Montana Notice of Qualifying Event from Employer to Plan Administrator
Description
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
Have you ever been in a location where you must have documentation for business or personal purposes almost daily.
There are numerous legitimate document templates accessible online, but finding forms you can trust can be challenging.
US Legal Forms provides thousands of template options, including the Montana Notice of Qualifying Event from Employer to Plan Administrator, crafted to meet state and federal requirements.
Once you find the correct form, click on Acquire now.
Choose the pricing plan you prefer, complete the required information to create your account, and pay for the transaction using your PayPal or credit card.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- Then, you can download the Montana Notice of Qualifying Event from Employer to Plan Administrator template.
- If you do not have an account and wish to use US Legal Forms, follow these steps.
- Acquire the form you need and ensure it is for the correct region/county.
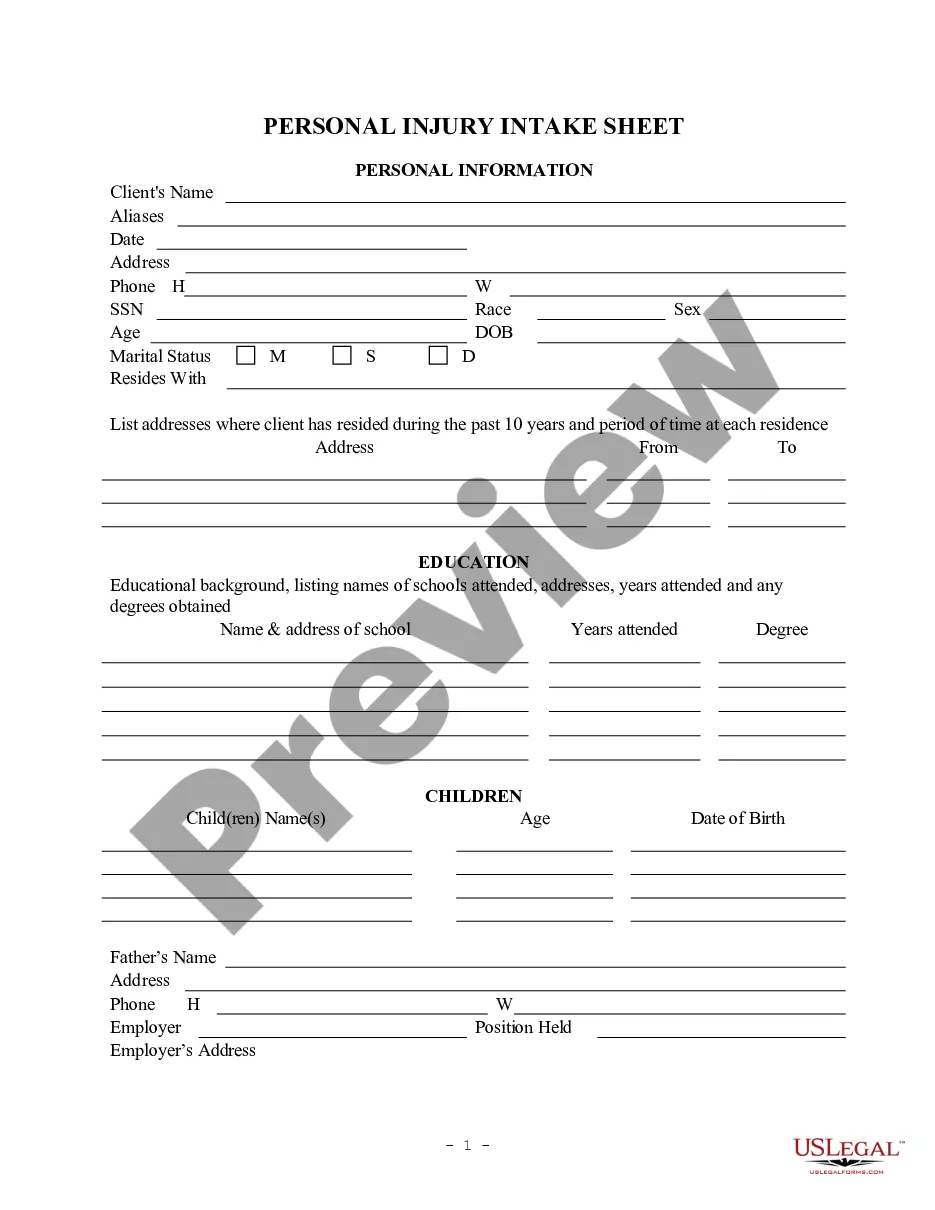
- Utilize the Review button to evaluate the form.
- Read the summary to ensure that you have selected the right form.
- If the form is not what you are looking for, use the Lookup field to find the template that meets your needs.
Form popularity
FAQ
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Yes, You Can Get COBRA Insurance After Quitting Your Job According to the Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA), companies with 20 or more employees are required to allow workers to keep their health insurance coverage, if that coverage would end due to a qualifying event.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
If you are laid-off or quit your job, COBRA will pay your health care costs up until 18 months following termination of employment. However, you must have both dental and vision coverage while employed if you want them covered by Cobra after quitting.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
Taking a leave of absence under the Family and Medical Leave Act of 1993 (FMLA) is not a COBRA qualifying event because FMLA requires a covered employer to maintain group health plan benefits for an employee so the employee has no coverage loss.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
A qualifying event is one that would cause an employee who had group health coverage to lose that coverage. Dropping coverage during open enrollment is not a qualifying event, although doing so in conjunction with a qualifying event such as divorce or legal separation triggers COBRA rights for the spouse.