Oregon Qualifying Event Notice Information for Employer to Plan Administrator
Description
How to fill out Qualifying Event Notice Information For Employer To Plan Administrator?
If you desire to finalize, download, or print legal document templates, utilize US Legal Forms, the premier collection of legal forms, available online.
Make use of the site's straightforward and user-friendly search to obtain the documents you need.
Various templates for business and personal purposes are categorized by type and state, or keywords.
Step 4. Once you have located the form you want, select the Acquire now button. Choose the payment plan you prefer and enter your information to register for an account.
Step 5. Process the payment. You can use your Visa or MasterCard or PayPal account to complete the transaction.
- Utilize US Legal Forms to retrieve the Oregon Qualifying Event Notice Information for Employer to Plan Administrator in just a couple of clicks.
- If you are already a US Legal Forms user, Log In to your account and click on the Obtain button to find the Oregon Qualifying Event Notice Information for Employer to Plan Administrator.
- You can also access forms you previously acquired in the My documents tab of your account.
- If you utilize US Legal Forms for the first time, refer to the following instructions.
- Step 1. Ensure you have selected the form for the correct area/state.
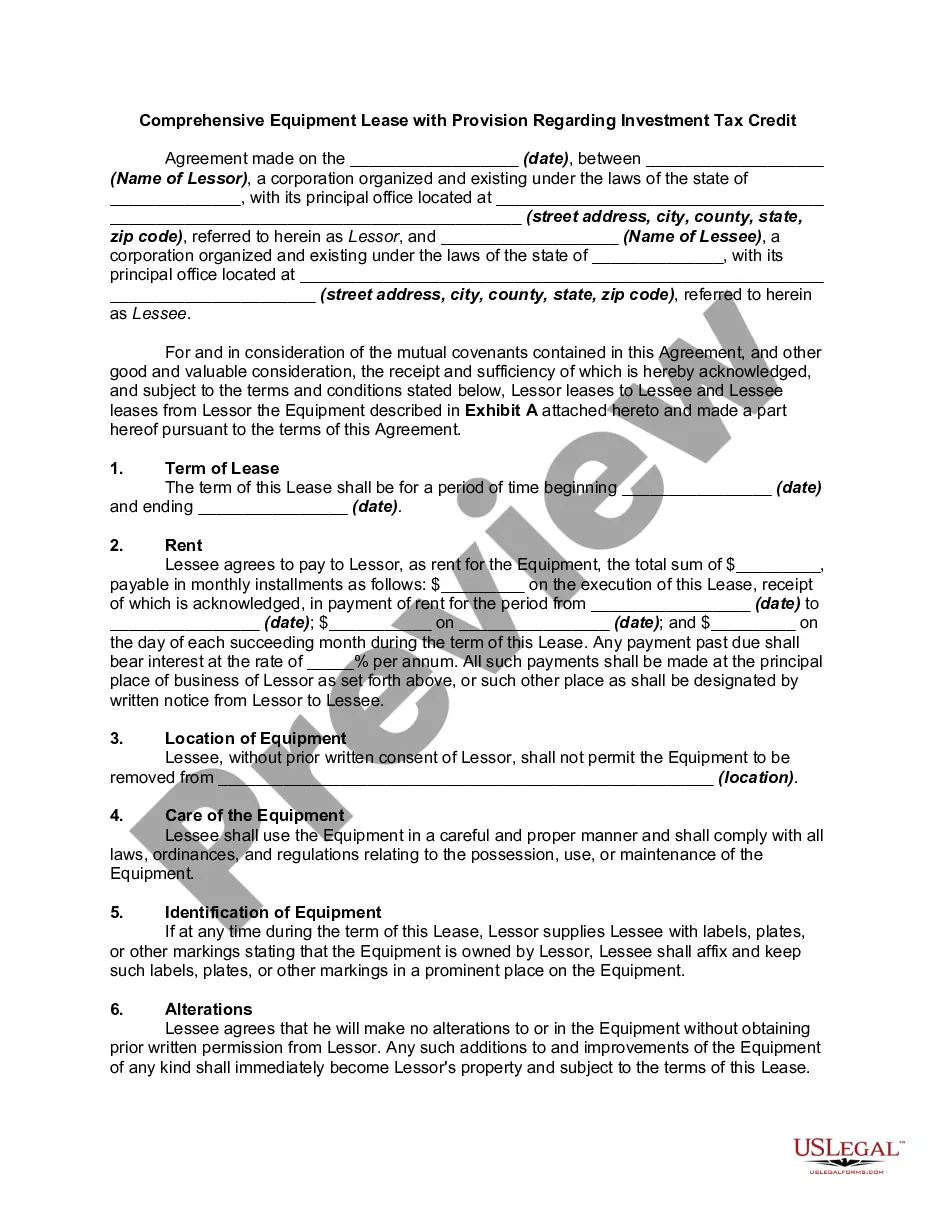
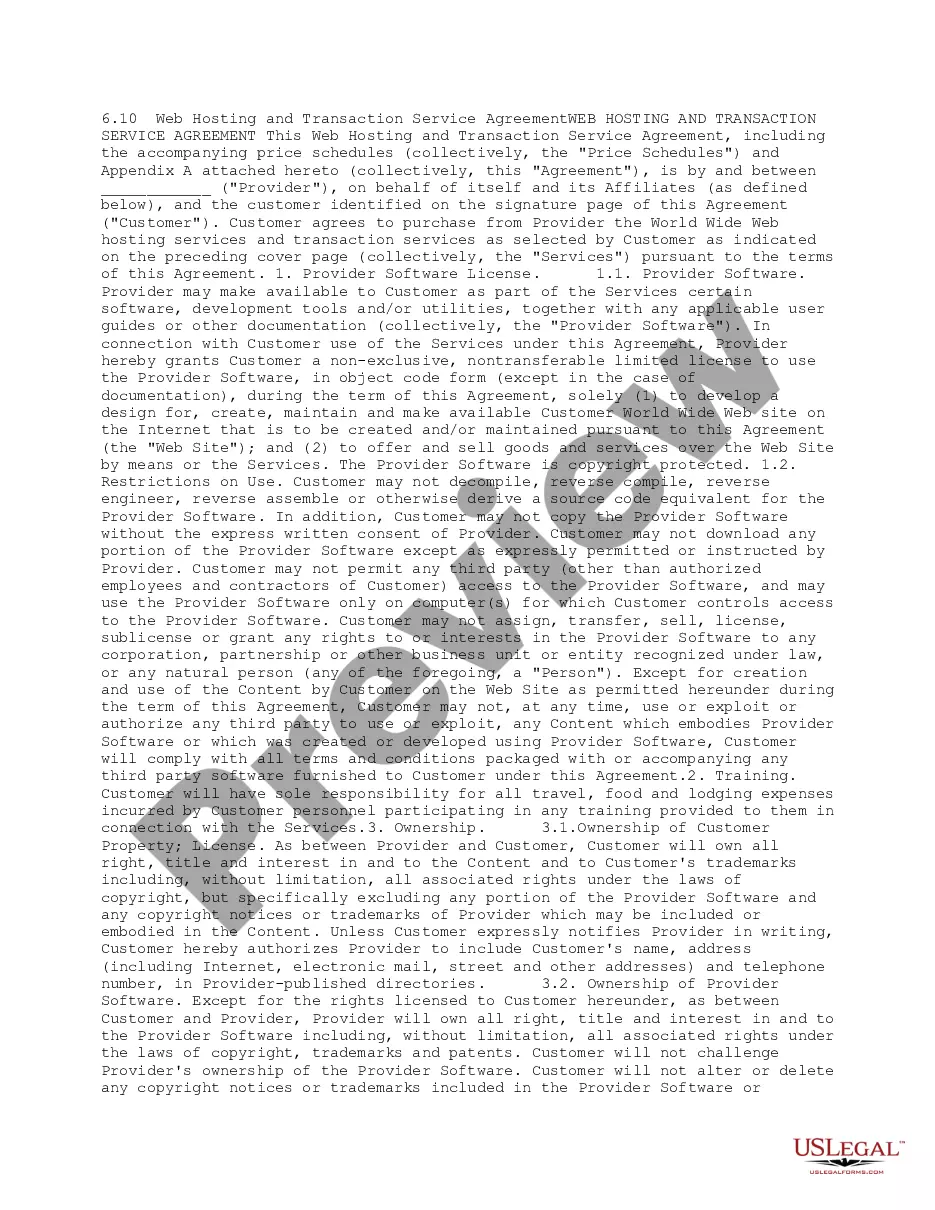
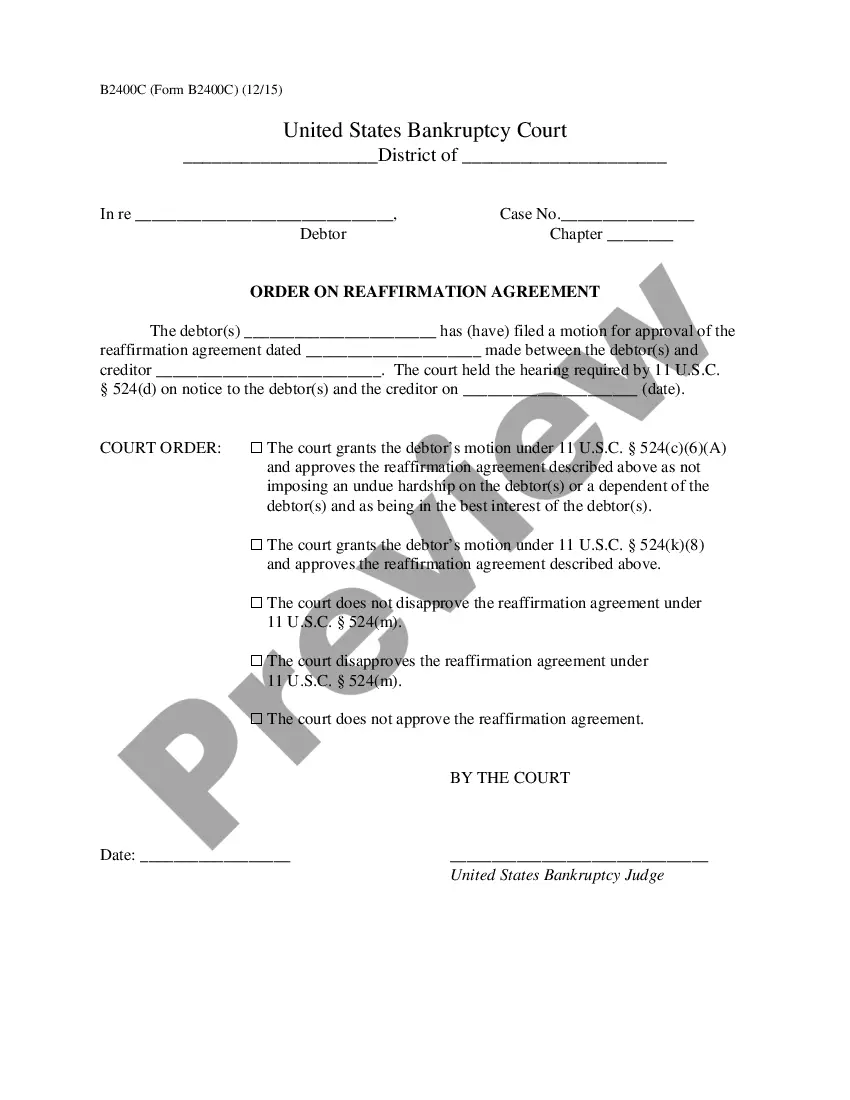
- Step 2. Use the Preview option to review the form's details. Don't forget to read the description.
- Step 3. If you are not satisfied with the template, use the Search area at the top of the screen to find other versions of the legal form design.
Form popularity
FAQ
Justin is receiving disability income benefits from a group policy paid for by his employer. How are these benefits treated for tax purposes? (A single contract for Group Medical Insurance issued to an employer is known as a master policy.)
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
COBRA is a federal law under which certain former employees, retirees, spouses, former spouses and dependent children have the right to temporarily continue their existing group health coverage at group rates when group coverage otherwise would end due to certain life events, called 'Qualifying Events.
COBRA generally applies to all private-sector group health plans maintained by employers that have at least 20 employees on more than 50 percent of its typical business days in the previous calendar year. Both full- and part-time employees are counted to determine whether a plan is subject to COBRA.
COBRA generally applies to all group health plans maintained by private-sector employers with at least 20 employees or by state and local governments.