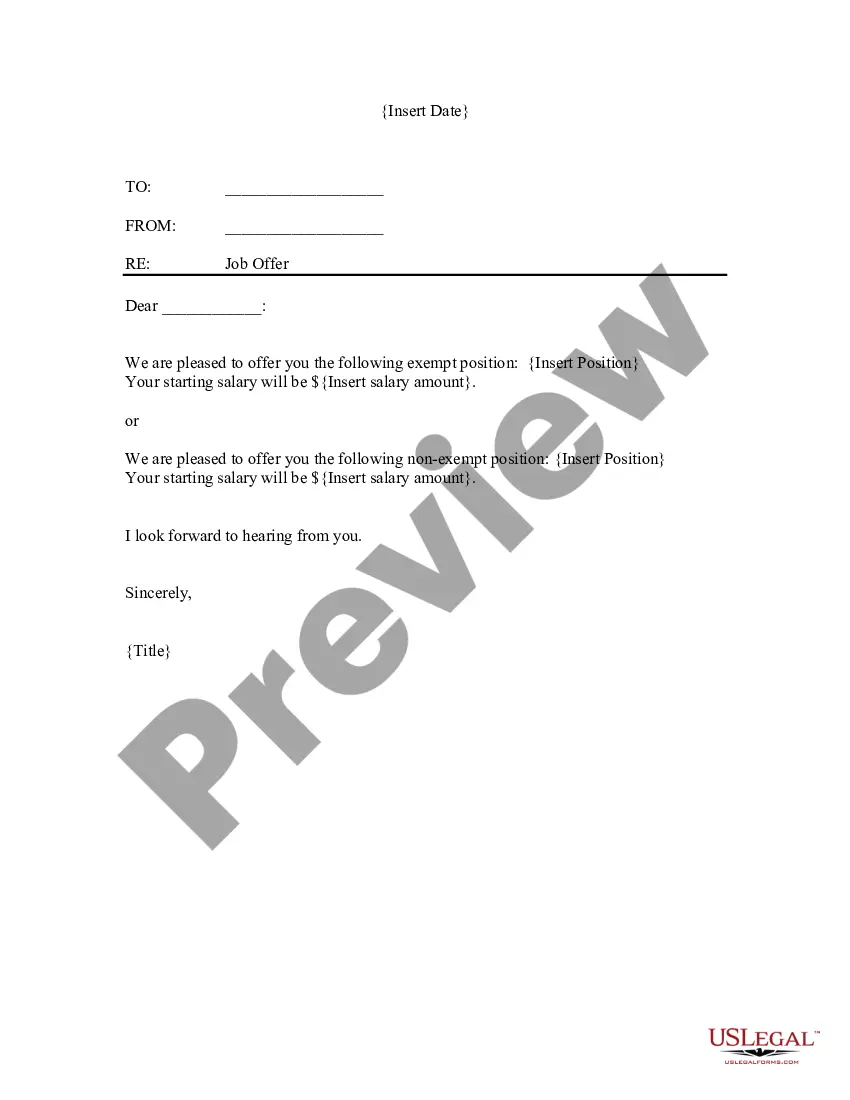
- First, ensure you have selected the correct document for your city/county. You can review the document using the Preview button and read the document description to confirm it is the suitable one for you.
- If the document does not meet your requirements, utilize the Search field to find the right document.
- When you are confident that the document is correct, click the Get now button to obtain the document.
- Choose the pricing plan you desire and enter the necessary information. Create your account and complete the purchase using your PayPal account or credit card.
- Select the file format and download the legal document template to your device.
Form popularity
FAQ
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
COBRA Coverage PeriodsYou can cancel the COBRA coverage at any time within 18 months. You're not locked in. You will likely want to drop COBRA once you become eligible for a different health plan, such as if you get another job. If you stop paying premiums, COBRA coverage will end automatically.
