Missouri Services Request Cover Sheet
Description
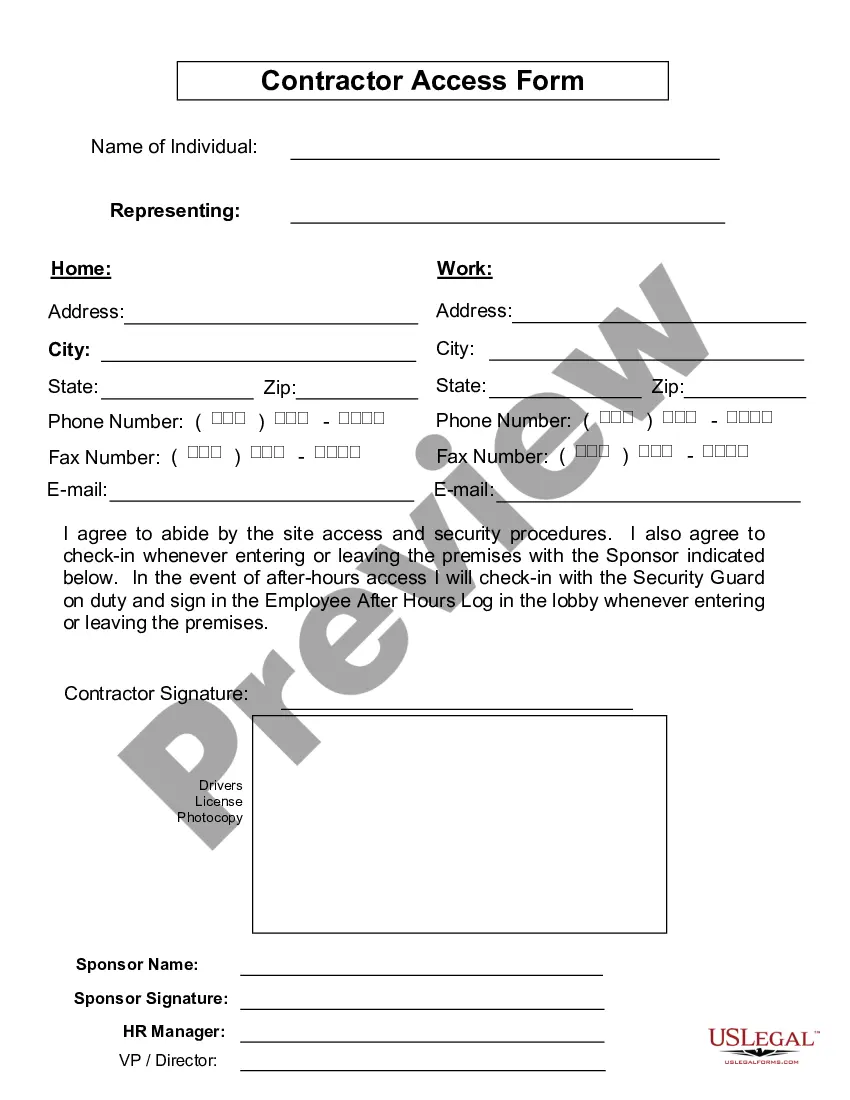
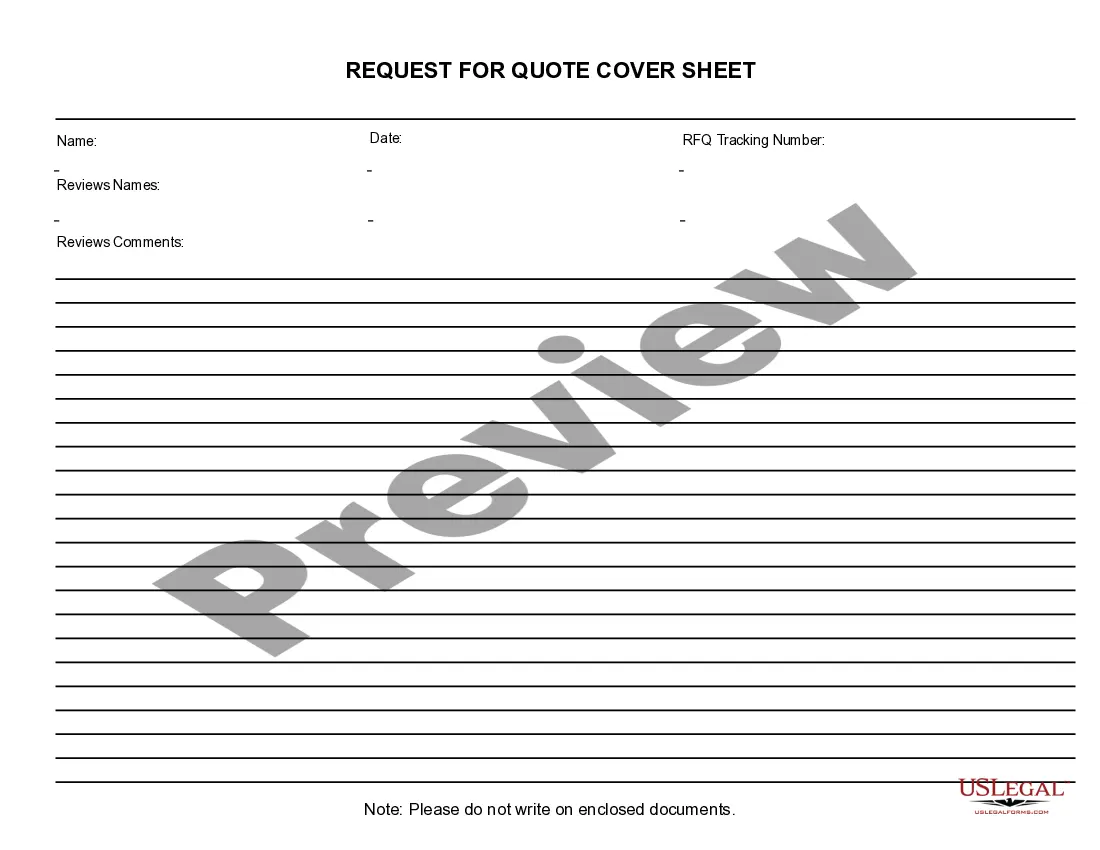
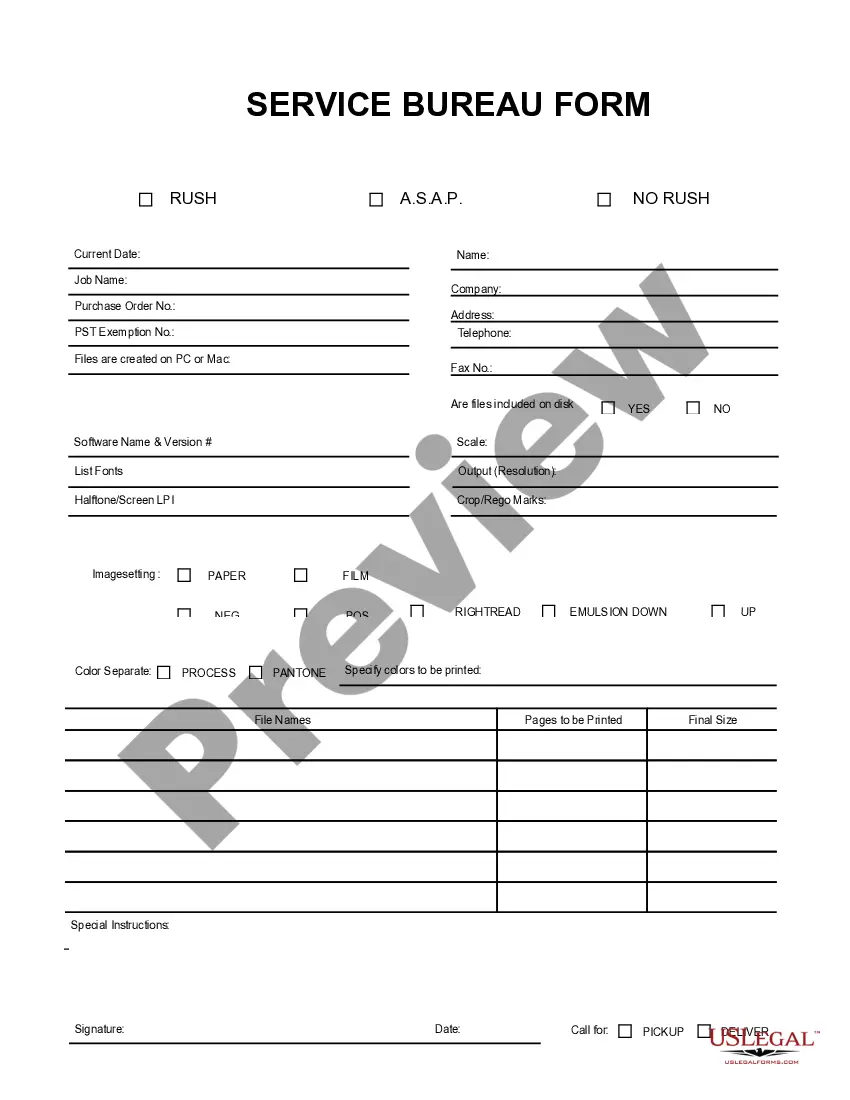
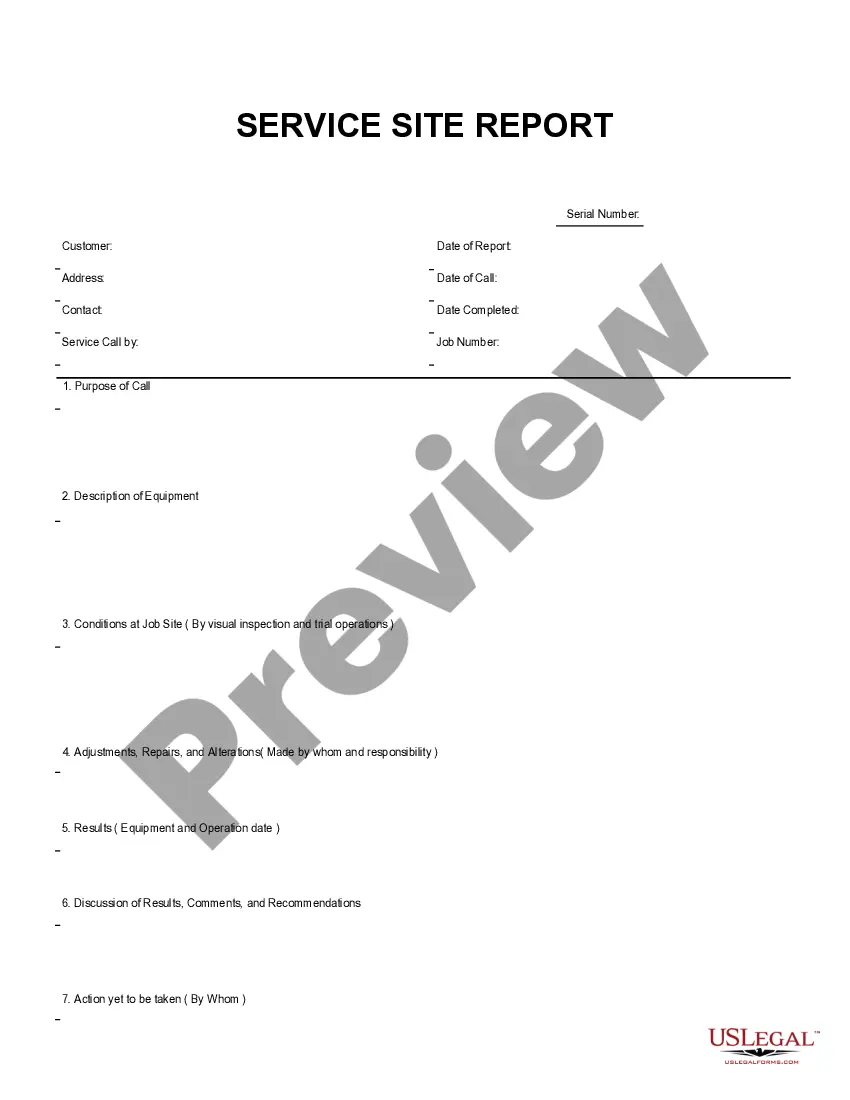
How to fill out Services Request Cover Sheet?
Choosing the best lawful record format can be quite a battle. Obviously, there are tons of templates available on the net, but how will you get the lawful form you want? Make use of the US Legal Forms internet site. The service offers a large number of templates, including the Missouri Services Request Cover Sheet, which can be used for business and personal requirements. All the kinds are inspected by pros and fulfill state and federal specifications.
When you are previously listed, log in for your bank account and then click the Down load button to obtain the Missouri Services Request Cover Sheet. Utilize your bank account to look from the lawful kinds you may have purchased formerly. Visit the My Forms tab of your own bank account and get another duplicate of your record you want.
When you are a whole new customer of US Legal Forms, here are easy recommendations that you should follow:
