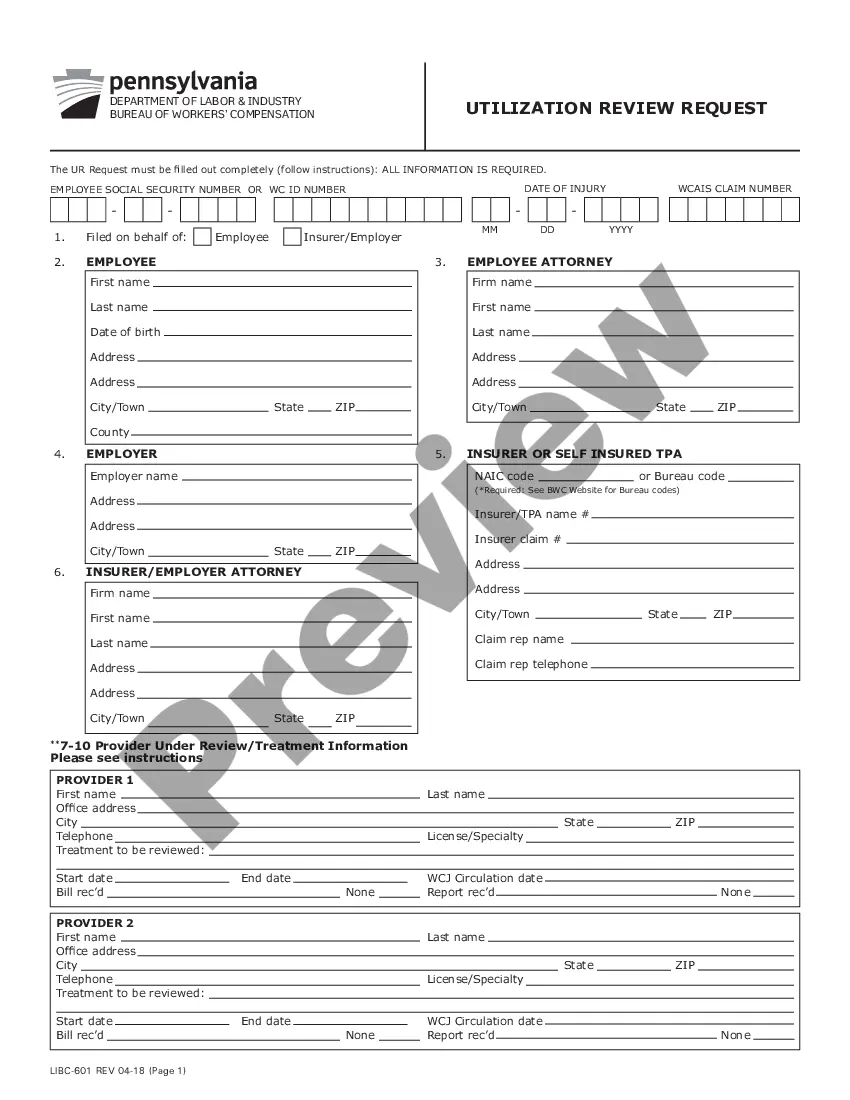
The Pennsylvania Utilization Review Determination Face Sheet is a document used by health insurance providers in Pennsylvania to review and determine the medical necessity of health care services. It is used to determine if a health care service is medically necessary and should be covered by insurance. The Face Sheet includes information about the patient, the requesting provider, the requested service, and the determination of medical necessity. There are two types of Pennsylvania Utilization Review Determination Face Sheets: Medical Necessity Determination Face Sheet and Non-Medical Necessity Determination Face Sheet. The Medical Necessity Determination Face Sheet is used when the requested service is considered medically necessary. The Non-Medical Necessity Determination Face Sheet is used when the requested service is not considered medically necessary.
