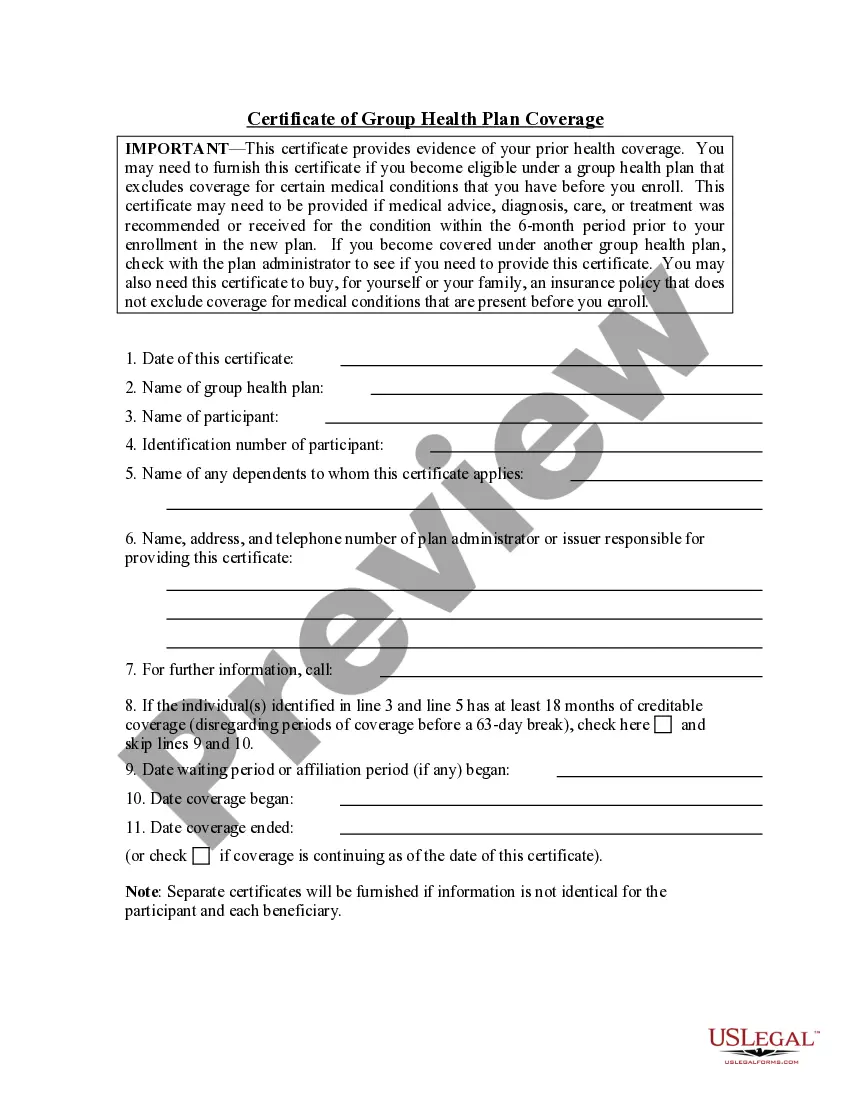
Kentucky Certificate of Group Health Plan Coverage with Statement of HIPAA Portability Rights
Description
How to fill out Certificate Of Group Health Plan Coverage With Statement Of HIPAA Portability Rights?
