Louisiana Affidavit of No Coverage by Another Group Health Plan
Description
How to fill out Affidavit Of No Coverage By Another Group Health Plan?
US Legal Forms - one of the largest collections of legal documents in the United States - offers a variety of legal form templates that you can download or print.
By utilizing the website, you can access thousands of forms for business and personal purposes, organized by categories, states, or keywords. You can retrieve the latest versions of forms like the Louisiana Affidavit of No Coverage by Another Group Health Plan within moments.
If you have an account, Log In and download the Louisiana Affidavit of No Coverage by Another Group Health Plan from the US Legal Forms catalog. The Download button will be visible on each form you review. You can find all previously downloaded forms in the My documents section of your account.
Process the transaction. Use a credit card or PayPal account to complete the payment.
Select the format and download the form to your device. Edit. Fill out, modify, print, and sign the downloaded Louisiana Affidavit of No Coverage by Another Group Health Plan. Each template you add to your account does not expire, meaning it's yours forever. Therefore, to download or print another copy, simply navigate to the My documents section and click on the form you need. Access the Louisiana Affidavit of No Coverage by Another Group Health Plan through US Legal Forms, one of the most extensive collections of legal document templates. Utilize thousands of professional and state-specific templates that meet your business or personal needs and requirements.
- Follow these simple steps to start using US Legal Forms for the first time.
- Make sure you have selected the right form for your city/region.
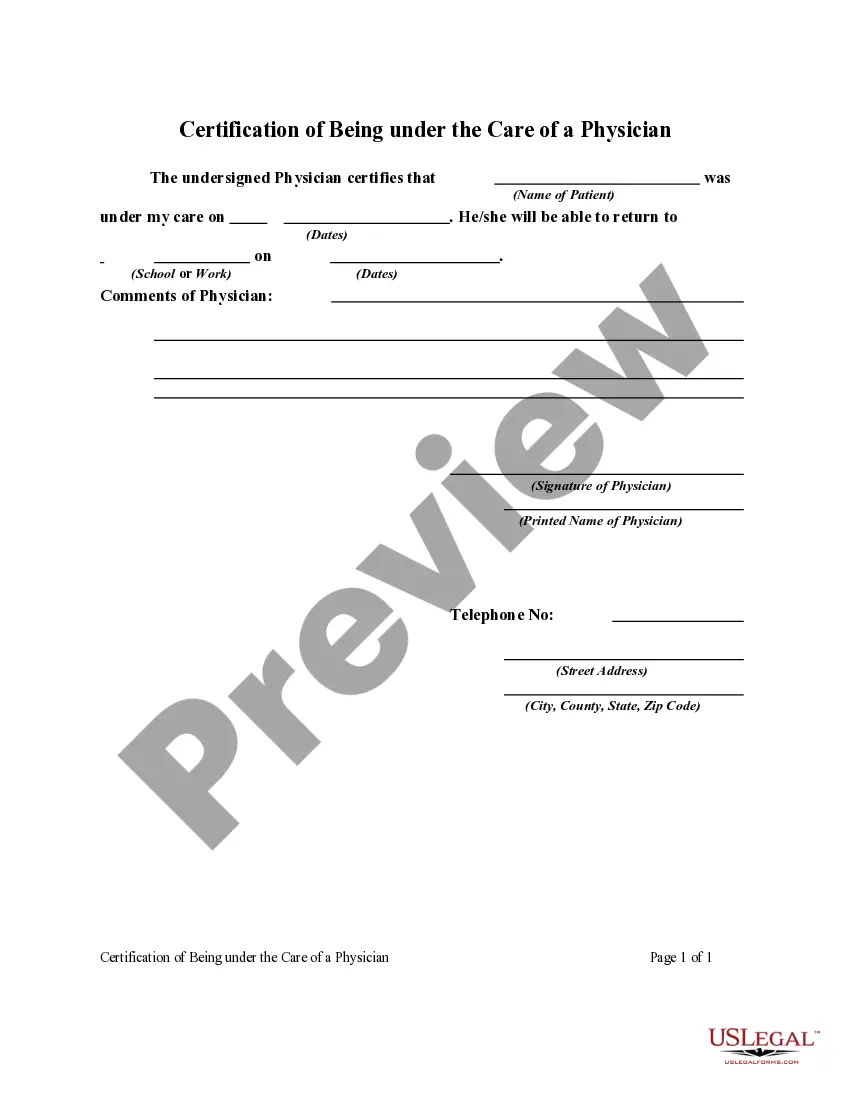
- Click on the Review button to check the content of the form.
