Minnesota Acknowledgment of Receipt of COBRA Notice
Description
How to fill out Acknowledgment Of Receipt Of COBRA Notice?
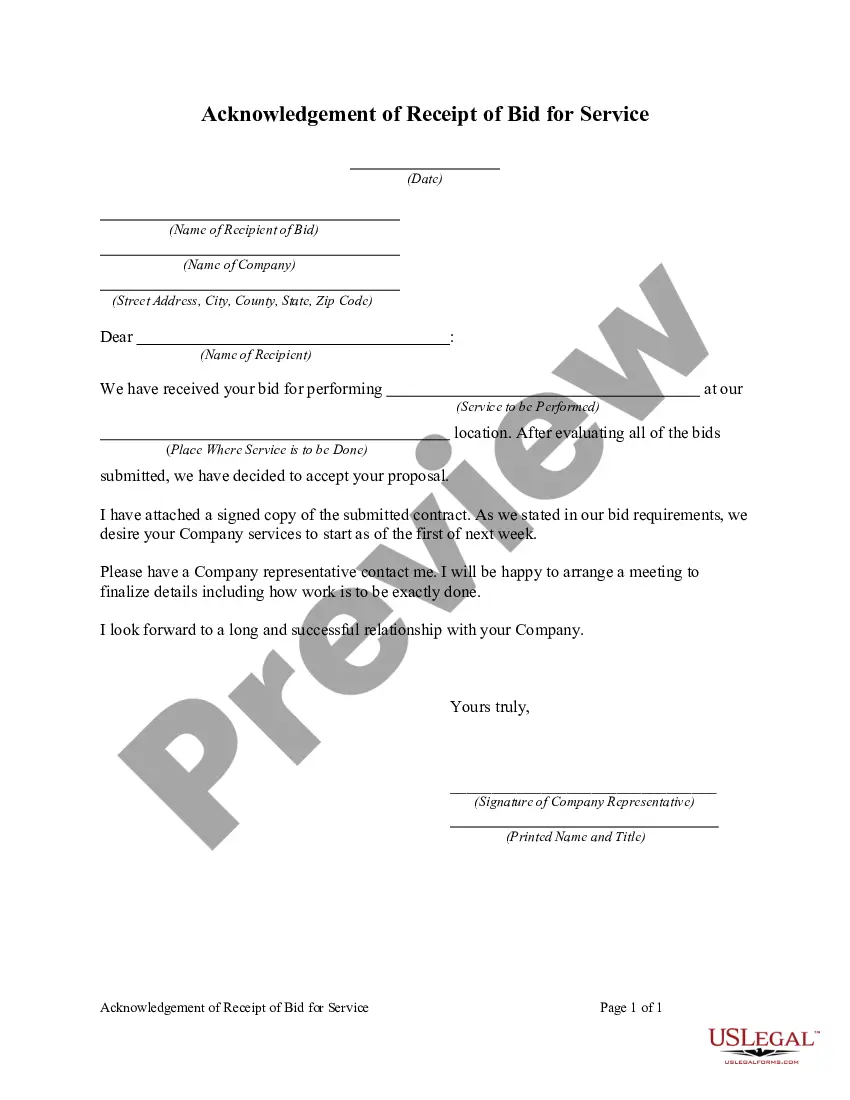
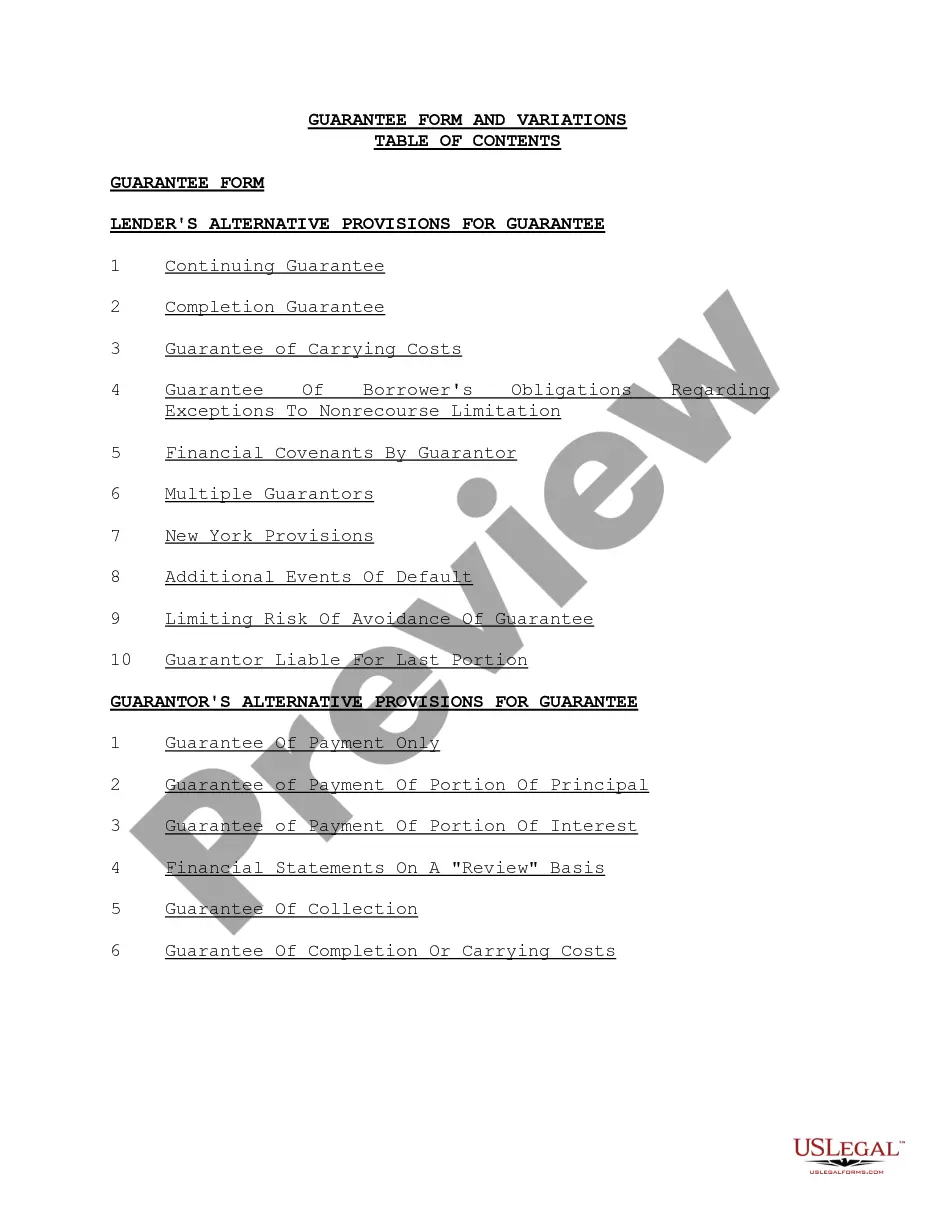
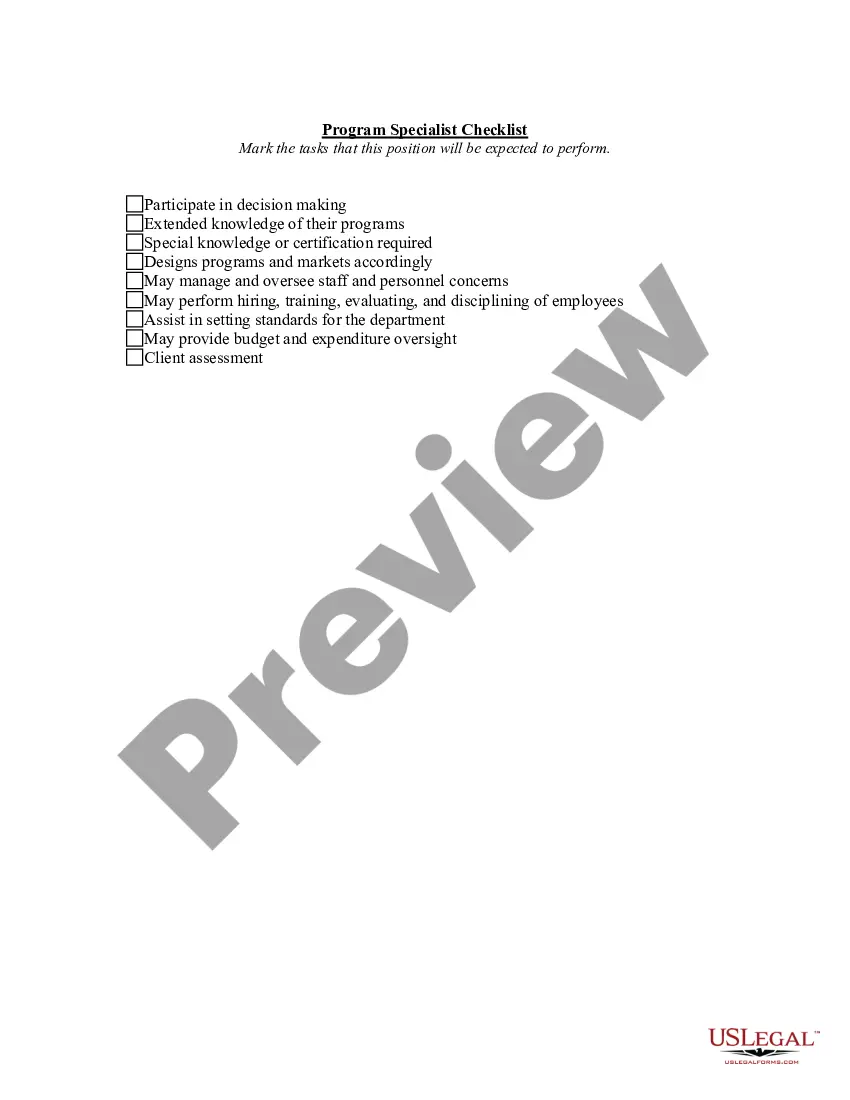
You can invest multiple hours online trying to locate the legal document template that meets the federal and state requirements you need.
US Legal Forms offers a multitude of legal forms that are vetted by experts.
You can download or print the Minnesota Acknowledgment of Receipt of COBRA Notice from our service.
If available, utilize the Review button to browse through the document template as well. If you wish to find another version of the form, use the Search field to locate the template that suits your needs and requirements.
- If you possess a US Legal Forms account, you can Log In and click the Acquire button.
- Afterwards, you can complete, modify, print, or sign the Minnesota Acknowledgment of Receipt of COBRA Notice.
