Nevada Hospital Audit Program
Description
How to fill out Hospital Audit Program?
If you want to be thorough, download, or print legal document templates, use US Legal Forms, the biggest variety of legal forms, which are available online.
Utilize the website's simple and user-friendly search feature to find the documents you need.
Various templates for professional and personal purposes are organized by categories and claims, or keywords.
Every legal document template you purchase is yours permanently. You can access every form you downloaded in your account. Click on the My documents section and choose a form to print or download again.
Complete and retrieve, and print the Nevada Hospital Audit Program with US Legal Forms. There are millions of professional and state-specific forms available for your business or personal requirements.
- Use US Legal Forms to acquire the Nevada Hospital Audit Program in just a few clicks.
- If you are already a US Legal Forms customer, Log In to your account and click the Obtain button to access the Nevada Hospital Audit Program.
- You can also find forms you previously downloaded in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow the steps below.
- Step 1. Ensure you have chosen the form for your appropriate city/state.
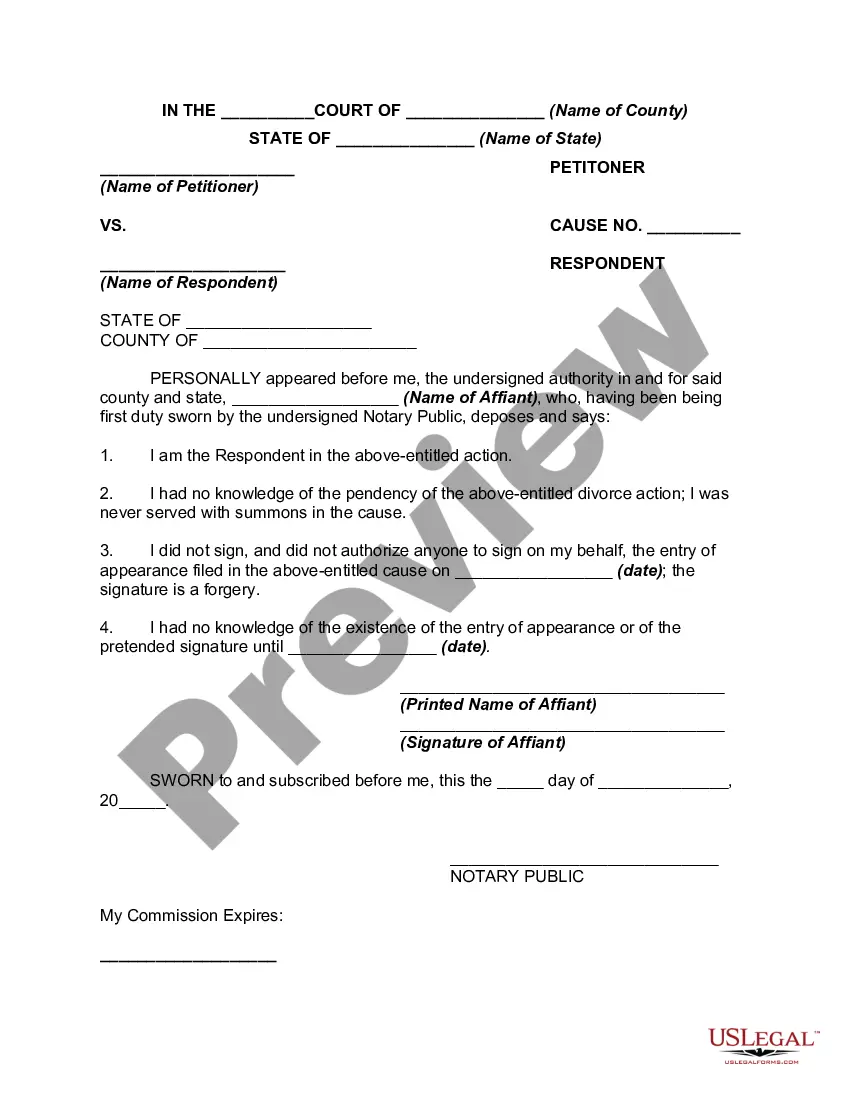
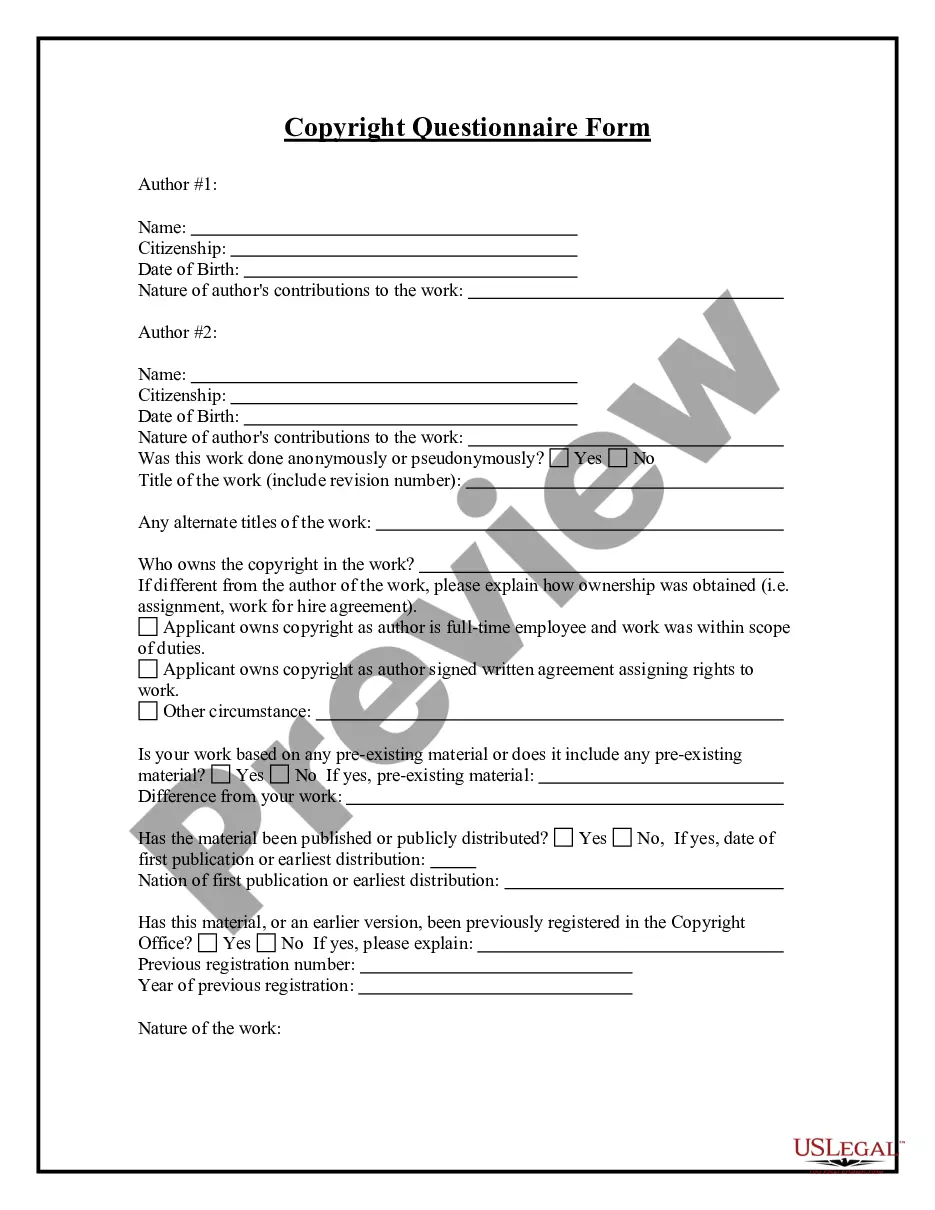
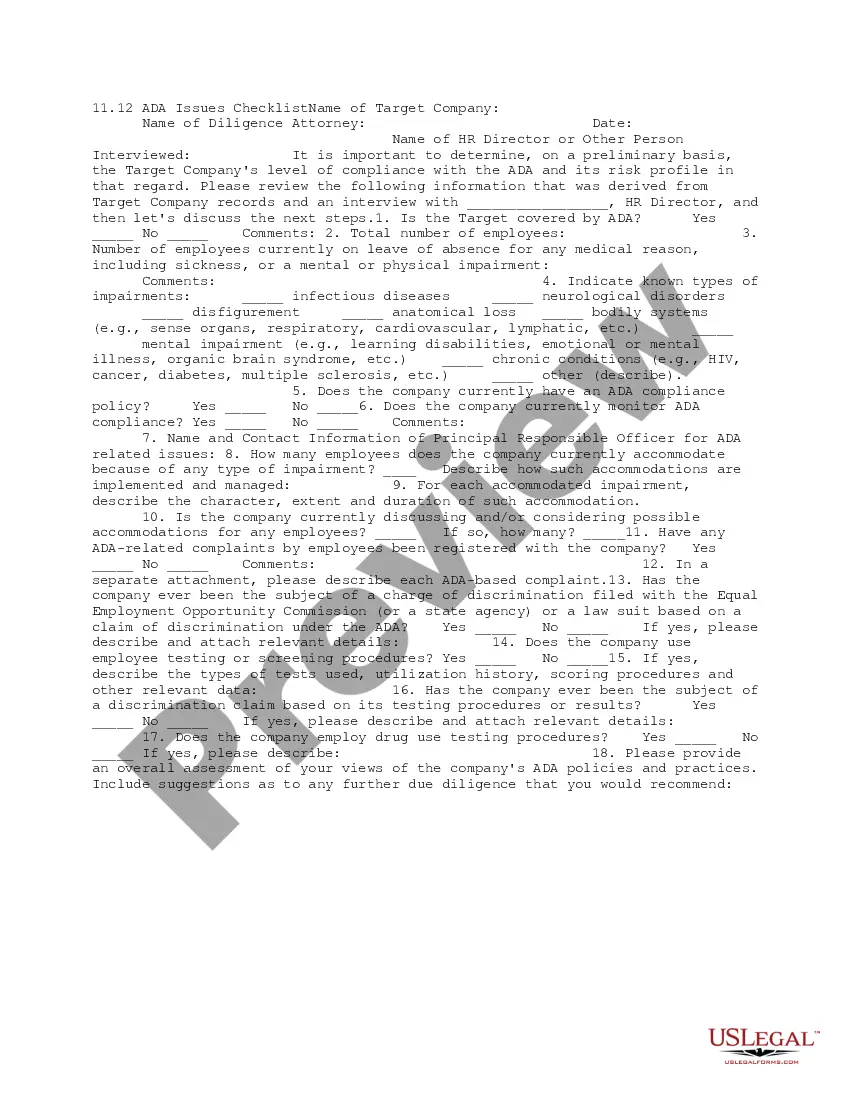
- Step 2. Use the Preview function to review the form's content. Don't forget to read the description.