- Read the form description to confirm that you have selected the correct one.
- If the form doesn't fit your needs, use the Search field at the top of the screen to find the one that does.
- Once you’re satisfied with the form, confirm your choice by clicking the Buy now button.
- Then choose the pricing plan you prefer and provide your details to register for an account.
Form popularity
FAQ
A dependent is a person who is eligible to be covered by you under these plans.
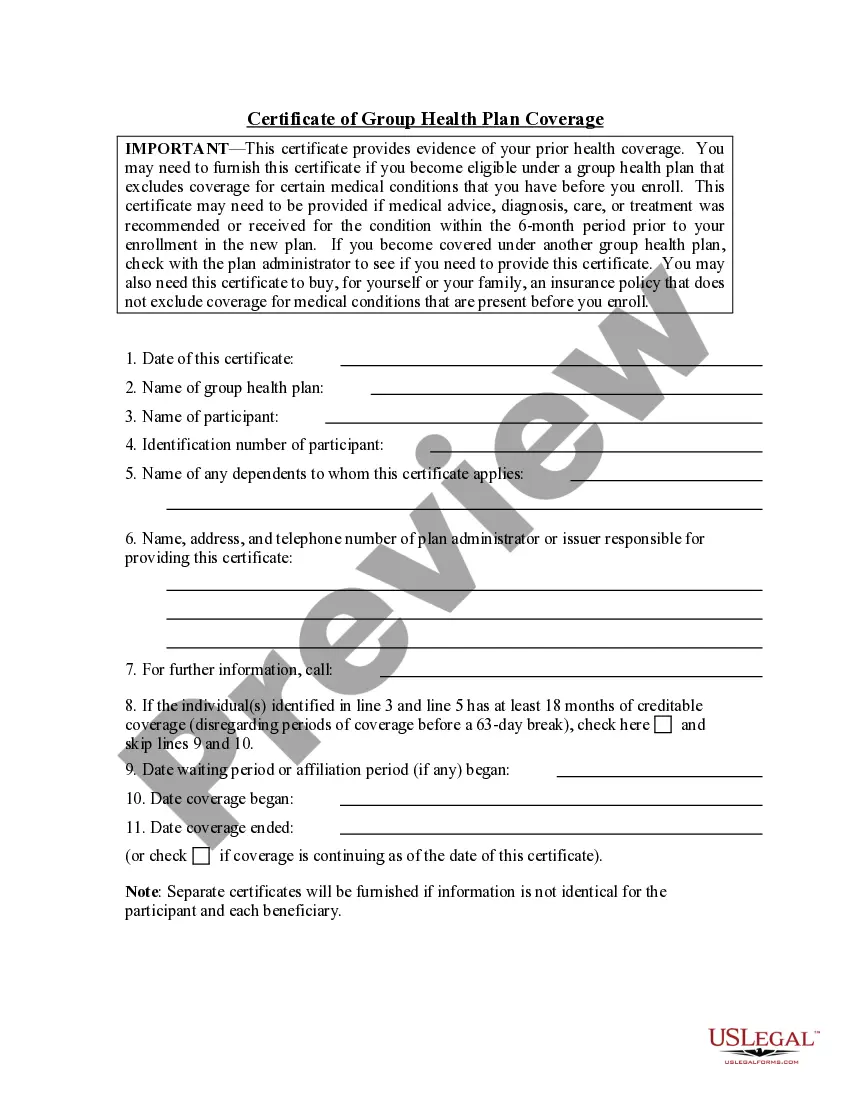
The primary purpose of the certificate is to show the amount of creditable coverage that you had under a group health plan or other health insurance coverage, because this can reduce or eliminate the length of time that any pre-existing condition clause in a new plan otherwise might apply to you.
A certificate of Creditable Coverage (COCC) is a document provided by your previous insurance carrier that proves that your insurance has ended. This includes the name of the member to whom it applies as well as the coverage effective date and cancelation date.
