Under the Health Insurance Portability and Accountability Act of 1996 (HIPAA) and the Privacy Regulations written pursuant to the Act, the general rule is that covered entities may not use or disclose an individual's protected health information for purposes unrelated to treatment, payment, healthcare operations, or certain defined exceptions without first obtaining the individual's prior written authorization.
Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508
Description
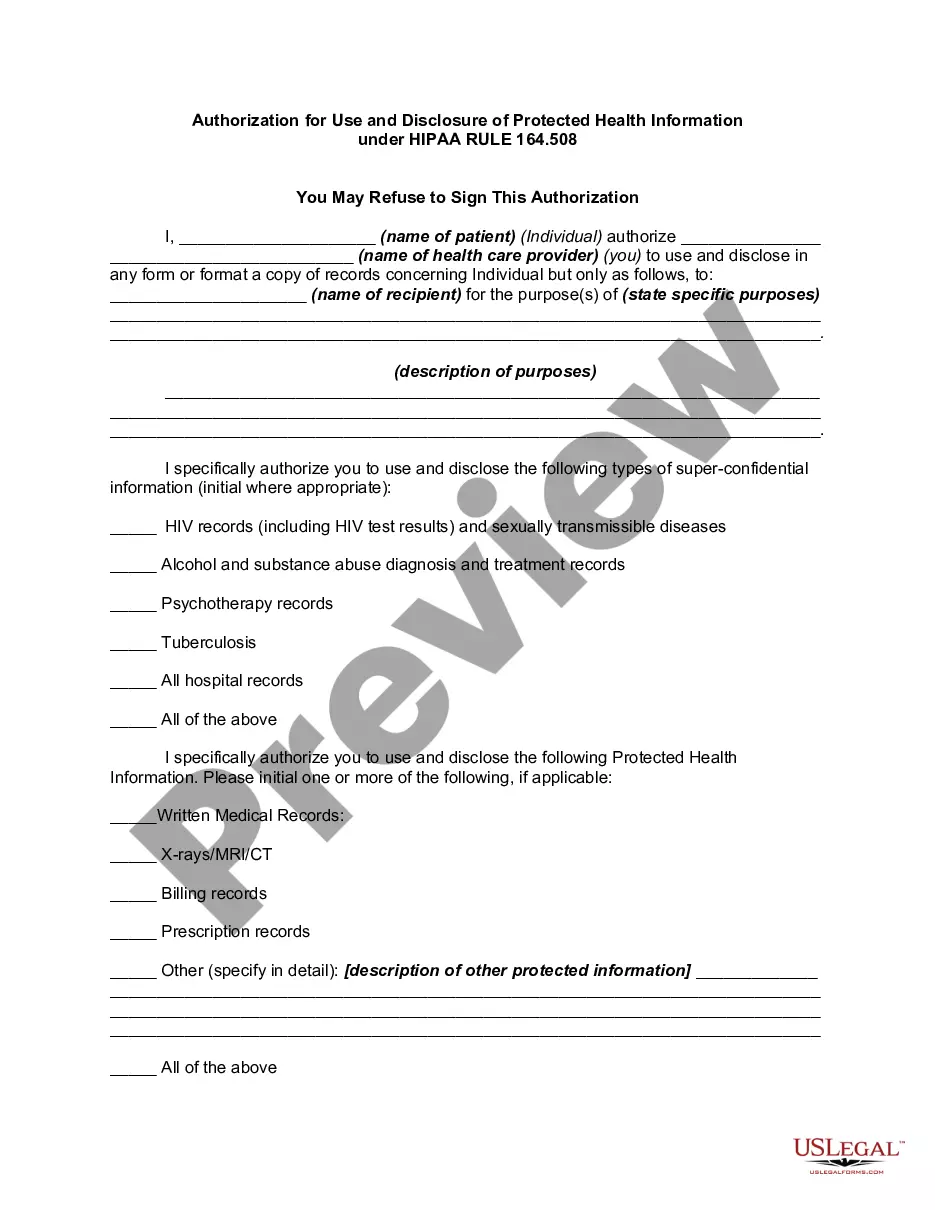
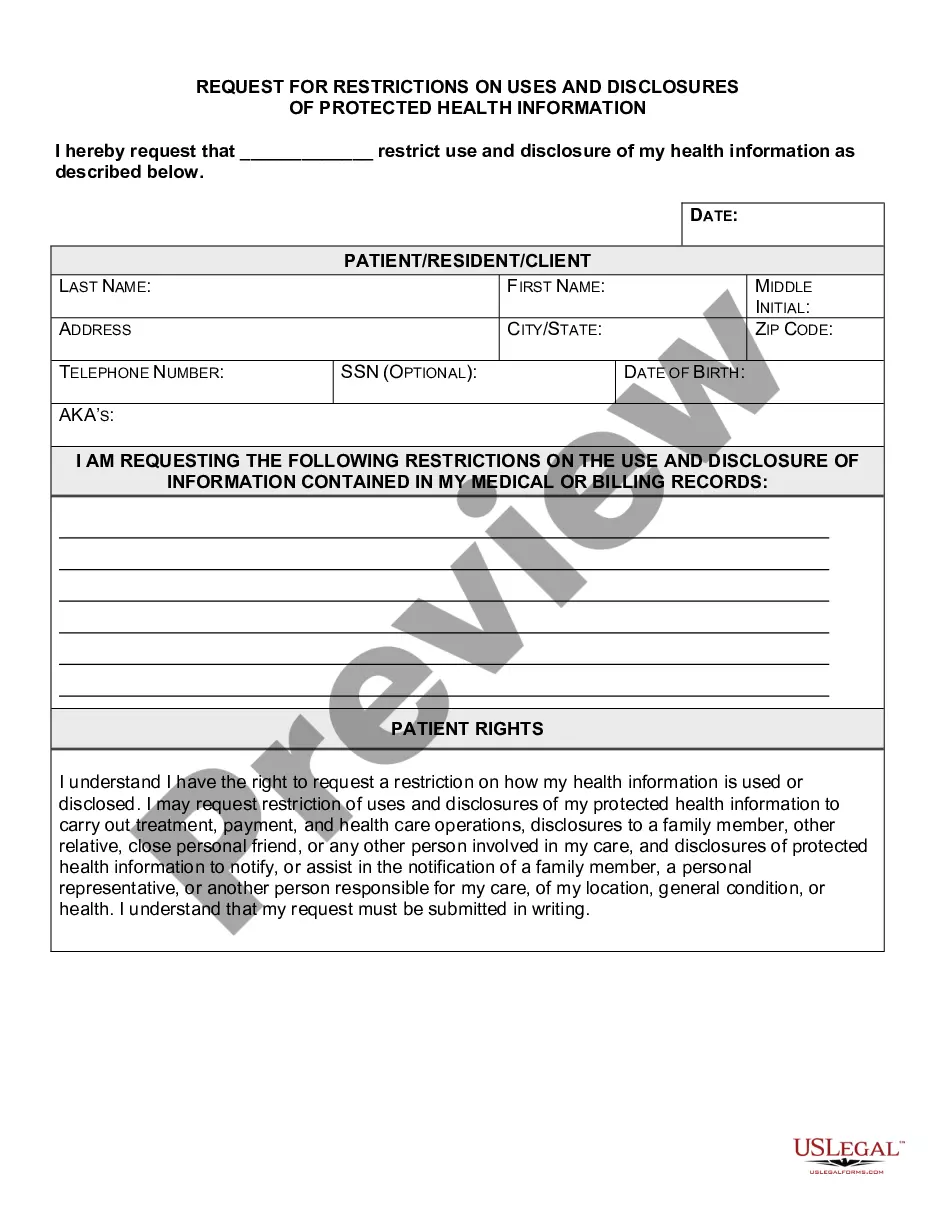
How to fill out Authorization For Use And Disclosure Of Protected Health Information Under HIPAA RULE 164.508?
It is feasible to invest time online looking for the legal document template that meets federal and state regulations that you require.
US Legal Forms provides thousands of legal documents that have been evaluated by experts.
You can easily download or print the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 from our service.
If available, use the Preview button to review the document template as well.
- If you already have a US Legal Forms account, you can Log In and click the Obtain button.
- Then, you can complete, edit, print, or sign the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508.
