New York Introductory COBRA Letter
Description
How to fill out Introductory COBRA Letter?
US Legal Forms - one of the largest collections of legal documents in the United States - provides an extensive array of legal form templates that you can download or print. By utilizing the website, you can access thousands of forms for business and personal use, categorized by types, states, or keywords. You can find the latest versions of forms such as the New York Introductory COBRA Letter in just moments.
If you already hold a monthly subscription, Log In and download the New York Introductory COBRA Letter from your US Legal Forms library. The Download button will be visible on every form you check out. You can access all previously obtained forms in the My documents section of your account.
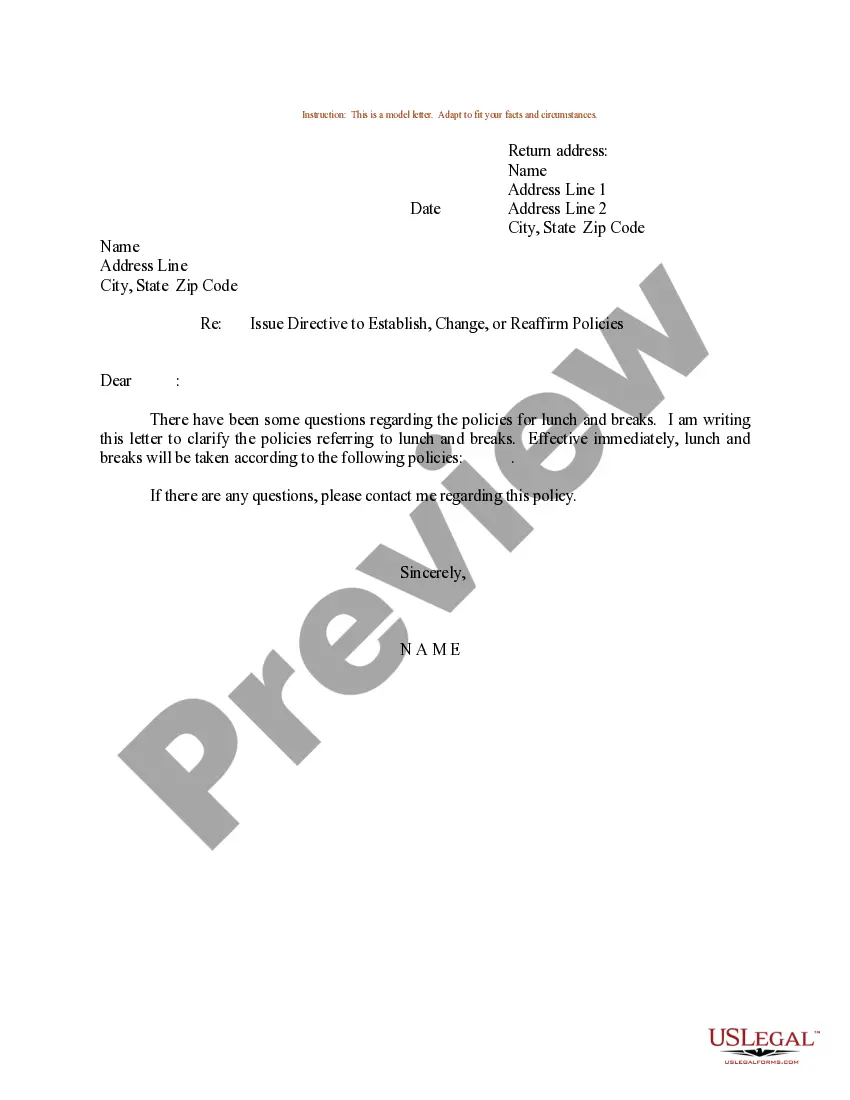
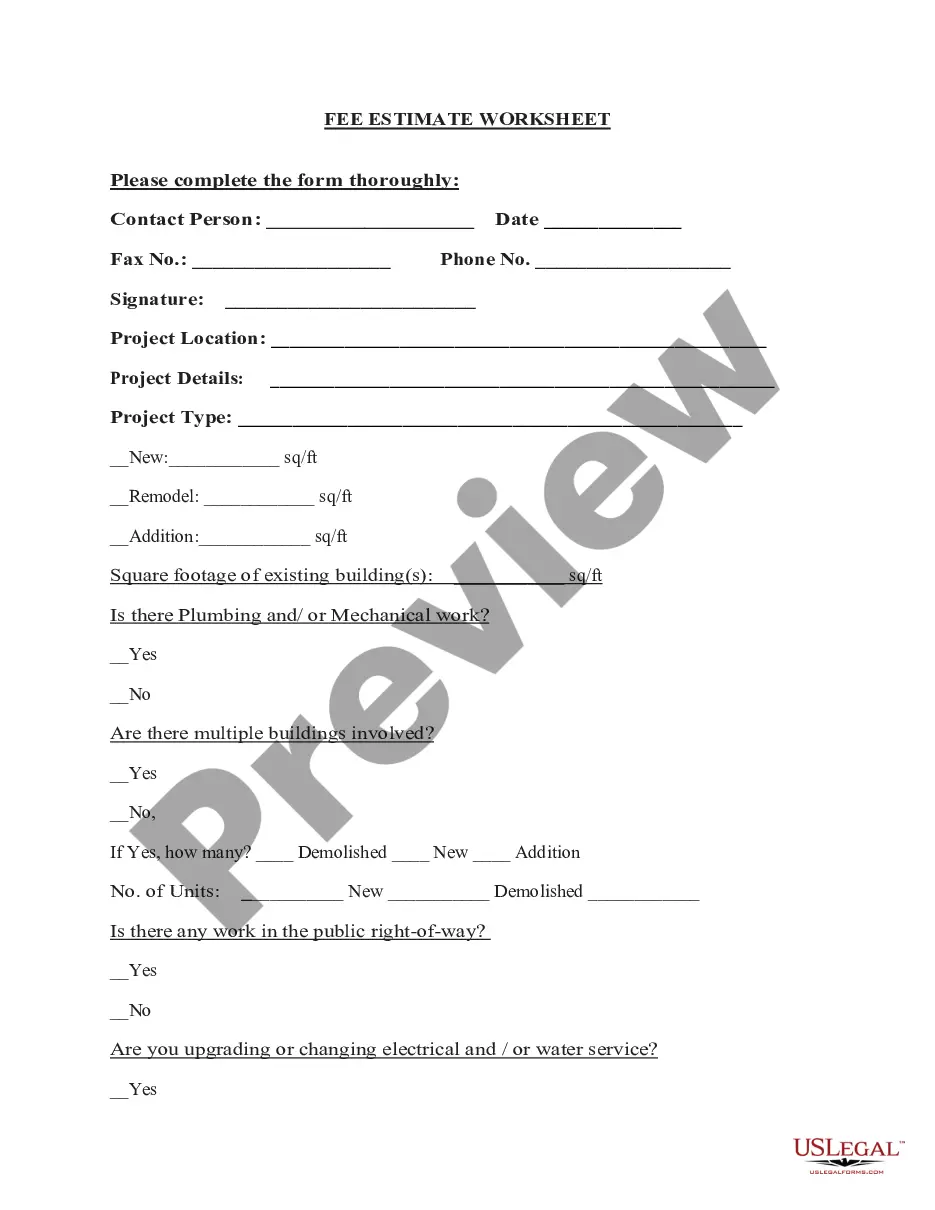
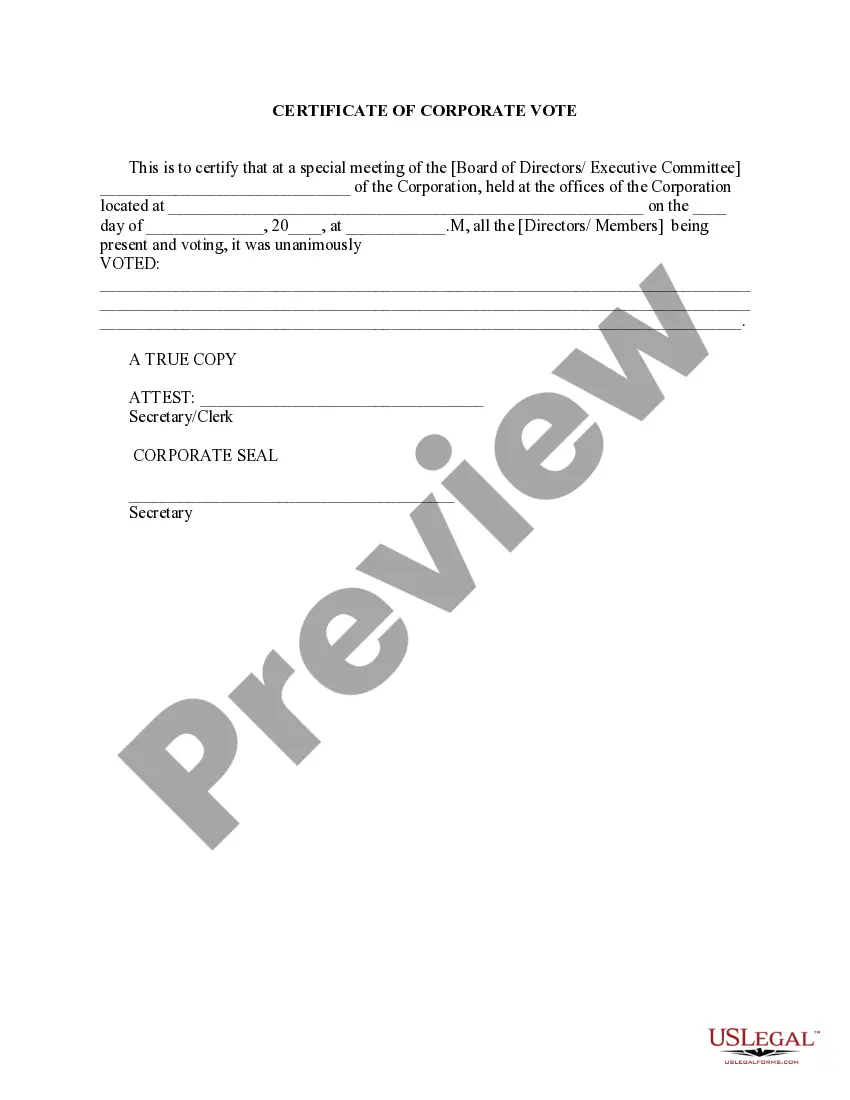
If you are using US Legal Forms for the first time, here are simple instructions to get started: Verify that you have selected the correct form for your city/state. Click on the Preview button to examine the form's content. Review the form summary to ensure you have chosen the correct document. If the form does not fulfill your requirements, utilize the Search field at the top of the screen to find one that does.