Noncontributory - Group life insurance plans are those in which the employer pays the entire premium and the employee supplies no portion of the premium costs. Employers have the option of contributing to the employees' premium payments in part or in full.
The term continuation coverage refers to the extended coverage provided under the group benefit plan in which an eligible employee or eligible dependent is currently enrolled.
If a Social Security agreement assigns coverage of the employee's work to the United States, the Social Security Administration issues a U.S. Certificate of Coverage. The certificate serves as proof that the employee and employer are exempt from the payment of Social Security taxes to the foreign country.
Continuation coverage allows someone who recently lost their employer-based health coverage to continue their current insurance policy as long as they pay the full monthly premiums.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
State continuation coverage refers to state laws that enable employees to extend their employer-sponsored group health insurance even if they are not eligible for an extension through COBRA. While COBRA law applies throughout the U.S., it is only applicable to employers with 20 or more employees.
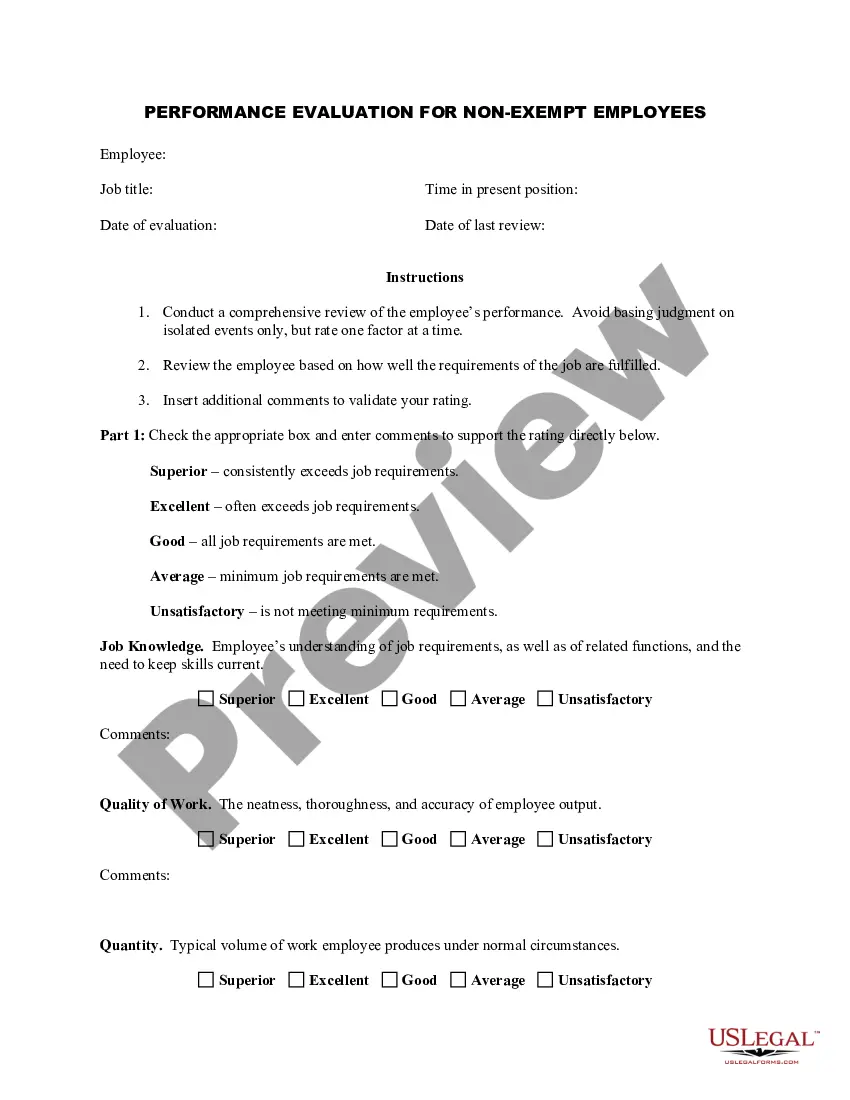
What Is Group Coverage? Group medical coverage refers to a single policy issued to a group (typically a business with employees, although there are other kinds of groups that can get coverage) that covers all eligible employees and sometimes their dependents.