Pennsylvania Utilization Review Determination Face Sheet
Description
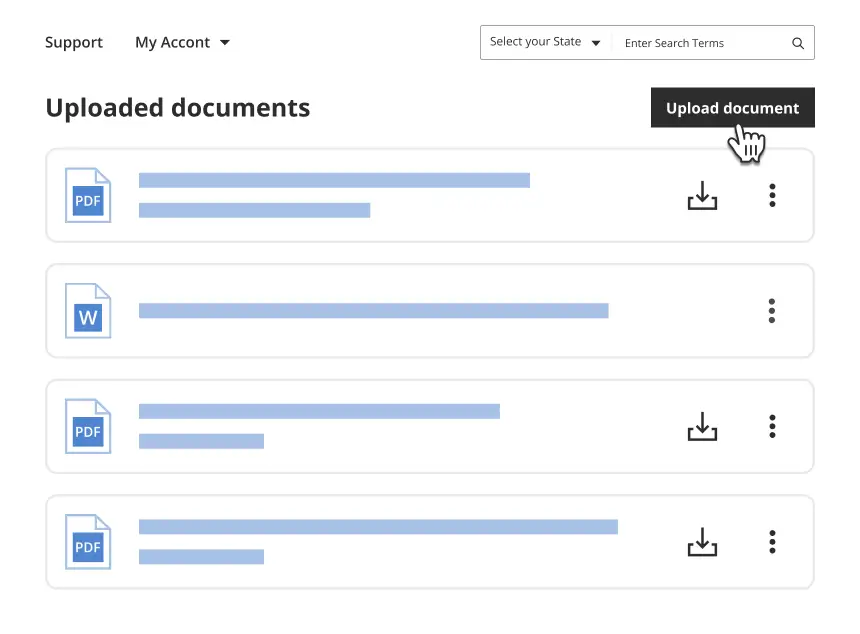
Get your form ready online
Our built-in tools help you complete, sign, share, and store your documents in one place.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Make edits, fill in missing information, and update formatting in US Legal Forms—just like you would in MS Word.
Download a copy, print it, send it by email, or mail it via USPS—whatever works best for your next step.
Sign and collect signatures with our SignNow integration. Send to multiple recipients, set reminders, and more. Go Premium to unlock E-Sign.
If this form requires notarization, complete it online through a secure video call—no need to meet a notary in person or wait for an appointment.
We protect your documents and personal data by following strict security and privacy standards.
Looking for another form?
How to fill out Pennsylvania Utilization Review Determination Face Sheet?
Preparing legal paperwork can be a real stress if you don’t have ready-to-use fillable templates. With the US Legal Forms online library of formal documentation, you can be confident in the blanks you obtain, as all of them correspond with federal and state regulations and are verified by our specialists. So if you need to prepare Pennsylvania Utilization Review Determination Face Sheet, our service is the perfect place to download it.
Obtaining your Pennsylvania Utilization Review Determination Face Sheet from our catalog is as easy as ABC. Previously authorized users with a valid subscription need only sign in and click the Download button after they locate the proper template. Afterwards, if they need to, users can get the same blank from the My Forms tab of their profile. However, even if you are unfamiliar with our service, signing up with a valid subscription will take only a few minutes. Here’s a quick guide for you:
- Document compliance check. You should carefully examine the content of the form you want and ensure whether it satisfies your needs and meets your state law regulations. Previewing your document and looking through its general description will help you do just that.
- Alternative search (optional). If there are any inconsistencies, browse the library using the Search tab above until you find a suitable template, and click Buy Now when you see the one you want.
- Account registration and form purchase. Create an account with US Legal Forms. After account verification, log in and select your most suitable subscription plan. Make a payment to continue (PayPal and credit card options are available).
- Template download and further usage. Select the file format for your Pennsylvania Utilization Review Determination Face Sheet and click Download to save it on your device. Print it to fill out your paperwork manually, or use a multi-featured online editor to prepare an electronic version faster and more effectively.
Haven’t you tried US Legal Forms yet? Subscribe to our service today to get any formal document quickly and easily every time you need to, and keep your paperwork in order!
