Oregon Notice of Qualifying Event from Employer to Plan Administrator
Description
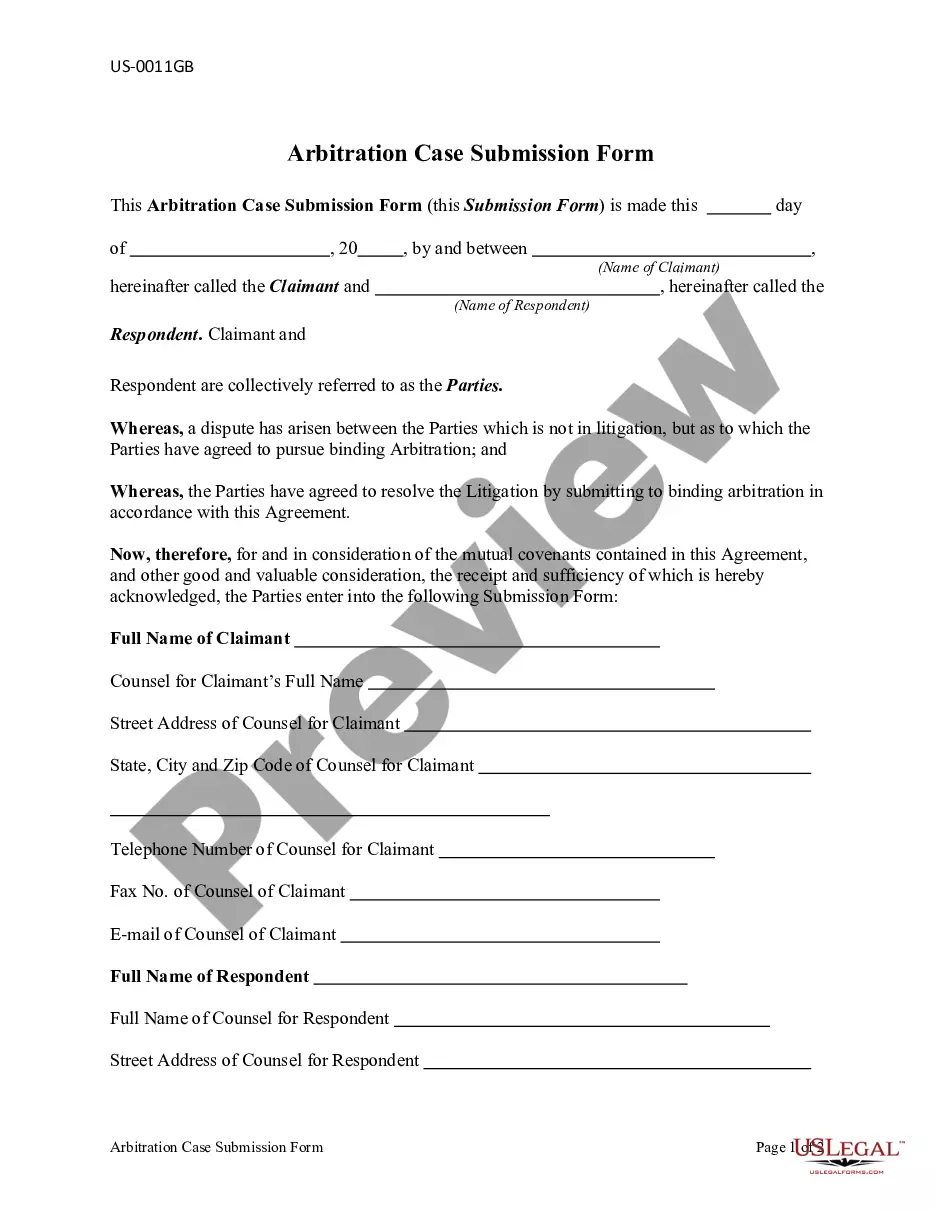
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
Are you presently in a situation where you require documents for occasional business or personal use almost daily.
There are numerous legitimate form templates accessible online, but locating reliable ones can be challenging.
US Legal Forms provides a vast selection of form templates, such as the Oregon Notice of Qualifying Event from Employer to Plan Administrator, that are designed to comply with federal and state regulations.
Once you have found the correct form, click Purchase now.
Choose your preferred payment plan, complete the required information to create your account, and finalize the transaction using PayPal or a credit card.
- If you are already acquainted with the US Legal Forms website and possess an account, simply Log In.
