Louisiana Notice of Qualifying Event from Employer to Plan Administrator
Description
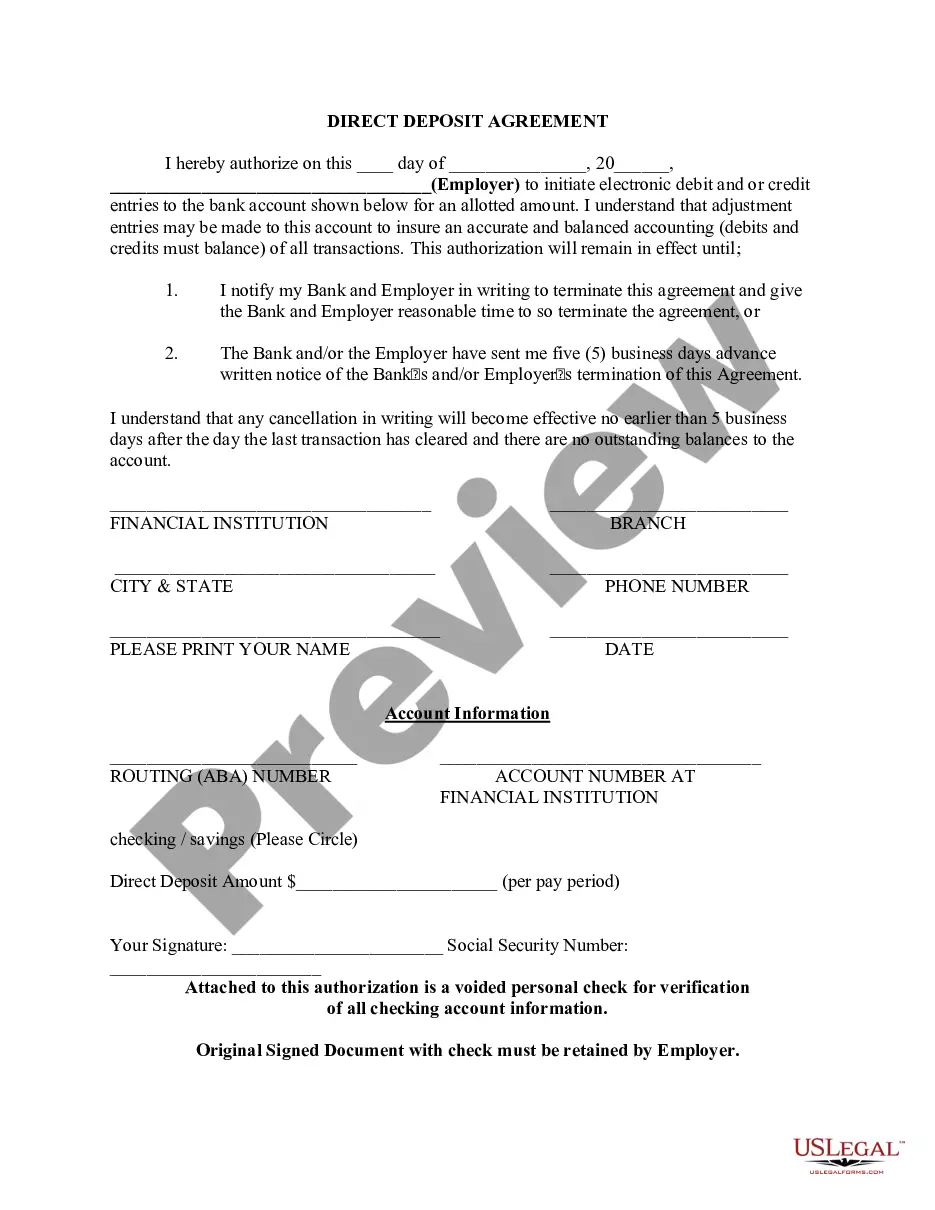
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
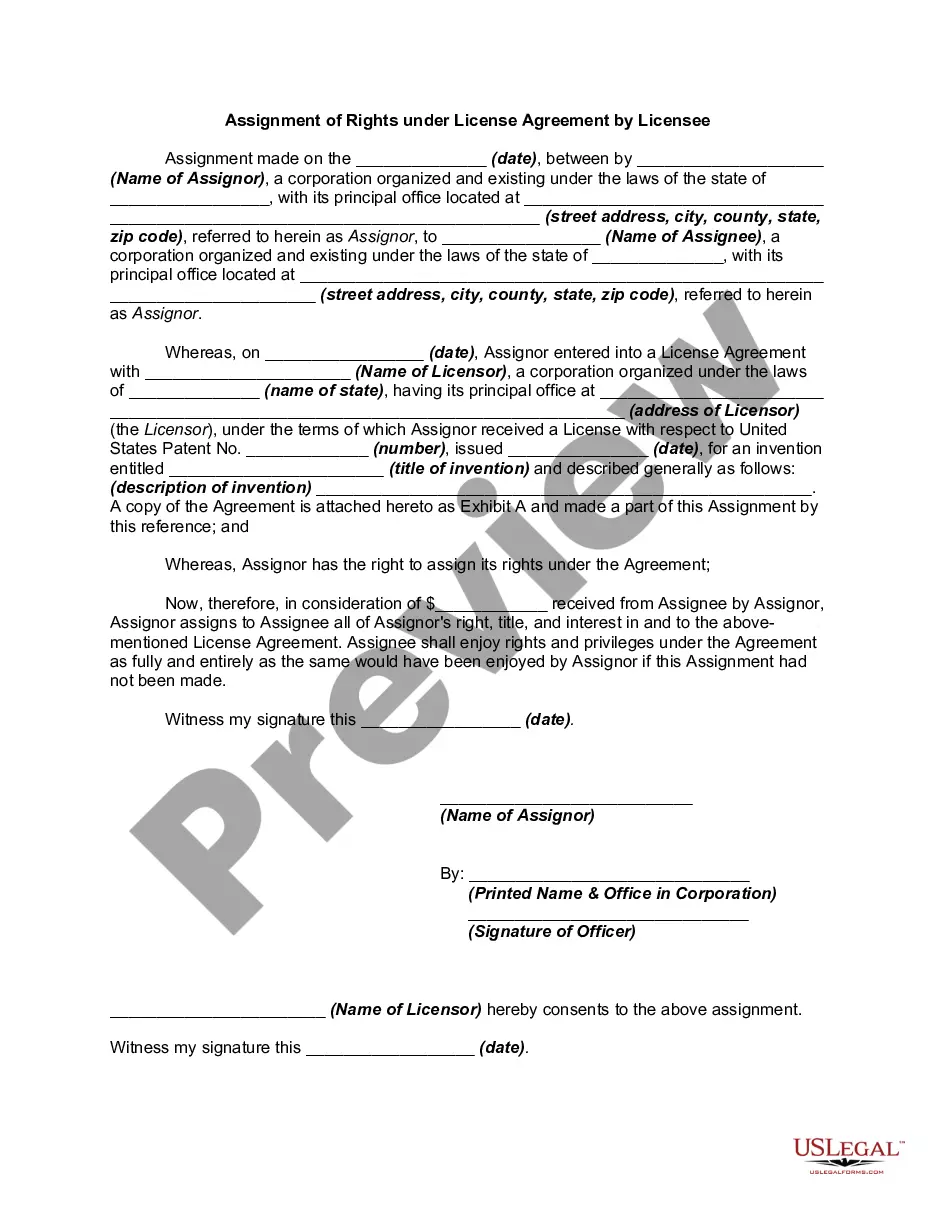
You can spend time online searching for the appropriate legal document template that meets the state and federal requirements you need.
US Legal Forms offers thousands of legal forms that can be reviewed by experts.
It's easy to download or print the Louisiana Notice of Qualifying Event from Employer to Plan Administrator through my service.
First, ensure that you have selected the correct document template for the region you choose. Review the form summary to confirm you have picked the right template. If available, use the Preview option to browse through the document template as well.
- If you already possess a US Legal Forms account, you can Log In and select the Download option.
- Then, you can fill out, modify, print, or sign the Louisiana Notice of Qualifying Event from Employer to Plan Administrator.
- Every legal document template you obtain is yours permanently.