Form popularity
FAQ
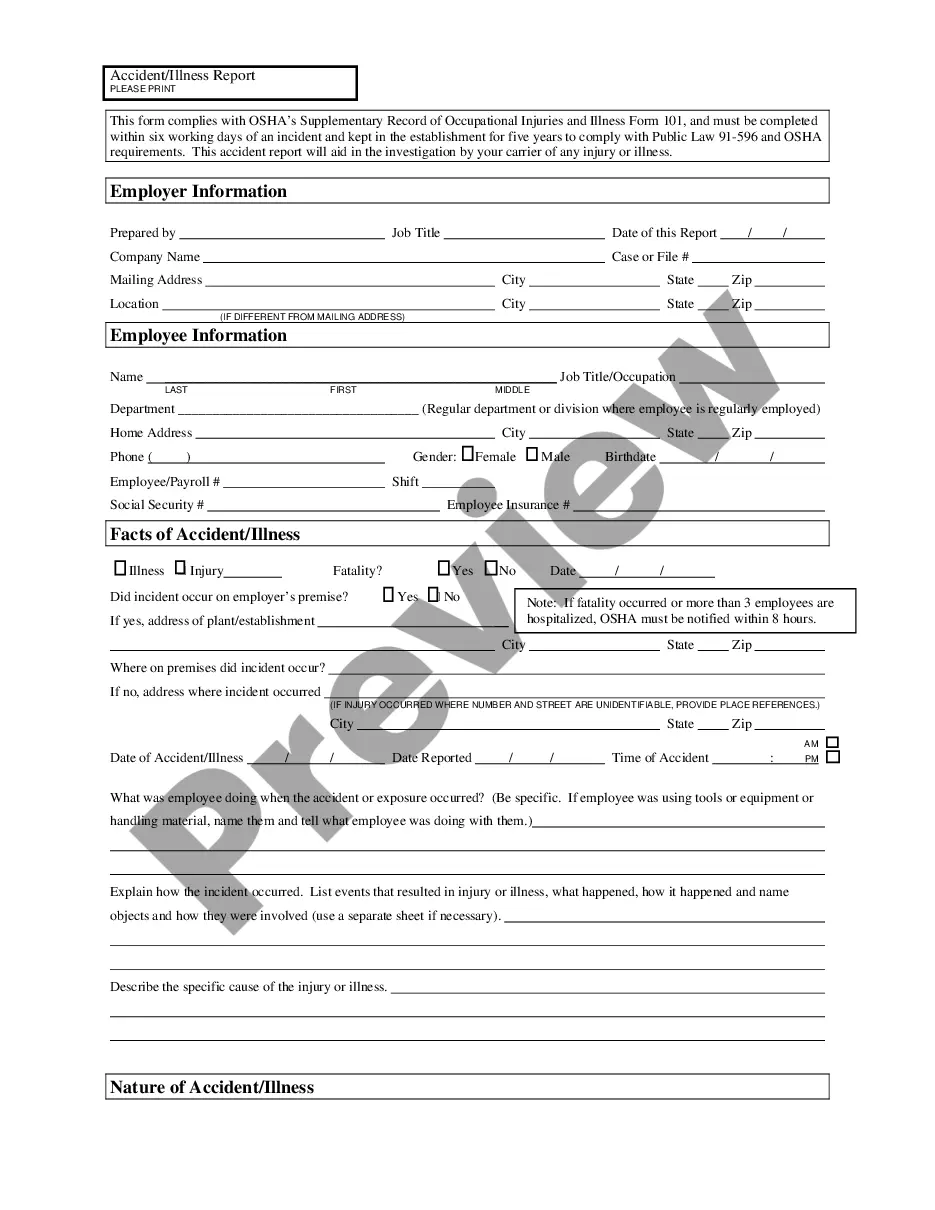
Form LIBC-344 First Report of Injury (FROI). As soon as you have been notified of a work-related injury, please fill out this form and submit it to EMPLOYERS. This form must be completed within 10 days from notice of a work-related injury. Fatalities must be reported within 24 hours.
Under the Pennsylvania Workers' Compensation Act, injured workers are entitled to wage loss (?indemnity benefits?) based on the earnings at the time of injury. Generally speaking, indemnity benefits are calculated based on two-thirds (2/3) of your average weekly wage (?AWW?).
Workers' Compensation is tax-free. In Pennsylvania, the weekly compensation rate amounts to 66% of the injured worker's average weekly wage if they earned between $810.76 and $1,621.50 prior to the injury. For workers who earn between $600.56 and $810.75, the weekly compensation rate is $540.50.
The utilization review process provides for the impartial review of the reasonableness or necessity of medical treatment rendered to, or proposed for, work-related injuries and illnesses.
The maximum amount of wage loss benefits is based on the Department of Labor and Industry's calculation of the statewide average weekly wage. For the calendar year 2023 the maximum weekly compensation rate is $1,273.00. This amount only applies if you sustain a work-related injury in 2023 that results in wage loss.
The proposed employer assessment factor is 0.0318. This factor, in concert with the proposed employer assessment procedure, is subject to approval by the Insurance Commissioner.
The Employer's Assessment Fee Is 0.0289 (2.89%)
The Pennsylvania Workers' Compensation Act provides wage loss and medical benefits to compensate employees suffering from work- related injuries or diseases. The Act also provides for death benefits to the dependents of workers who die as a result of a work-related injury or disease.