- Then, you can download the Oregon Notice of Qualifying Event from Employer to Plan Administrator template.
- If you do not have an account and wish to start using US Legal Forms, follow these instructions.
- Select the form you need and ensure it is for the correct city/state.
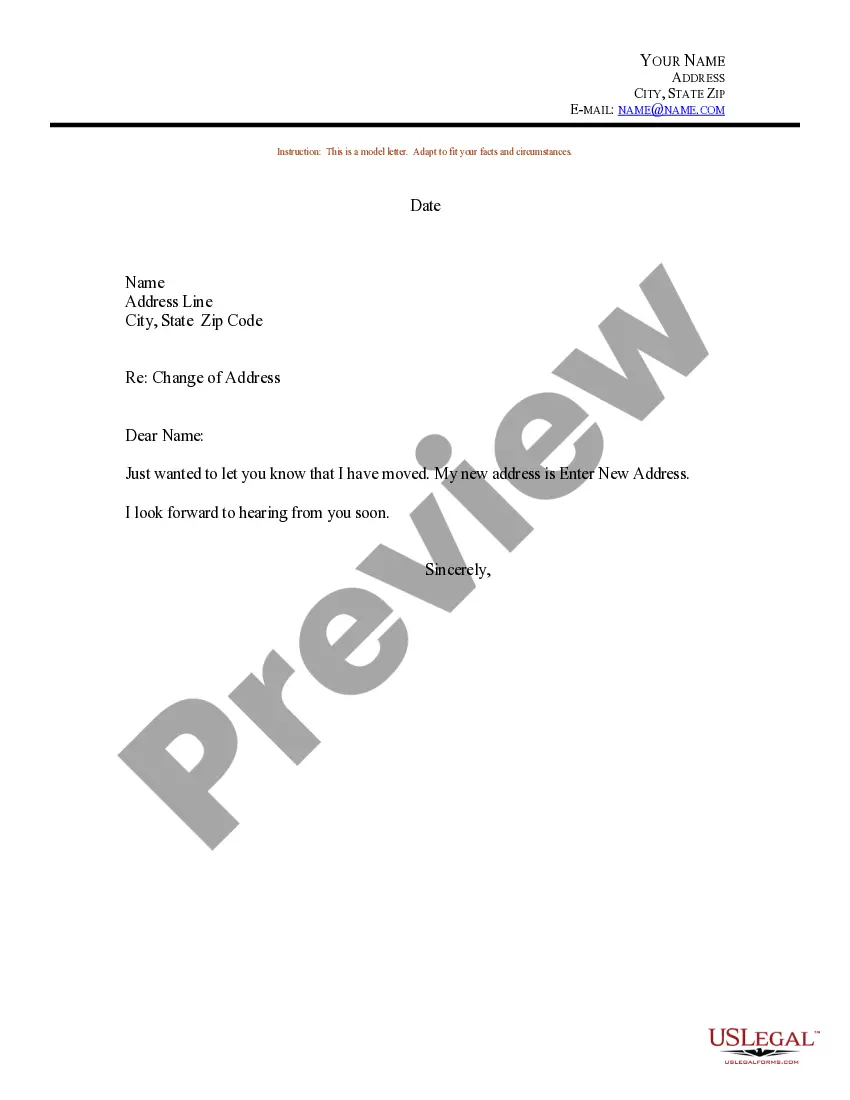
