Missouri Sample COBRA Enrollment and / or Waiver Letter
Description
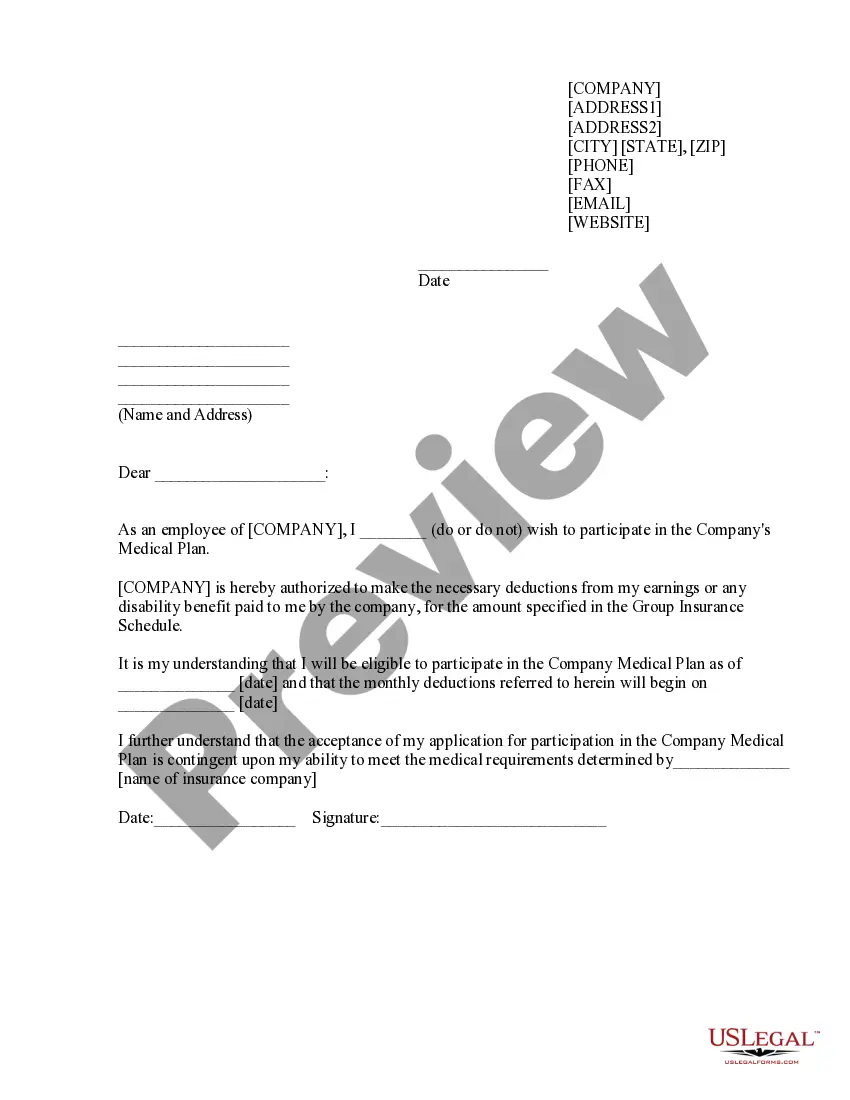
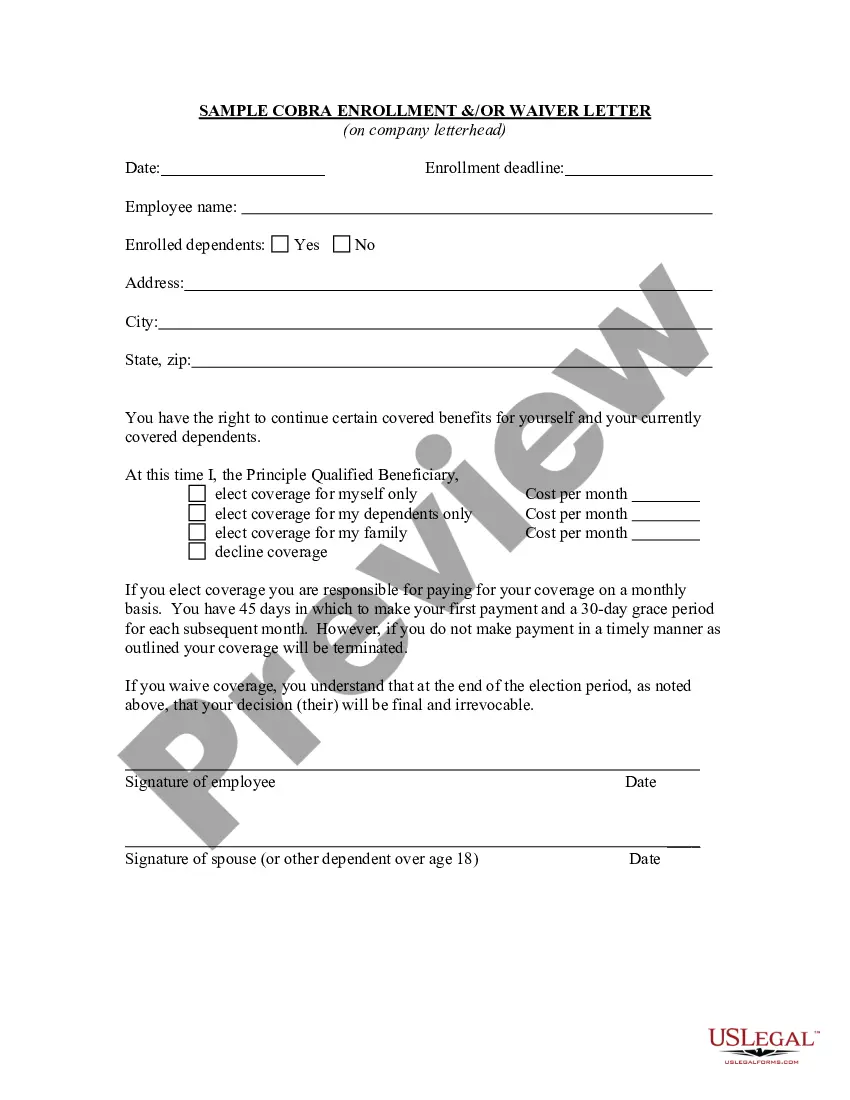
How to fill out Sample COBRA Enrollment And / Or Waiver Letter?
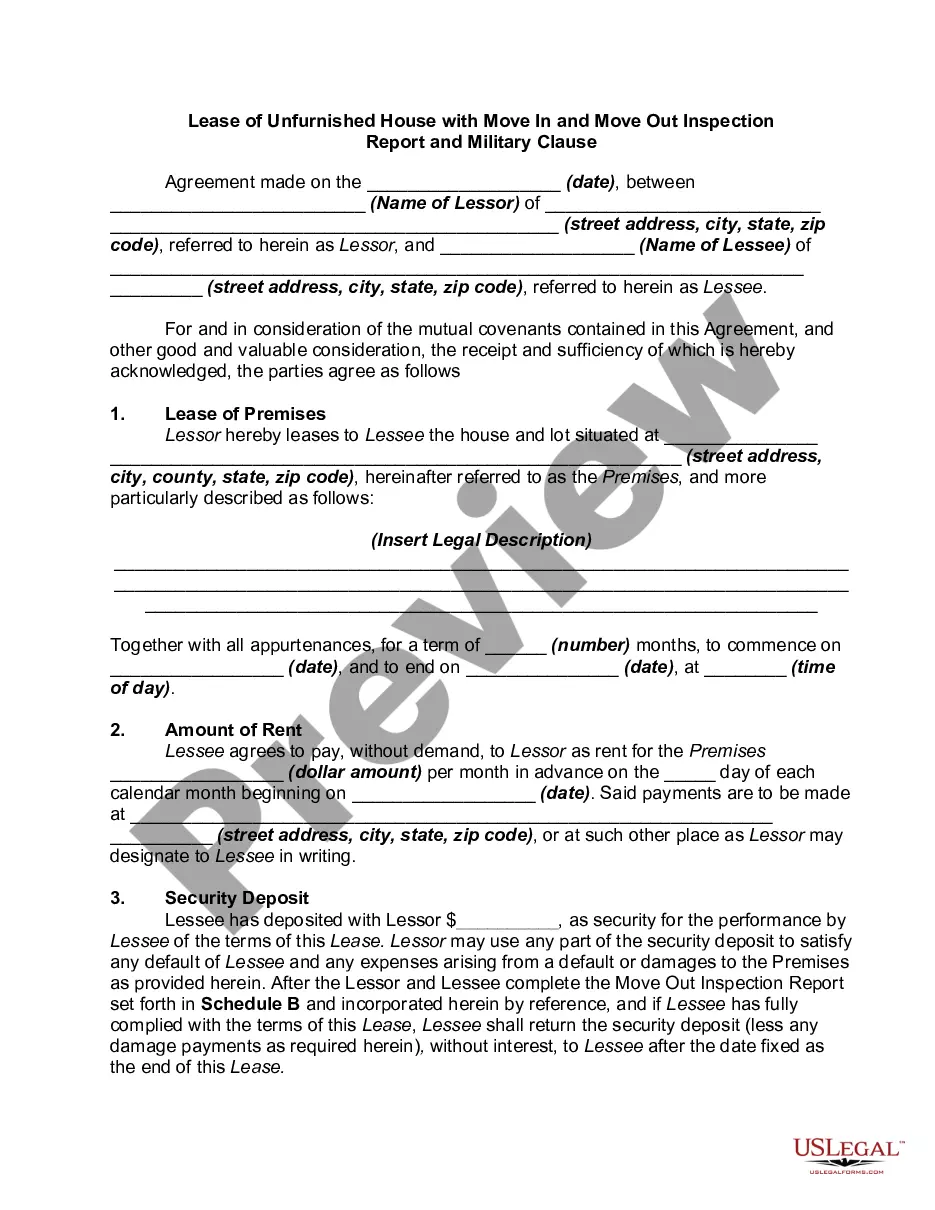
Selecting the optimal official document format can be a challenging task. Naturally, there are numerous templates available online, but how can you obtain the official form you need? Utilize the US Legal Forms website. The service offers thousands of templates, including the Missouri Sample COBRA Enrollment and/or Waiver Letter, that can be utilized for business and personal purposes.
All the forms are reviewed by experts and comply with federal and state requirements.
If you are already registered, Log In to your account and click the Download button to locate the Missouri Sample COBRA Enrollment and/or Waiver Letter. Use your account to search through the legal forms you have previously acquired. Navigate to the My documents tab in your account to obtain another copy of the document you need.
Complete, modify, and print and sign the acquired Missouri Sample COBRA Enrollment and/or Waiver Letter. US Legal Forms is the largest repository of legal forms where you can find various document templates. Use the service to download professionally-crafted paperwork that meets state requirements.
- If you are a new user of US Legal Forms, here are some simple instructions for you to follow.
- First, ensure you have selected the correct form for your city/region. You can review the form using the Preview button and read the form details to confirm it is the right one for you.
- If the form does not meet your requirements, use the Search field to find the suitable form.
- Once you are confident the form is appropriate, click on the Get now button to retrieve the form.
- Choose the pricing plan you prefer and enter the required information. Create your account and pay for your order using your PayPal account or credit card.
- Select the document format and download the official document template to your device.