- Every legal document template you receive is yours permanently.
- To obtain another copy of any purchased form, navigate to the My documents tab and click the corresponding button.
- If you are visiting the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure you have selected the correct document template for the state/city of your choice.
- Review the form description to confirm you have chosen the right form.
Form popularity
FAQ
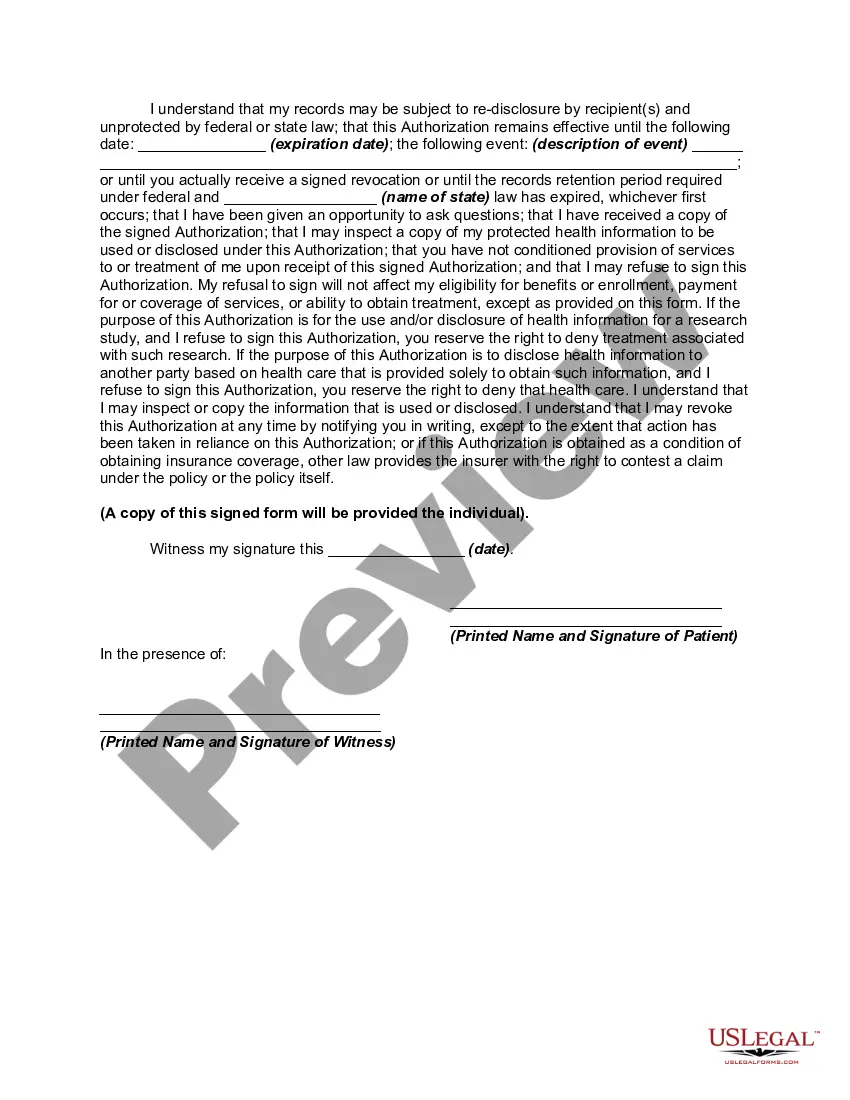
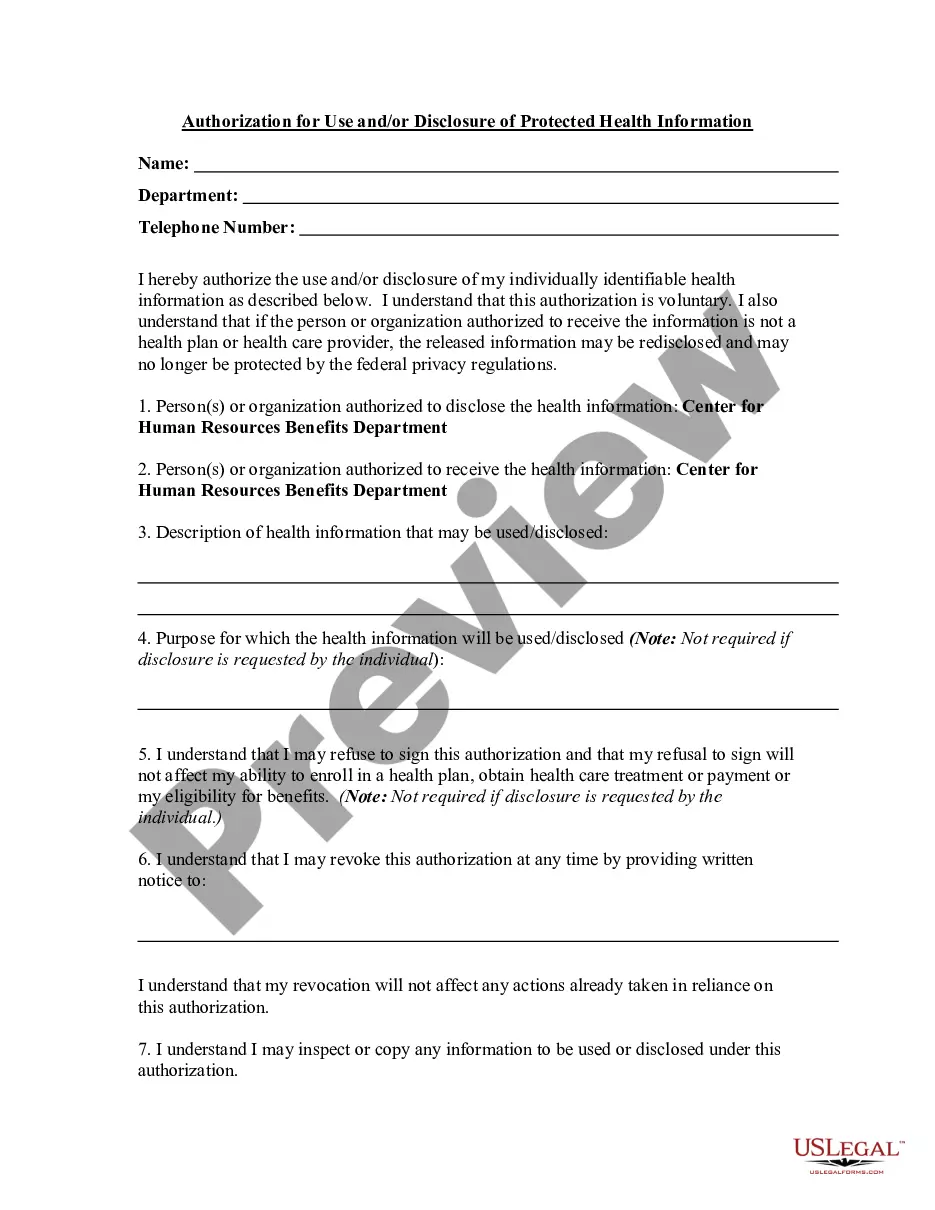
Under HIPAA, the authorization for the use and disclosure of protected health information must clearly state what information will be shared, with whom, and for what purpose. The Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 provides a comprehensive framework for this process. It helps ensure that your private health details remain confidential unless you provide explicit consent for their release. Utilizing a platform like USLegalForms can simplify the creation of this authorization, ensuring compliance with HIPAA regulations.