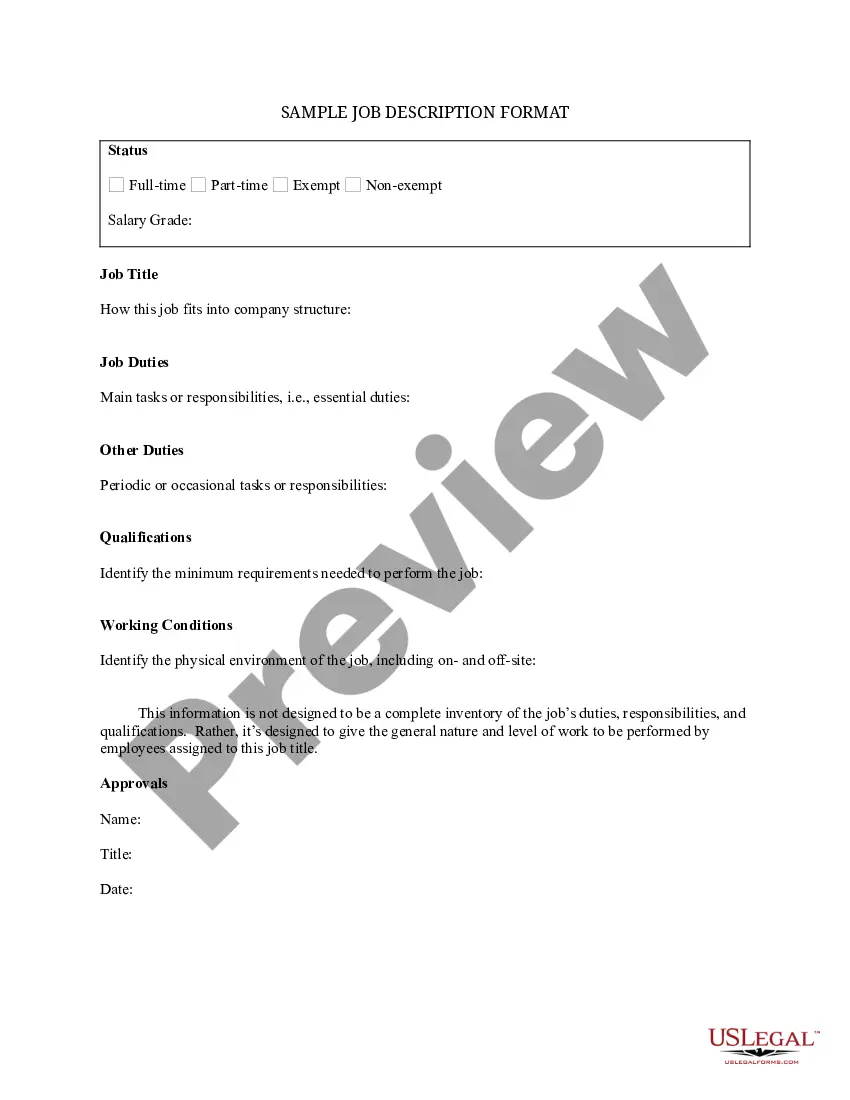
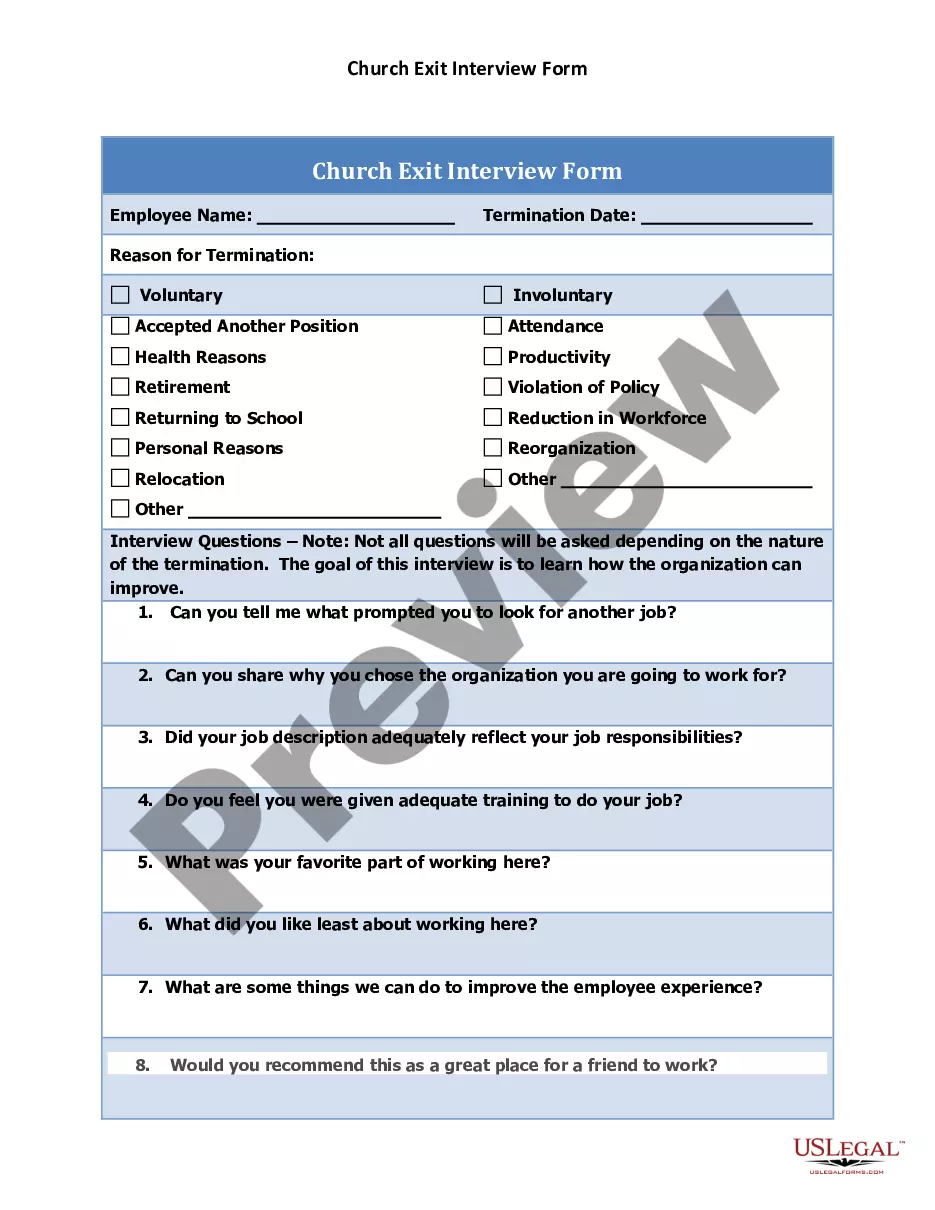
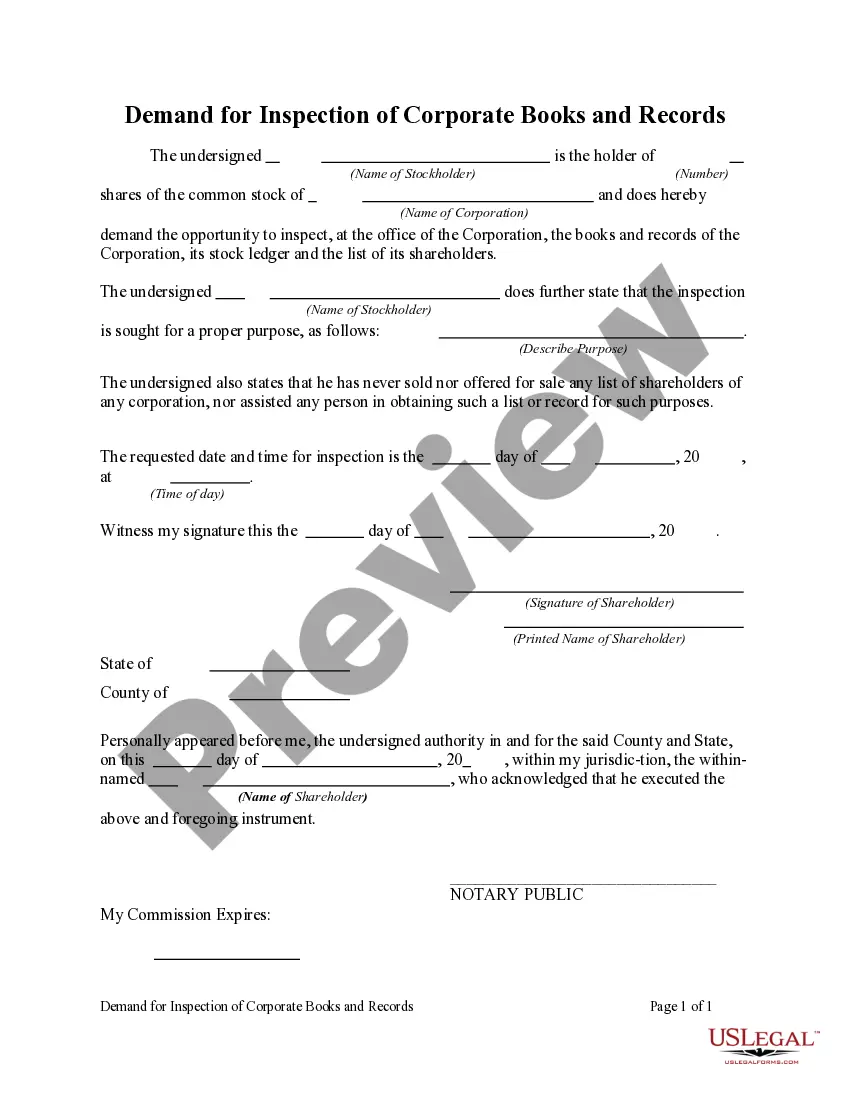
- Utilize the Review button to examine the form.