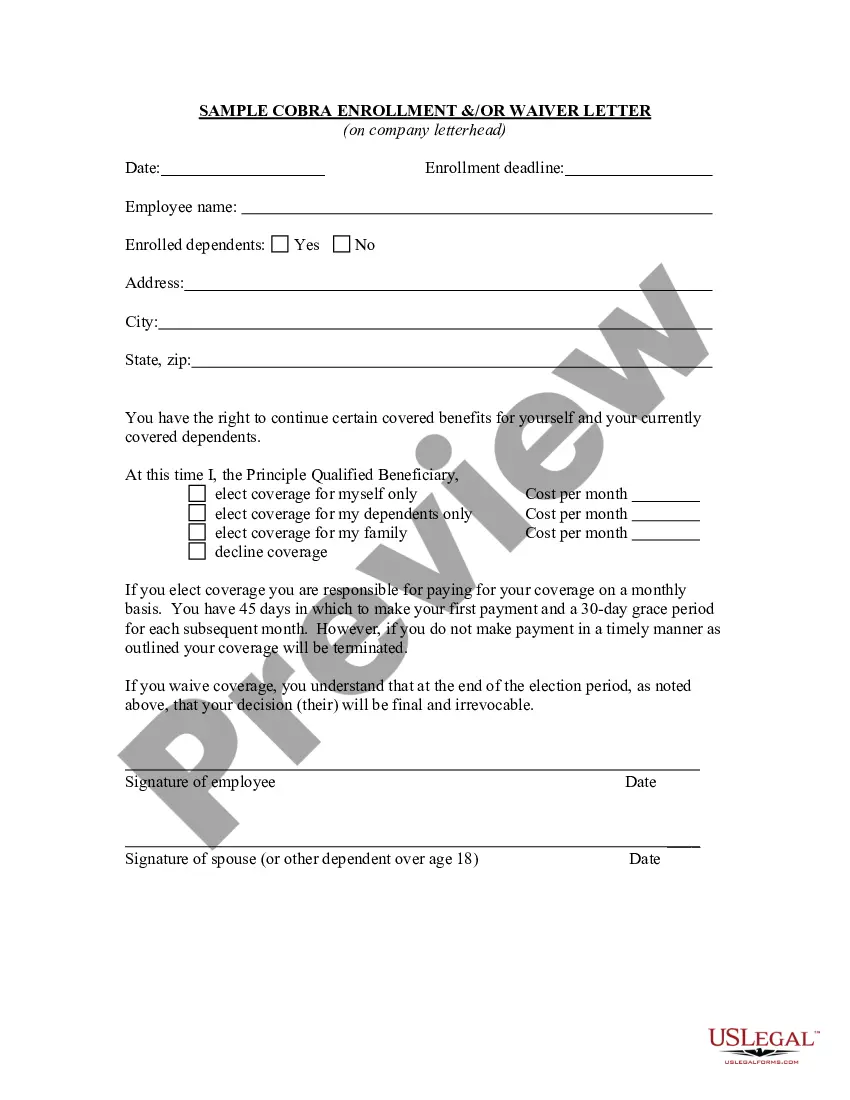
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
If you want to avoid paying the COBRA cost, go with a short-term plan if you're waiting for approval on another health plan. Choose a Marketplace or independent plan for broader coverage. Choose a high-deductible plan to keep your costs low.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
If you waive COBRA coverage during the election period, you must be permitted later to revoke your waiver of coverage and to elect continuation coverage as long as you do so during the election period. Then, the plan need only provide continuation coverage beginning on the date you revoke the waiver.
Instead, Assistance Eligible Individuals do not have to pay any of the COBRA premium for the period of coverage from April 1, 2021 through September 30, 2021. The premium is reimbursed directly to the employer, plan administrator, or insurance company through a COBRA premium assistance credit.
COBRA continuation coverage notices are documents that explain employees' rights under the Consolidated Omnibus Budget Reconciliation Act of 1985. These documents generally contain a variety of information, including the following: The name of the health insurance plan.