Access the New York Introductory COBRA Letter with US Legal Forms, the most comprehensive collection of legal document templates. Utilize a vast number of professional and state-specific templates that meet your business or personal needs and requirements.
- If you are satisfied with the form, confirm your selection by clicking the Purchase now button.
- Then, pick the payment plan you desire and provide your details to register for an account.
- Process the transaction. Use your credit card or PayPal account to complete the purchase.
- Select the format and download the form to your device.
- Make modifications. Complete, edit, print, and sign the downloaded New York Introductory COBRA Letter.
- Every template you added to your account has no expiration date and is yours indefinitely. Thus, if you want to download or print an additional copy, simply head over to the My documents section and click on the form you need.
Form popularity
FAQ
In New York, COBRA coverage can extend for either 18 or 36 months, depending on specific circumstances. Generally, if you experience a qualifying event like job loss or reduced work hours, you may be eligible for 18 months of coverage. However, if you are a dependent or if specific situations arise, this duration could extend to 36 months. To ensure you understand your eligibility, reviewing a New York Introductory COBRA Letter is beneficial.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) permits employees and their dependents to extend health coverage under an employer's group health plan when coverage would otherwise be lost due to termination of employment or other qualifying events. Under COBRA, employees must receive specific notices
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
New York State law requires small employers (less than 20 employees) to provide the equivalent of COBRA benefits. You are entitled to 36 months of continued health coverage at a monthly cost to you of 102% of the actual cost to the employer which may be different from the amount deducted from your paychecks.
Failure to pay premiums. When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums.
You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.