Ohio Authorization for Use and / or Disclosure of Protected Health Information
Description
How to fill out Authorization For Use And / Or Disclosure Of Protected Health Information?
If you require to obtain, download, or print legal document templates, utilize US Legal Forms, the largest selection of legal forms available online.
Take advantage of the website's simple and user-friendly search to locate the documents you need.
Various templates for business and personal needs are categorized by type and jurisdiction, or by keywords. Utilize US Legal Forms to acquire the Ohio Authorization for Use and/or Disclosure of Protected Health Information in just a few clicks.
Every legal document template you acquire is yours indefinitely. You can access any document you have saved in your account. Click on the My documents section and select a document to print or download again.
Act quickly and download or print the Ohio Authorization for Use and/or Disclosure of Protected Health Information with US Legal Forms. There are thousands of professional and state-specific forms available for your business or personal needs.
- If you are already a US Legal Forms customer, Log In to your account and click the Download button to access the Ohio Authorization for Use and/or Disclosure of Protected Health Information.
- You can also view forms you previously saved in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the instructions below.
- Step 1. Ensure you have selected the form for your correct city/state.
- Step 2. Use the Review option to examine the form's details. Don't forget to read the description.
- Step 3. If you are unsatisfied with the form, use the Search box at the top of the page to find alternative versions of the legal form template.