- Step 3. If you are not satisfied with the form, utilize the Search field at the top of the screen to find other versions of the legal form template.
- Step 4. Once you have found the form you need, click on the Purchase now button. Select the payment plan you prefer and enter your information to create an account.
- Step 5. Complete the transaction. You can use your Visa or Mastercard or PayPal account to finalize the purchase.
- Step 6. Choose the format of the legal document and download it to your device.
- Step 7. Complete, modify, and print or sign the Nevada Hospital Audit Program.
Form popularity
FAQ
MAC audits are powerful and intrusive procedures that have the potential to lead to serious federal charges for healthcare entities. A Recovery Audit Contractor (RAC) reviews claims and identifies overpayments from Medicare so that CMS and other auditors are able to prevent improper payments in the future.
The purpose of the Medicaid Administrative Claiming (MAC) program is to provide State affiliated public agencies in Texas the opportunity to submit reimbursement claims for administrative activities that support the Medicaid program.
Mid-arm circumference (MAC) is an important measure of nutritional status. Following a patient's nutritional status is key for establishing eligibility for hospice care.
RACs review claims on a post-payment basis and will be able to look back three years from the date the claim was paid.
A Medicare Administrative Contractor (MAC) is a private health care insurer that has been awarded a geographic jurisdiction to process Medicare Part A and Part B (A/B) medical claims or Durable Medical Equipment (DME) claims for Medicare Fee-For-Service (FFS) beneficiaries.
RACs are paid on a contingency fee basis, which means they are reimbursed based on a percentage of the improper payments they find or collect. The amount of the contingency fee is based on the amount of money from, or reimbursed to, providers.
RAC auditswhich may be triggered by an innocent documentation errorare not one-time or intermittent reviews. They are part of a systematic and concurrent operating process created to ensure compliance with Medicare's clinical payment criteria and documentation and billing requirements.
What does a Recovery Audit Contractor (RAC) do? RAC's review claims on a post-payment basis. The RAC's detect and correct past improper payments so that CMS and Carriers, FIs, and MACs can implement actions that will prevent future improper payments.
5 Ways You Can Begin Preparing for a RAC AuditPerform an Internal Audit. This action will help you to determine the likelihood of coding and billing mistakes within your company.Identify and Correct Coding/Billing Issues.Review Problem Areas.Check Documentation.Find Assistance.
They look for improper payments The aim of the Medicare Fee for Service Recovery Audit Program is to identify and fix incorrect and improper payments in a variety of healthcare fields, home health and hospice included. RAC looks for both overpayments made to patients and underpayments made to providers.