- Check the description to ensure you have chosen the correct form.
- If the form does not meet your needs, use the Search field to locate the form that fulfills your specifications.
Form popularity
FAQ
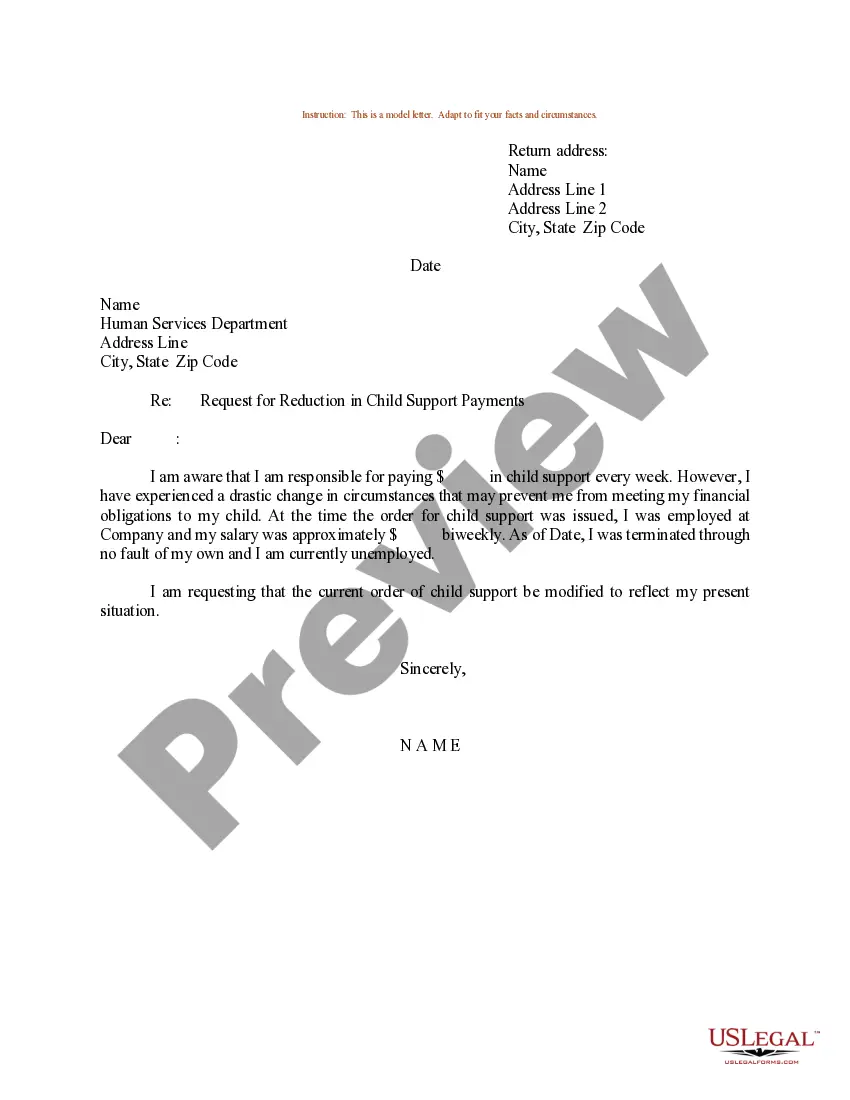
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Who is eligible? An employee who has had continuous health coverage (not necessarily with the same employer) for at least three months prior to the date employment or coverage ended. The employee's spouse and children are also eligible to maintain coverage.
COBRA continuation coverage is a temporary continuation of coverage that generally lasts for 18 months due to employment termination or reduction of hours of work.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
What is COBRA continuation coverage? COBRA is a federal law that requires large employers (including Multnomah County) to offer employees and their families the opportunity to continue their health care coverage when there is a qualifying event that would result in a loss of coverage in the County's health plan.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
You have only 60 days from the date you lost your employer coverage to purchase coverage directly from us or another health insurance carrier. If you do not enroll within 60 days, you must wait until the next open enrollment period to buy an individual health plan.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.