- To retrieve another copy of the purchased form, go to the My documents section and click the appropriate option.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
Form popularity
FAQ
Yes, you can cancel COBRA coverage, but obtaining a refund may depend on specific conditions. If you decide to cancel after making a premium payment, you might not receive a refund for the unused portion of the coverage. It's important to notify your employer or the plan administrator promptly after you cancel. For guidance on the process, you can refer to the Louisiana Notice of Qualifying Event from Employer to Plan Administrator, which outlines the necessary steps and your rights in such situations.
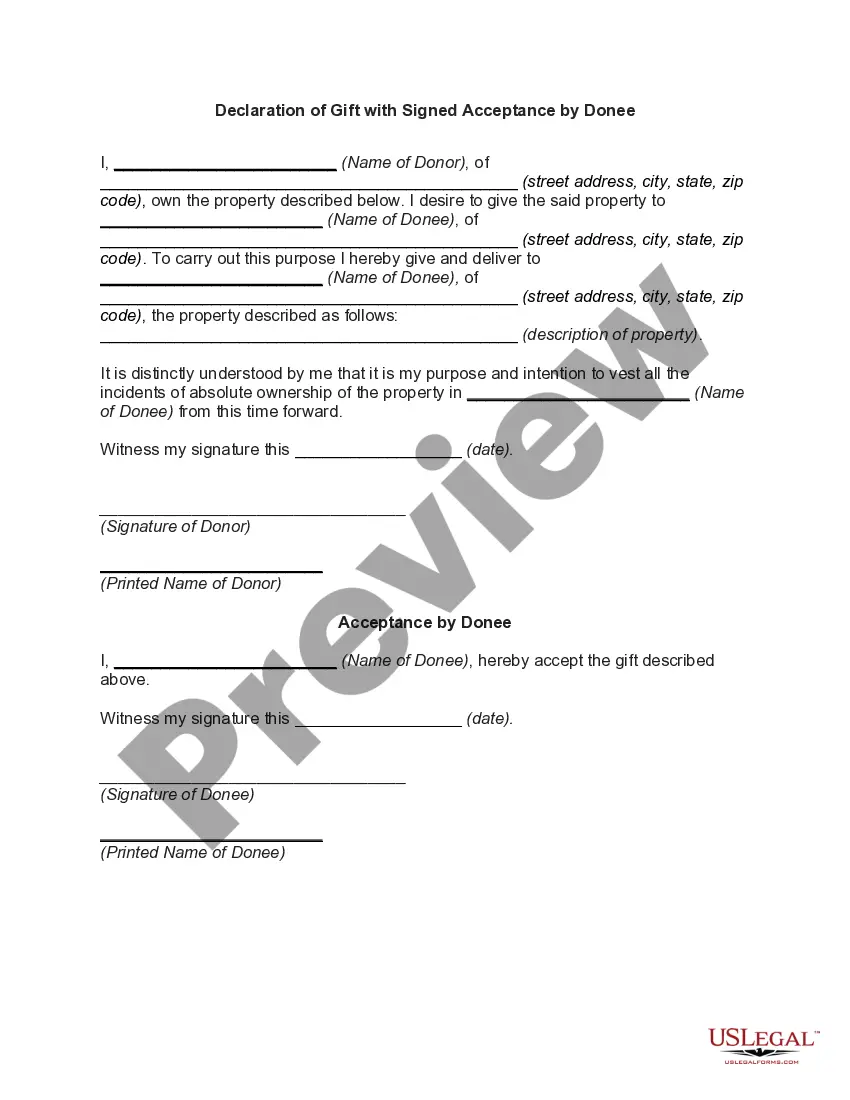
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
What Is The ACA Waiting Period? The Affordable Care Act (ACA) mandates that employers cannot wait more than 90 calendar days to offer health insurance coverages to eligible employees. This is called the 90-day waiting period limitation.
Part-time employee eligibility to participate in a company's retirement plan must comply with the Employee Retirement Income Security Act (ERISA) "1,000-hour rule." Employees who have completed 1,000 hours of service in a 12-month period are eligible to participate in any retirement plan that is offered to other
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.