- Step 4. Once you find the form you need, select the Buy now button. Choose the pricing plan you prefer and enter your information to sign up for an account.
- Step 5. Complete the transaction. You can use your credit card or PayPal account to finalize the payment.
- Step 6. Choose the format of the legal form and download it to your device.
- Step 7. Complete, edit, and print or sign the Ohio Authorization for Use and/or Disclosure of Protected Health Information.
Form popularity
FAQ
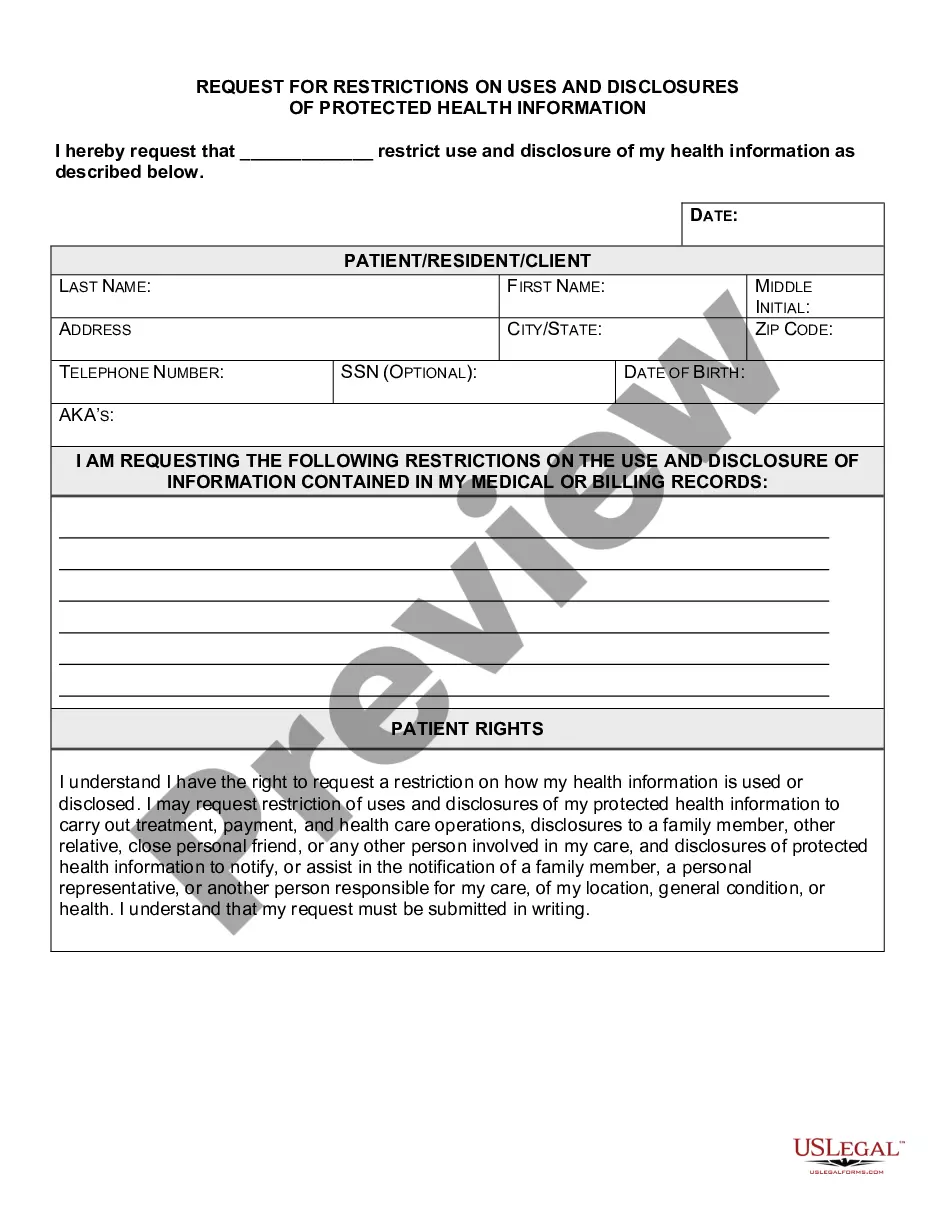
You must obtain authorization from a person before disclosing their protected health information in situations that do not fall under exemptions set by law. For example, if you plan to share their information for marketing purposes or research, getting their consent through an Ohio Authorization for Use and / or Disclosure of Protected Health Information is necessary. This ensures compliance with legal standards and respects the individual's privacy. Clear authorization not only protects the individual's rights but also ensures your organization adheres to regulatory mandates.