- Initially, make certain you have selected the correct form for the area/region. You are able to examine the shape using the Review button and look at the shape outline to guarantee it will be the best for you.
- If the form will not fulfill your preferences, make use of the Seach area to get the correct form.
- Once you are certain that the shape would work, select the Purchase now button to obtain the form.
- Choose the rates strategy you would like and enter in the necessary information and facts. Design your bank account and pay for your order with your PayPal bank account or bank card.
- Choose the data file structure and download the lawful record format for your product.
- Complete, change and print out and indication the received Missouri Services Request Cover Sheet.
US Legal Forms is definitely the biggest collection of lawful kinds in which you can find various record templates. Make use of the service to download expertly-produced documents that follow status specifications.
Form popularity
FAQ
MO HealthNet eligibility may be verified through the following eligibility verification system 24 hours per day, 7 days per week: Interactive Voice Response (IVR) system, 1-573/751-2896, option 1. Internet at emomed.com.
A Missouri Medicaid prior authorization form is used by a prescribing medical provider to request treatment that is not covered by their patient's state health care plan.
If you do not have health insurance or you need help paying for your health care, you may be eligible for coverage through Missouri's Medicaid program, called MO HealthNet.
Apply for help online, manage your benefits, or start a chat by visiting myDSS.mo.gov. Schedule an appointment to visit an office nearest you (offices are located in each of the 114 counties of the state and in the city of St. Louis) Call 855-FSD-INFO (855-373-4636) to speak with a team member.
Pharmacy Help Desk, Drug Prior Authorization, Diabetic Supply Prior Authorization, Durable Medical Equipment (DME) Smart PA's, and Med Solution precertification Process: 1-800-392-8030.
Out-of-network physicians, facilities and other health care providers must request prior authorization for all procedures and services, excluding emergent or urgent care. Many of our benefit plans provide coverage for behavioral health services through a designated behavioral health network.
Prior authorization (prior auth, or PA) is a management process used by insurance companies to determine if a prescribed product or service will be covered. This means if the product or service will be paid for in full or in part.