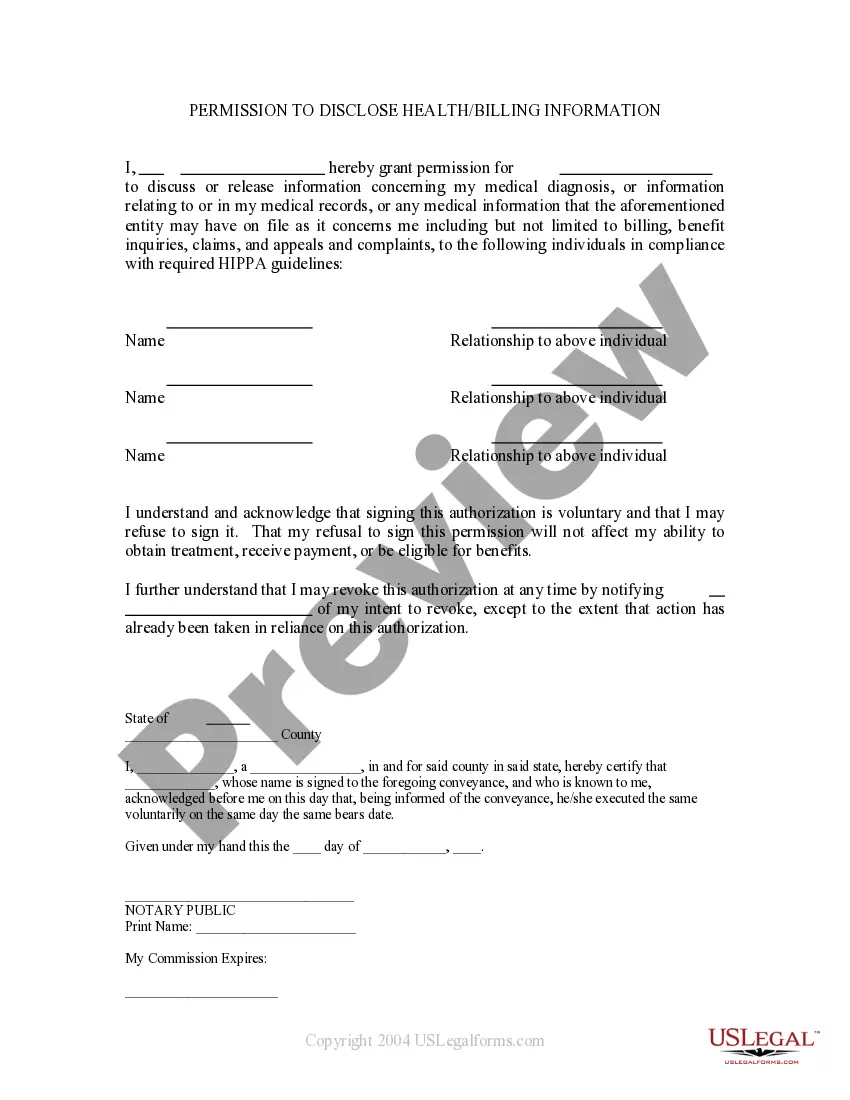
In the context of healthcare, any disclosure of a patient's health information that goes beyond treatment, payment, or healthcare operations generally requires the patient's authorization. This includes sharing personal health information with third parties for purposes such as marketing or research. Specifically, the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 lays out the legal standards and requirements for obtaining this consent, ensuring that your rights are protected.
To obtain HIPAA approval, start by completing the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 correctly. It’s vital to follow the required procedures and keep detailed records. Furthermore, you can leverage the resources available on the USLegalForms platform to ensure your application meets all necessary standards and regulations.
A patient's authorization for disclosure of PHI, such as the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, is a legal document. It allows healthcare providers to share patient information with designated third parties. This authorization is essential to ensure compliance with HIPAA regulations while safeguarding patient privacy.
Deciding whether to accept or decline HIPAA authorization depends on the specific circumstances. If you believe the disclosure of information is necessary for the patient's care, you may proceed with the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508. However, if you're uncertain about the implications or the type of information involved, it’s wise to seek legal advice.