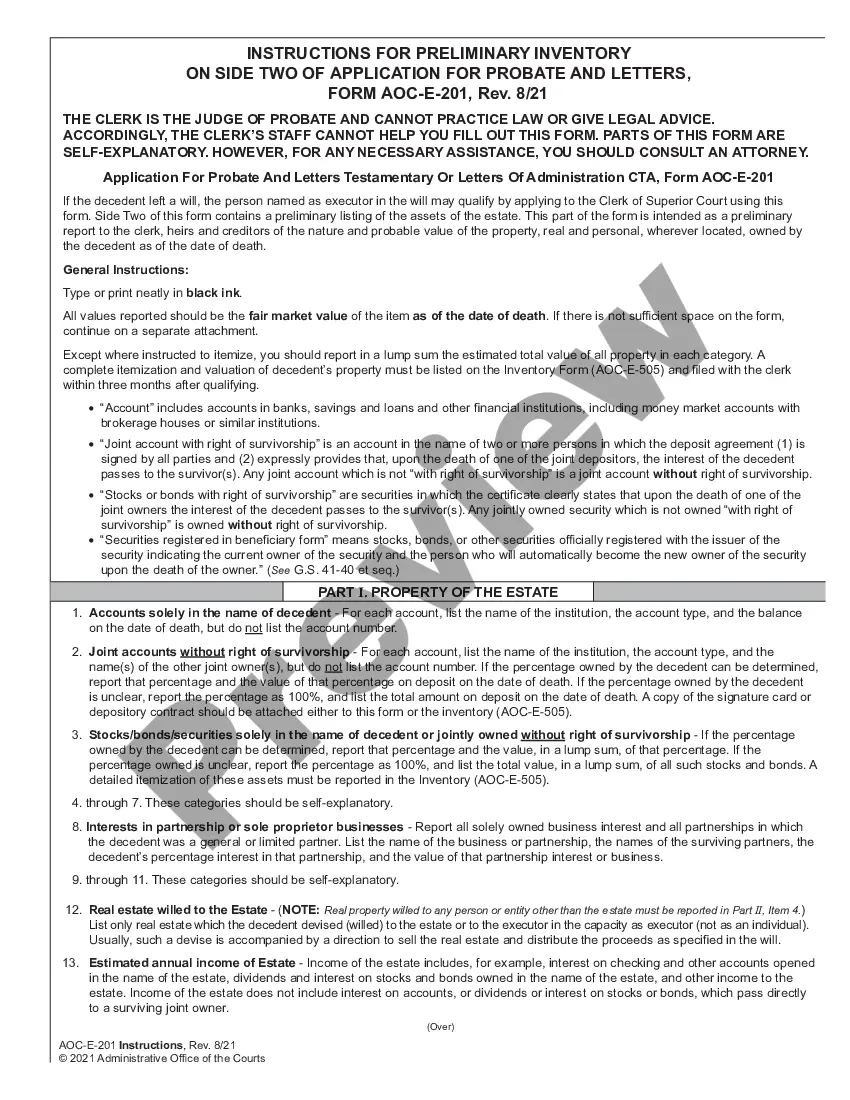
Are you in a place where you will need documents for possibly company or personal functions virtually every day? There are plenty of authorized record themes accessible on the Internet, but finding types you can rely isn`t straightforward. US Legal Forms offers a large number of kind themes, such as the Kentucky Certificate of Group Health Plan Coverage with Statement of HIPAA Portability Rights, which can be published to meet state and federal demands.
If you are already familiar with US Legal Forms web site and have an account, just log in. Afterward, you are able to acquire the Kentucky Certificate of Group Health Plan Coverage with Statement of HIPAA Portability Rights design.
Unless you have an account and need to start using US Legal Forms, adopt these measures:
- Find the kind you need and make sure it is to the appropriate city/state.
- Use the Preview switch to check the form.
- Browse the information to ensure that you have selected the right kind.
- In case the kind isn`t what you are searching for, use the Research field to discover the kind that suits you and demands.
- Whenever you obtain the appropriate kind, simply click Buy now.
- Opt for the prices plan you would like, submit the desired details to produce your money, and buy the transaction with your PayPal or Visa or Mastercard.
- Pick a convenient paper structure and acquire your version.
Locate each of the record themes you may have purchased in the My Forms food selection. You can aquire a additional version of Kentucky Certificate of Group Health Plan Coverage with Statement of HIPAA Portability Rights at any time, if possible. Just select the essential kind to acquire or printing the record design.
Use US Legal Forms, one of the most substantial selection of authorized forms, to save lots of efforts and steer clear of mistakes. The assistance offers appropriately manufactured authorized record themes that can be used for a selection of functions. Create an account on US Legal Forms and initiate making your life a little easier.