- Every legal document template you buy is yours indefinitely.
- To obtain another copy of a purchased form, go to the My documents tab and click the appropriate button.
- If you are using the US Legal Forms site for the first time, follow the simple instructions below.
- First, ensure that you have selected the correct document template for the county/region of your choice.
- Review the form details to confirm you have chosen the correct form.
Form popularity
FAQ
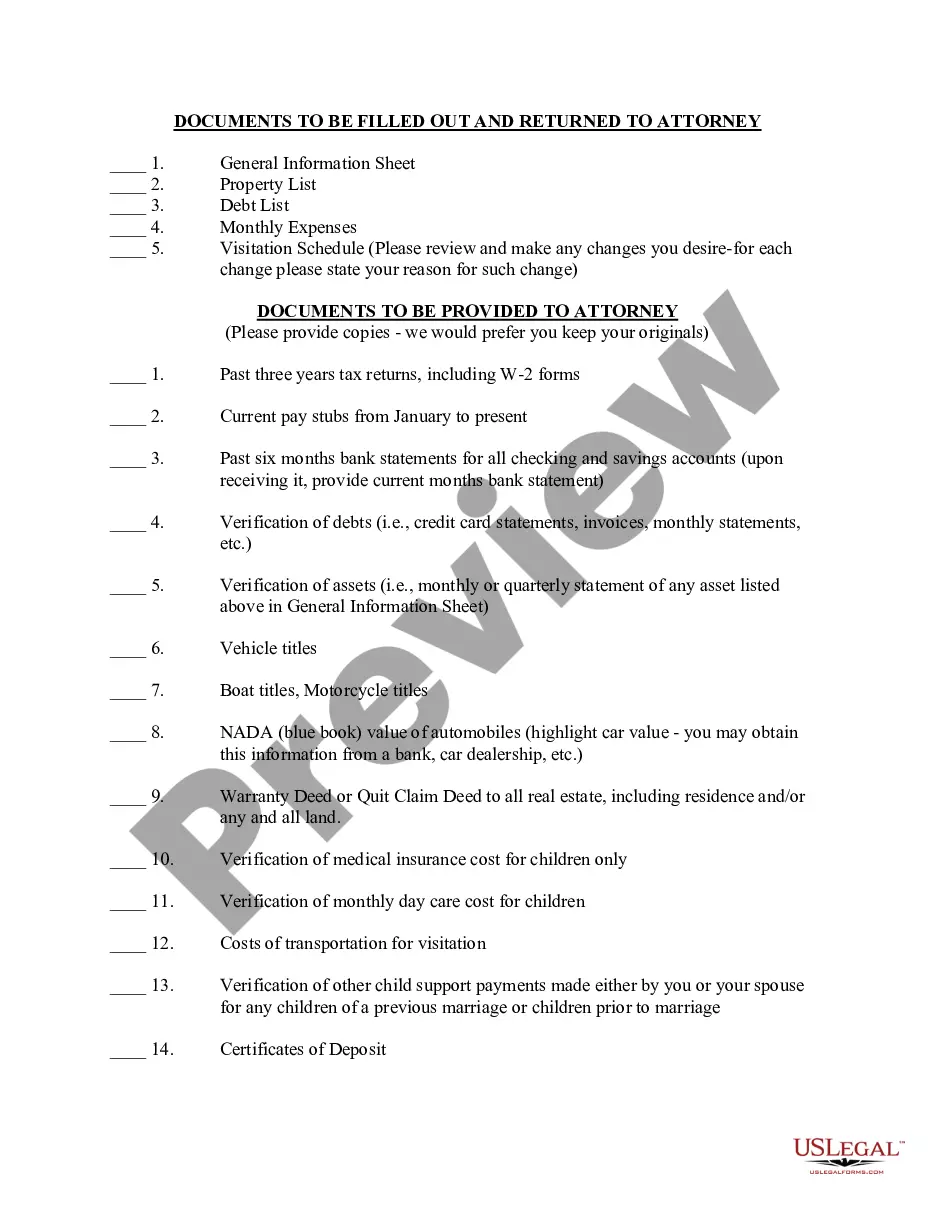
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
Key Takeaways. COBRA provides a good option for keeping your employer-sponsored health plan for a while after you leave your job. Although, the cost can be high. Make an informed choice by looking at all your options during the 60-day enrollment period, and don't focus on the premium alone.