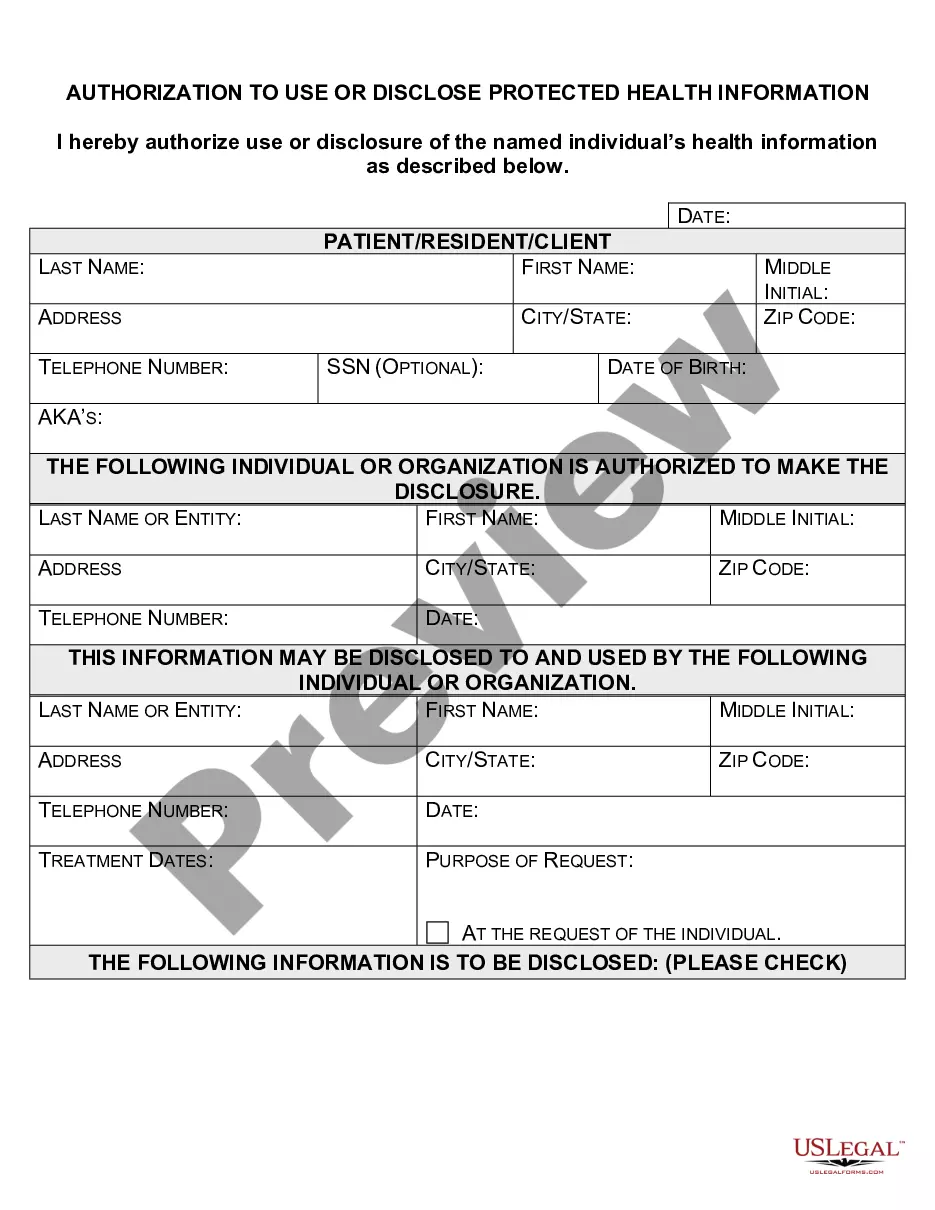
Filling out the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 involves several key steps. First, ensure you provide accurate patient information, including the full name and date of birth. Next, clearly specify the type of information to be disclosed and identify the recipient. Finally, sign and date the form to validate the authorization.
When HIPAA requires authorization to disclose information, the authorization must specify the purpose of the disclosure and list the information that will be shared. Additionally, the patient must sign this authorization, indicating their agreement. By following the guidelines established in the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508, healthcare providers can ensure that they are compliant with legal standards.
The four types of PHI include demographic information, medical history, healthcare provider details, and payment information. Each category plays a crucial role in healthcare operations and requires careful management under the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508. Recognizing these categories helps in maintaining compliance and protecting patient confidentiality.
HIPAA requires signed authorization for use or disclosure of any PHI that is not essential for treatments, payment, or healthcare operations. This often encompasses detailed medical records, psychotherapy notes, and any non-routine disclosures. It is vital to utilize the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508 to define the boundaries of such disclosures.
HIPAA requires a signed authorization for various types of PHI, especially when it involves sensitive medical records and mental health information. This includes patient diagnoses, treatment information, and any billing records that are not standard for healthcare operations. Understanding this requirement is essential to comply with the Minnesota Authorization for Use and Disclosure of Protected Health Information under HIPAA RULE 164.508.