Form popularity
FAQ
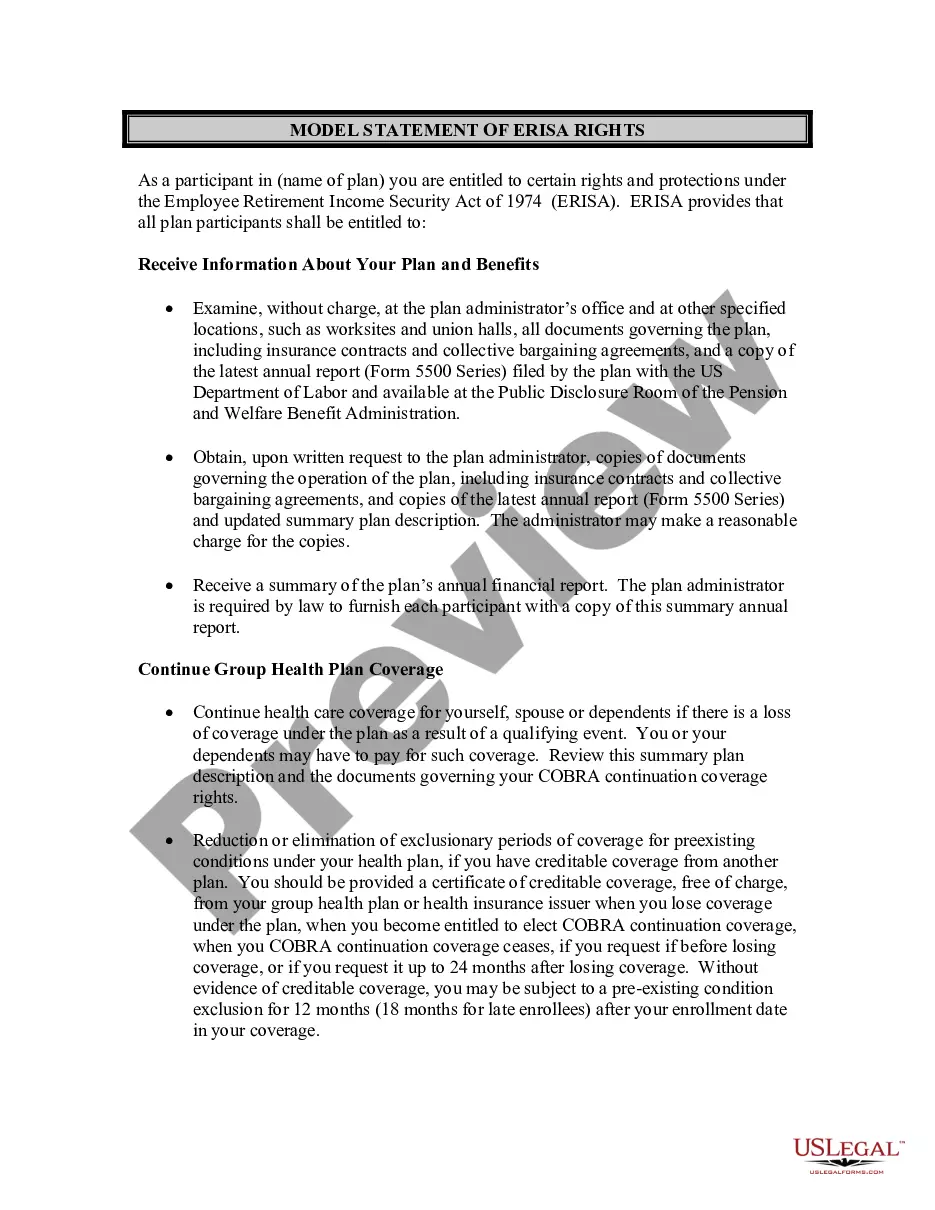
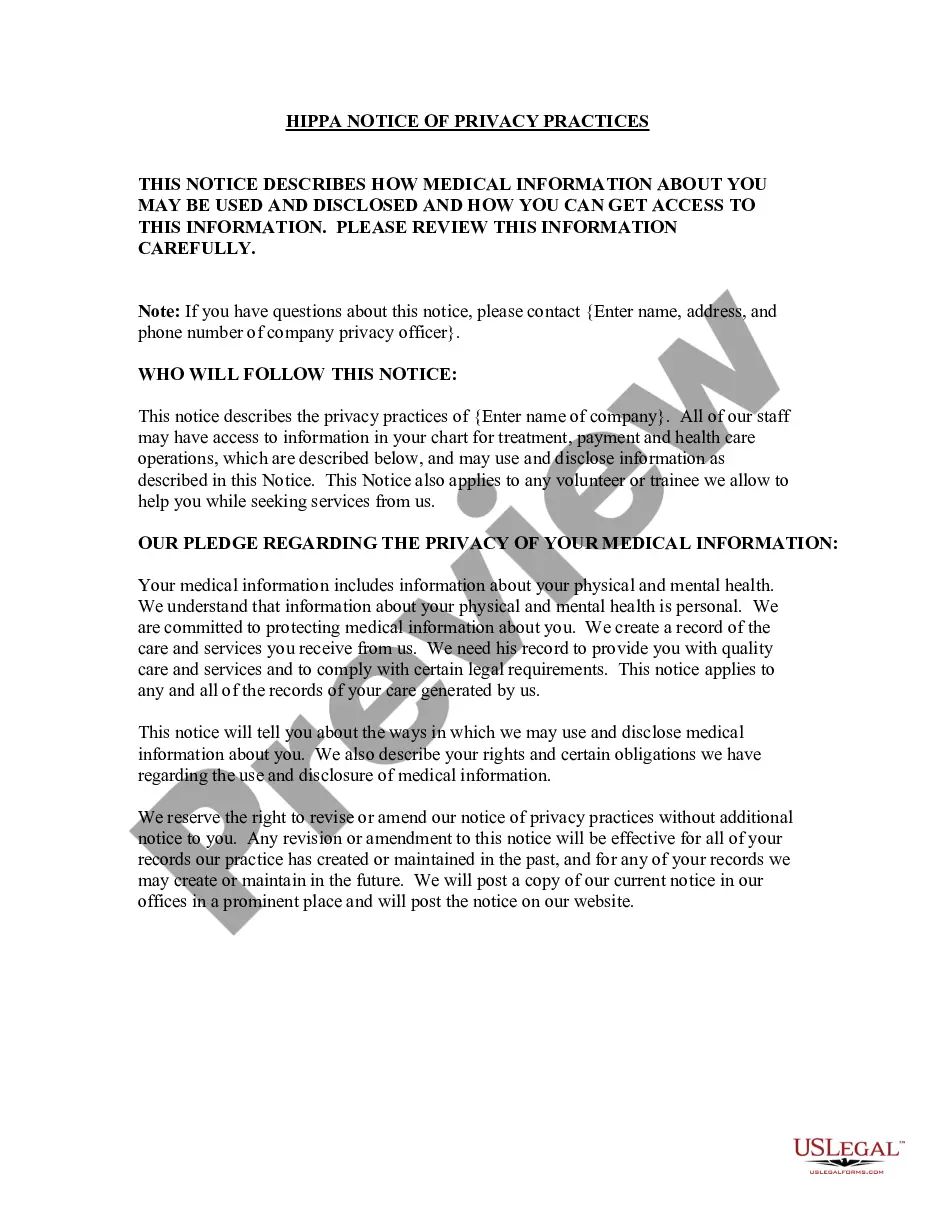
As a recap, all plans that self-insure, have fewer than 50 participants and are internally administered, are exempt from the privacy rule.
The definition of ?group health plan? is adopted from the statutory definition at section 1171(5)(A), and excludes from the rule as ?health plans? only the few insured or self-insured ERISA plans that have less than 50 participants and are self administered.
ANSWER: A health plan with fewer than 50 participants that is administered by the sponsoring employer is excluded from the definition of a ?group health plan? under HIPAA's administrative simplification provisions, which include the privacy and security requirements.
What is one way that the Health Insurance Portability and Accountability Act (HIPAA) limits exclusions to the rules for preexisting conditions? a) It allows employer-provided health plans to look back only 6 months for preexisting conditions.
Exceptions to the HIPAA Privacy Rule Limitations apply to uses and disclosures for the purpose of facilitating another party's activities. Exceptions are allowed for a covered entity to disclose PHI to: Any other provider (even a non-covered entity) to facilitate that provider's treatment activities.
What is a Non-Covered Entity Under HIPAA? As mentioned above, a non-covered entity is an entity that is not subject to the requirements of the HIPAA Privacy Rule. There are two types of non-covered entities under HIPAA: business associates and hybrid entities.
The CoC details the health benefits the beneficiary and their dependents have under their plan. Details include exclusions and conditions. Exclusions are uncovered services, and conditions are actions needed to receive benefits.
HIPAA, also known as Public Law 104-191, has two main purposes: to provide continuous health insurance coverage for workers who lose or change their job and to ultimately reduce the cost of healthcare by standardizing the electronic transmission of administrative and financial transactions.