Unauthorized access, use, and disclosure of protected health information occurs when PHI is accessed or shared without proper authorization. This can lead to serious privacy violations and potential legal consequences. It's essential to protect patient data by following the guidelines outlined in the Ohio Authorization for Use and / or Disclosure of Protected Health Information. Utilizing secure, compliant platforms can help mitigate such risks.
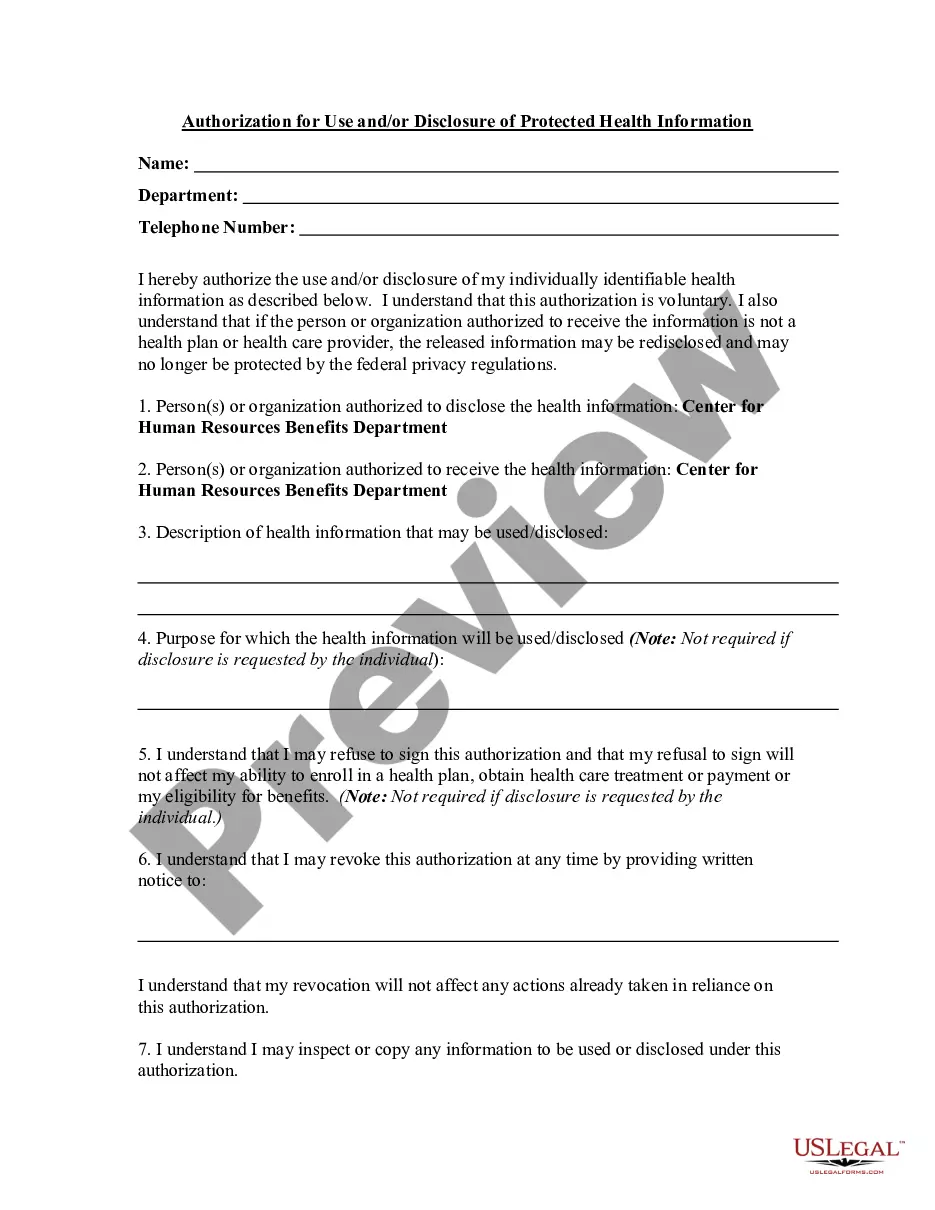
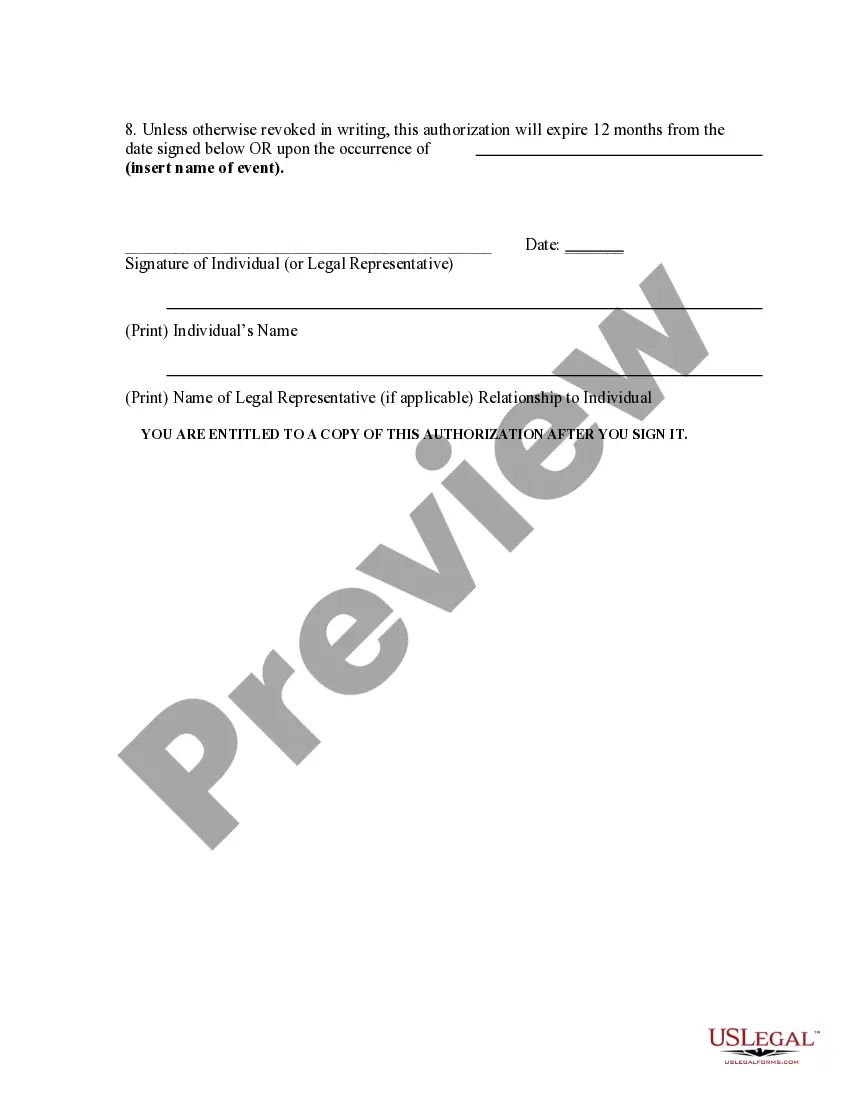
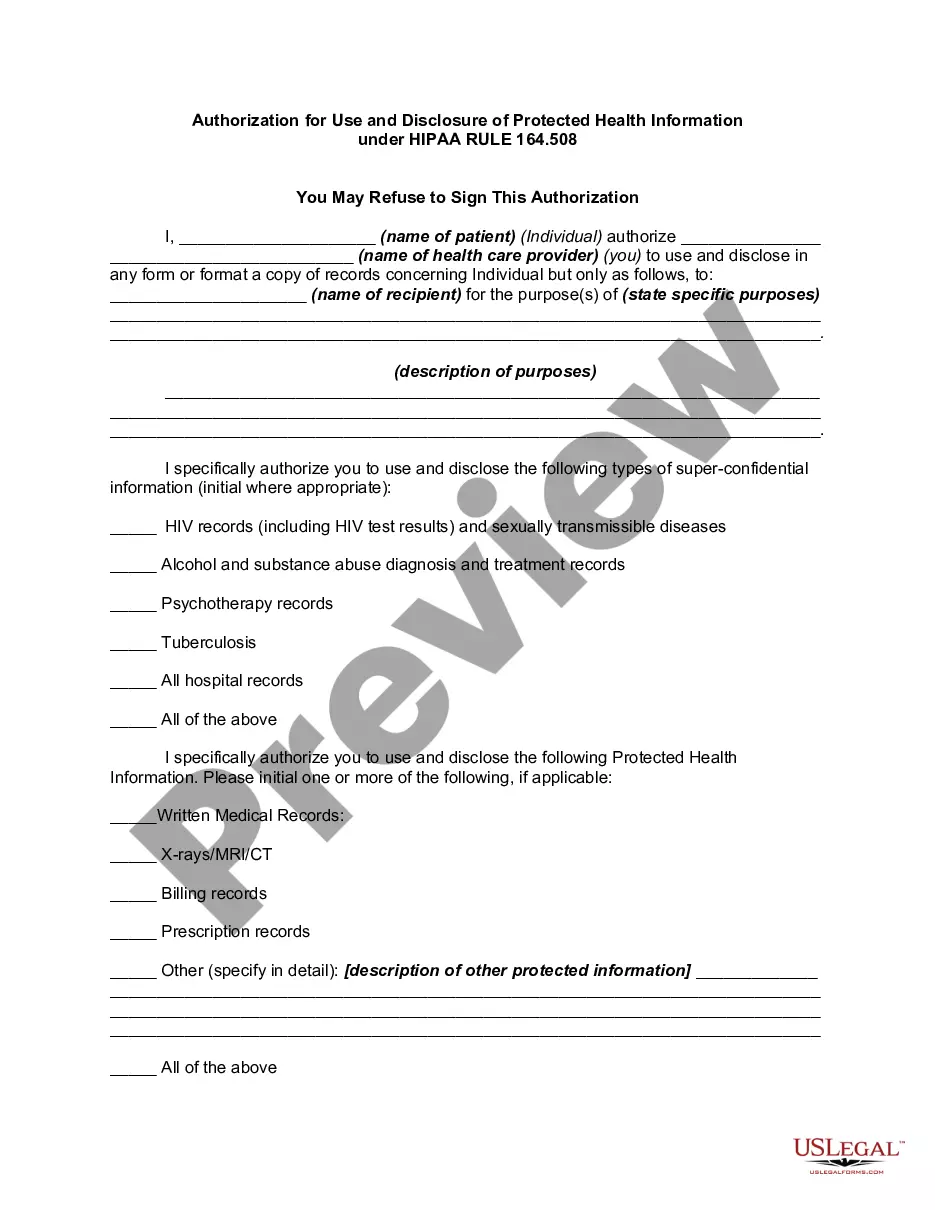
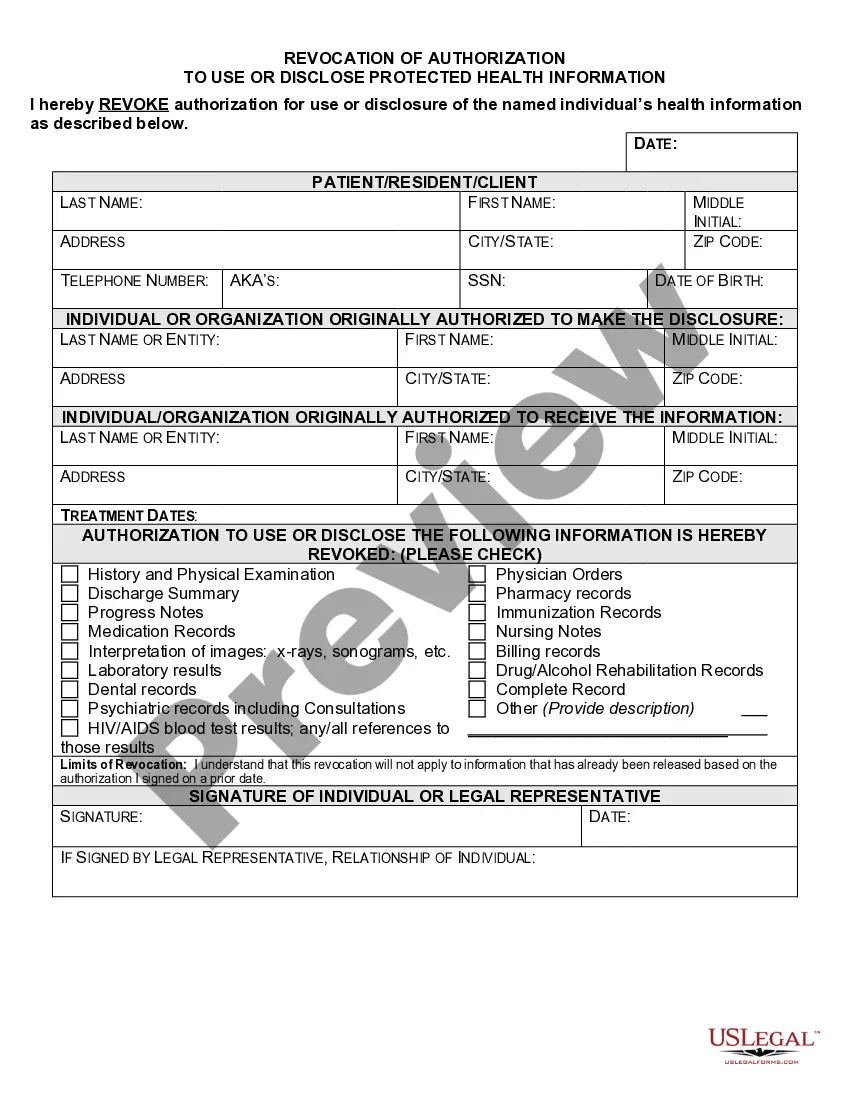
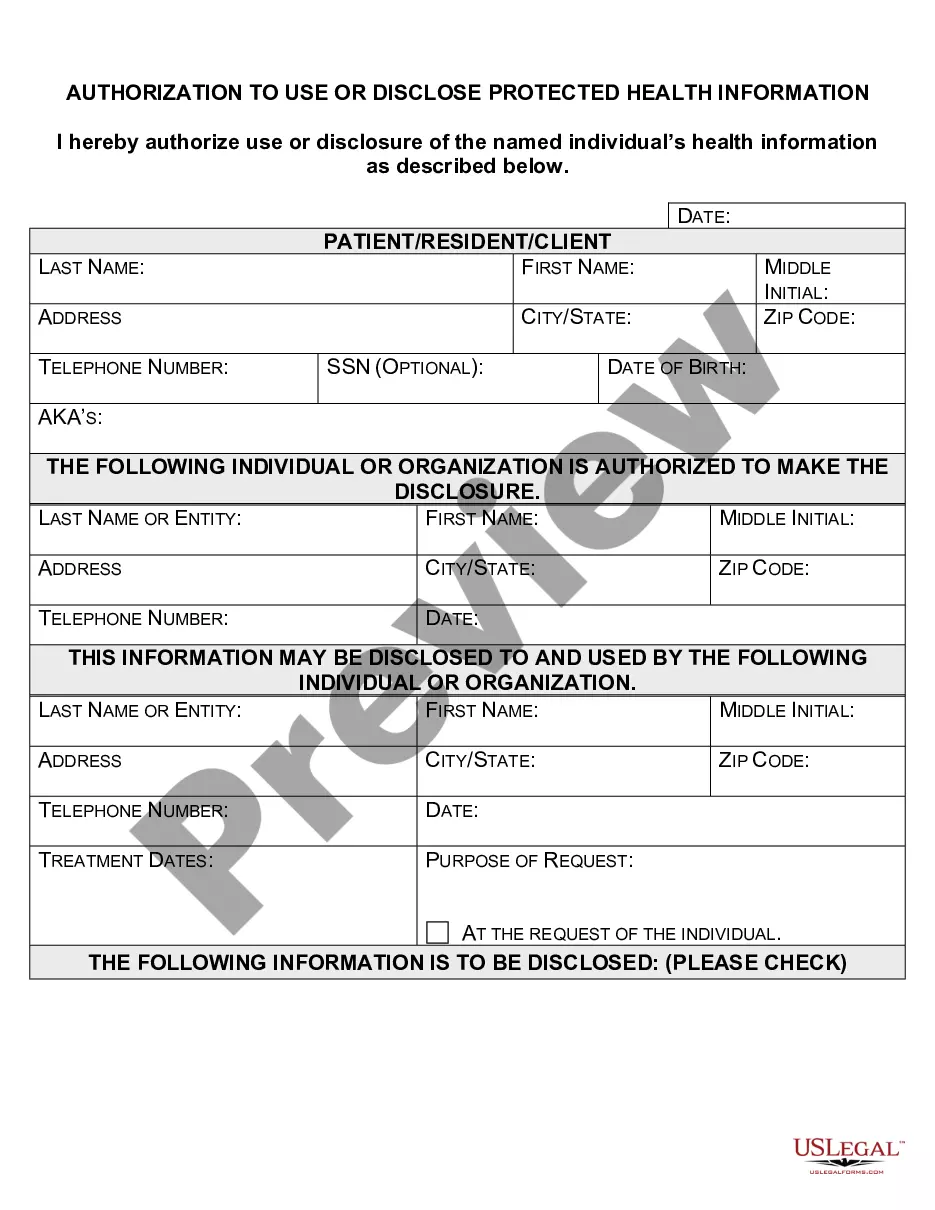
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the