Form popularity
FAQ
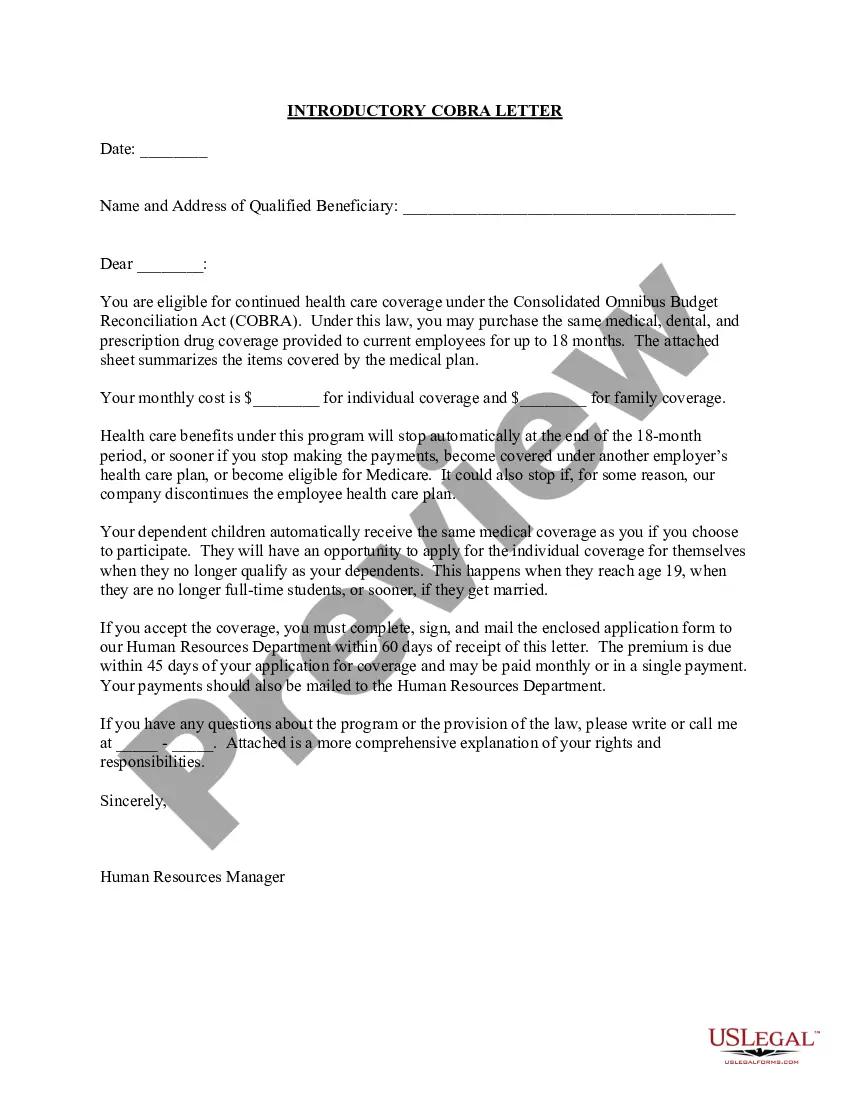
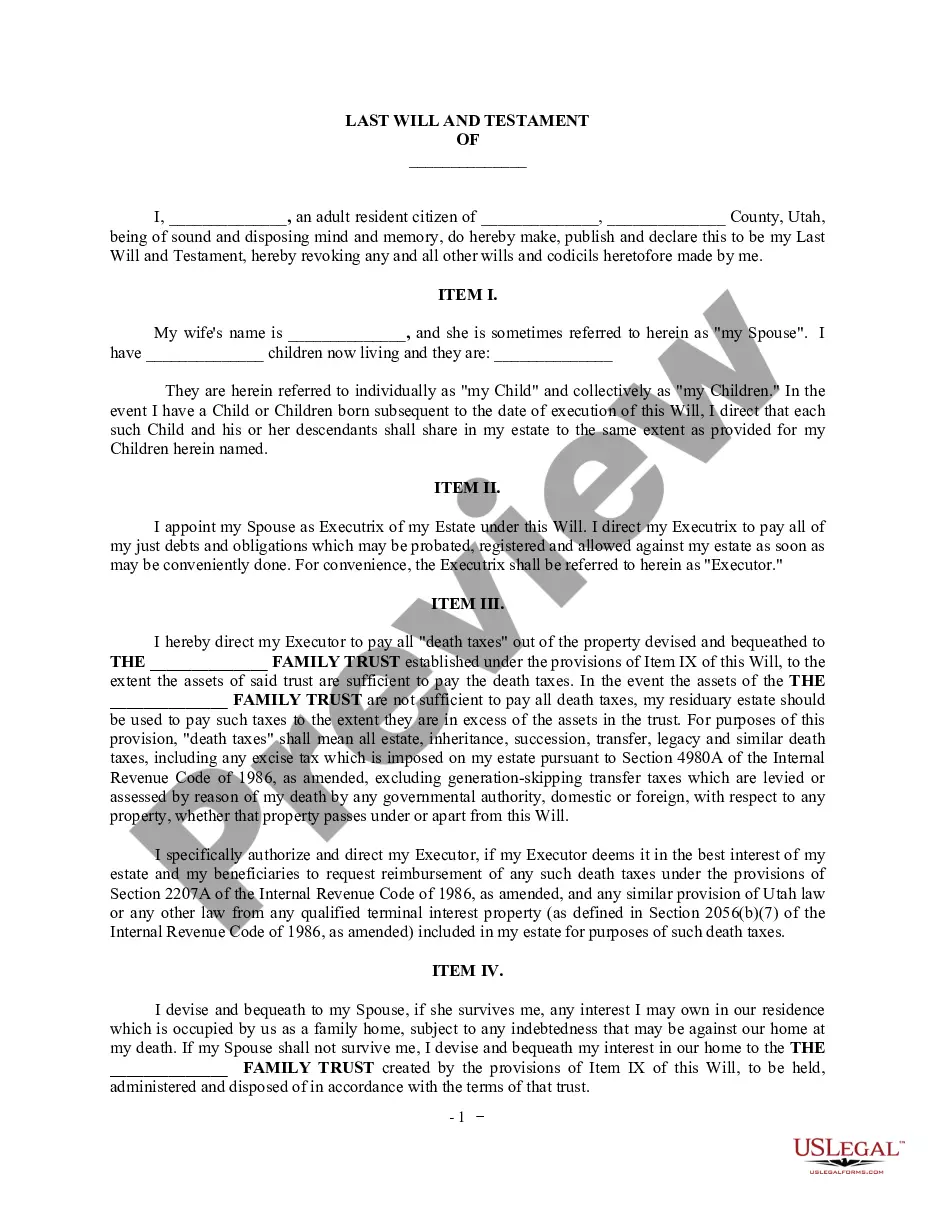
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a landmark federal law, passed in 1985, that provides for continuing group health insurance coverage for some employees and their families after a job loss or other qualifying event.
Failure to pay premiums. When a participant fails to make a timely payment of any required COBRA premium, the employer may terminate COBRA coverage. Employers must provide participants with at least a 30-day grace period for payment of any late premiums.
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
The purpose of this letter is to inform you of your rights and responsibilities as a plan participant. Qualifying Event: At the end of your employment or because of reduction of hours (not maintain full-time status) you will receive this letter.
Although the earlier rules only covered summary plan descriptions (SPDs) and summary annual reports, the final rules provide that all ERISA-required disclosure documents can be sent electronically -- this includes COBRA notices as well as certificates of creditable coverage under the Health Insurance Portability and
The initial notice, also referred to as the general notice, communicates general COBRA rights and obligations to each covered employee (and his or her spouse) who becomes covered under the group health plan.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The COBRA Notice informs the qualified beneficiary of their rights under COBRA law, and the form allows the qualified beneficiary to elect COBRA coverage to continue enrollment in benefits.