Employers should send notices by first-class mail, obtain a certificate of mailing from the post office, and keep a log of letters sent. Certified mailing should be avoided, as a returned receipt with no delivery acceptance signature proves the participant did not receive the required notice.
COBRA Notice of Early Termination of Continuation Coverage Continuation coverage must generally be made available for a maximum period (18, 29, or 36 months).
If You Do Not Receive Your COBRA PaperworkReach out to the Human Resources Department and ask for the COBRA Administrator. They may use a third-party administrator to handle your enrollment. If the employer still does not comply you can call the Department of Labor at 1-866-487-2365.
How long does it take for COBRA to kick in? With all paperwork properly submitted, your COBRA coverage should begin on the first day of your qualifying event (for example, the first day you are no longer with your employer), ensuring no gaps in your coverage.
Although the earlier rules only covered summary plan descriptions (SPDs) and summary annual reports, the final rules provide that all ERISA-required disclosure documents can be sent electronically -- this includes COBRA notices as well as certificates of creditable coverage under the Health Insurance Portability and
If you are enrolled on your parent's coverage and turn 26, you are eligible to continue Medical and Dental benefits on COBRA for 36 months. Your first day of COBRA coverage will be the first of the month following the date you turn 26.
In addition, employers can provide COBRA notices electronically (via email, text message, or through a website) during the Outbreak Period, if they reasonably believe that plan participants and beneficiaries have access to these electronic mediums.
The length of COBRA continuation depends upon the qualifying event: When the qualifying event is a dependent child losing eligibility as a dependent child, continuation lasts for up to 36 months. When the qualifying event is the death of the employee or divorce or legal separation, continuation may last indefinitely.