We may disclose your PHI for the following government functions: (1) Military and veterans activities, including information relating to armed forces personnel for the execution of military missions, separation or discharge from military services, veterans benefits, and foreign military personnel; (2) National security
When Must HIPAA Authorization be Obtained? The covered entity can use or disclosure of PHI for marketing purposes. If the marketing communication involves direct or indirect remuneration to the covered entity from a third party, the authorization must state that such remuneration is involved.
A covered entity must obtain the individual's written authorization for any use or disclosure of protected health information that is not for treatment, payment or health care operations or otherwise permitted or required by the Privacy Rule.
Marketing Activities: A covered entity must obtain an individual's authorization prior to using or disclosing PHI for marketing activities. Marketing is considered any message or statement to the public in an effort to get them to use or seek more information about a product or service.
A covered entity must disclose protected health information in only two situations: (a) to individuals (or their personal representatives) specifically when they request access to, or an accounting of disclosures of, their protected health information; and (b) to HHS when it is undertaking a compliance investigation or
A patient authorization is not required for disclosure of PHI between Covered Entities if the disclosure is needed for purposes of treatment or payment or for healthcare operations. You may disclose the PHI as long as you receive a request in writing.
The HIPAA Privacy Rule requires that an individual provide signed authorization to a covered entity, before the entity may use or disclose certain protected health information (PHI).