North Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
You can dedicate multiple hours online seeking the legal document template that meets your local and national requirements. US Legal Forms offers thousands of legal forms that can be reviewed by experts.
You can obtain or print the North Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage from this service.
If you have a US Legal Forms account, you can Log In and click on the Download button. Then, you can complete, modify, print, or sign the North Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. Each legal document template you acquire is yours permanently. To obtain another copy of the purchased form, go to the My documents tab and click on the appropriate button.
Select the format of the document and download it to your device. You can make edits to your document if applicable. You can complete, modify, sign, and print the North Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage. Access thousands of document templates using the US Legal Forms website, which offers the largest collection of legal forms. Utilize professional and state-specific templates to address your business or personal needs.
- If this is your first time using the US Legal Forms website, follow the simple instructions outlined below.
- First, make sure you have selected the correct document template for your area/city of choice. Review the form description to ensure you have chosen the right document.
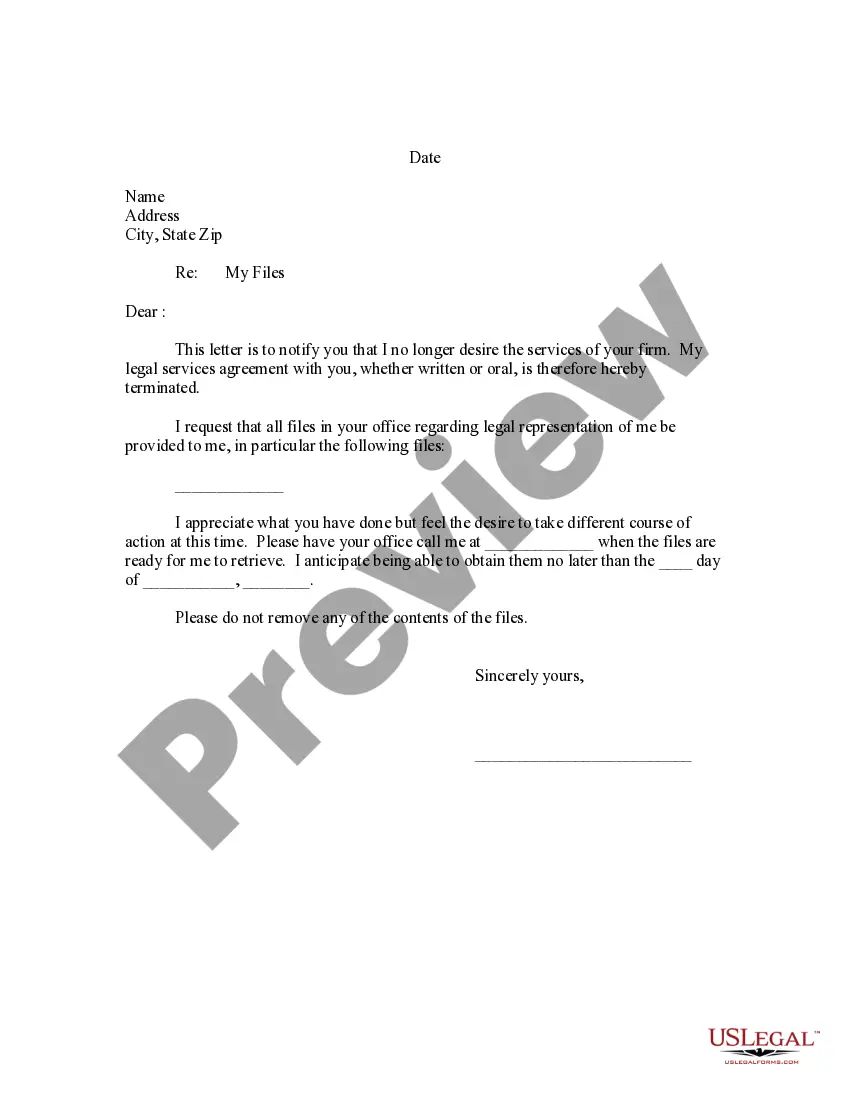
- If available, utilize the Preview button to view the document template as well.
- If you wish to find an alternate version of the form, use the Search field to locate the template that best suits your needs and requirements.
- Once you have found the template you need, click Buy now to continue.
- Select the pricing plan you prefer, enter your details, and create your account on US Legal Forms.
- Complete the payment. You can use your credit card or PayPal account to purchase the legal document.
Form popularity
FAQ
When a company provides continued health coverage after an employee is laid off, it is often referred to as COBRA or continuation coverage. Employees receiving this benefit can keep their insurance for a limited period, which is crucial during their job search. The North Carolina Notice from Employer to Employee Regarding Early Termination of Continuation Coverage clarifies the specifics of this coverage, ensuring employees understand their options.
If you are entitled to elect COBRA continuation coverage, you must be given an election period of at least 60 days (starting on the later of the date you are furnished the election notice or the date you would lose coverage) to choose whether or not to elect continuation coverage.
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be made available for a maximum period (18, 29, or 36 months).
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.