Indiana Affidavit of No Coverage by Another Group Health Plan
Description
How to fill out Affidavit Of No Coverage By Another Group Health Plan?
Selecting the top approved document template can be a challenge.
Clearly, there are numerous designs available online, but how do you find the legal form you require.
Utilize the US Legal Forms website.
If you are a new user of US Legal Forms, here are simple instructions to follow: First, make sure you have selected the correct form for your jurisdiction. You can review the form using the Preview button and read the form description to ensure it is the right fit for you. If the form does not meet your requirements, use the Search field to find the appropriate form. Once you are confident that the form is suitable, click the Get Now button to obtain the form. Choose your desired pricing plan and enter the required information. Create your account and pay for your order using your PayPal account or credit card. Choose the file format and download the legal document template to your device. Complete, modify, print, and sign the obtained Indiana Affidavit of No Coverage by Another Group Health Plan. US Legal Forms is the largest collection of legal forms where you can access numerous document templates. Utilize the service to obtain professionally crafted documents that adhere to state requirements.
- The platform provides thousands of templates, including the Indiana Affidavit of No Coverage by Another Group Health Plan, suitable for both business and personal purposes.
- All forms are verified by professionals and comply with state and federal regulations.
- If you are already registered, Log In to your account and click the Download button to obtain the Indiana Affidavit of No Coverage by Another Group Health Plan.
- Use your account to search through the legal forms you may have previously purchased.
- Navigate to the My documents tab in your account to secure another copy of the document you need.
Form popularity
FAQ
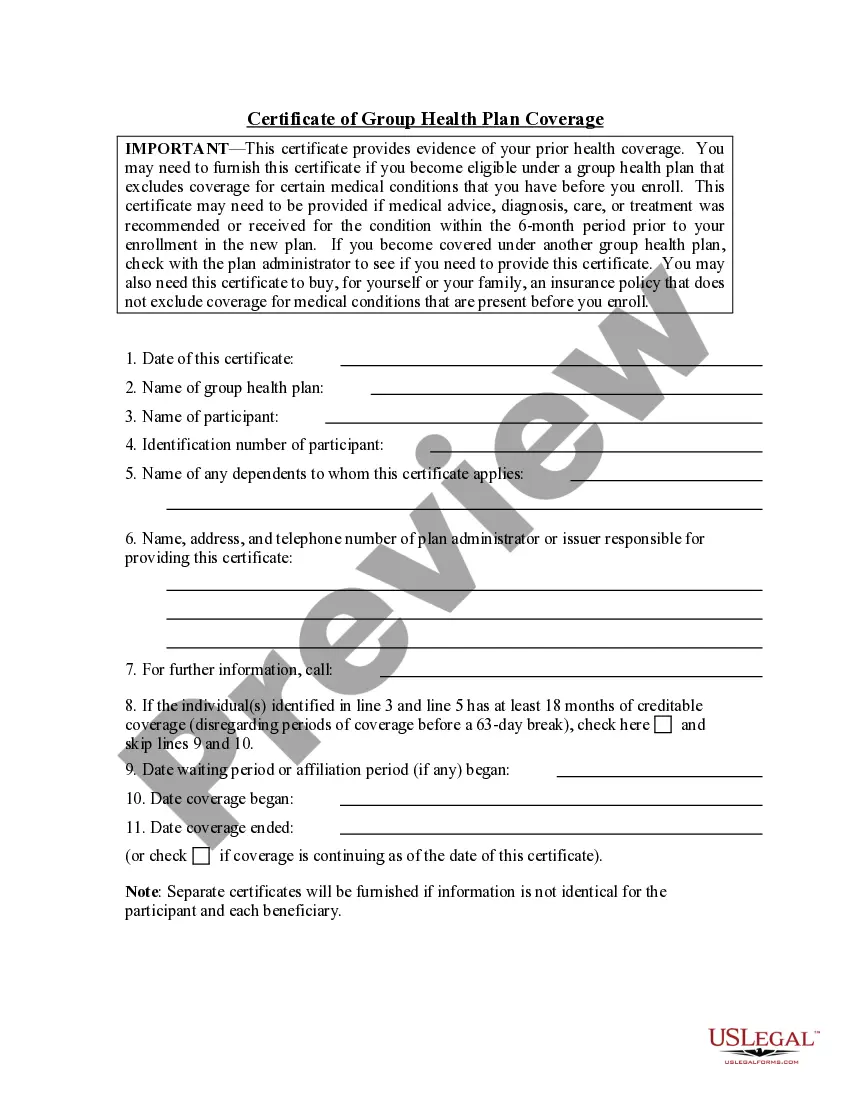
If you're losing health coverage. You must send documents showing the lost coverage and the date it ends. Acceptable documents include notices from your previous insurance company or your employer.
When a group life insurance claim is denied, the beneficiary may find himself struggling with paying funeral expenses and other financial obligations associated with the death of a loved one. A family who loses the only breadwinner and receives a denial letter from the life insurance company may feel despair.
Types of exclusions in health insurancePre-existing illnesses. War/radiation-induced illnesses/injuries. Voluntary medical procedures/tests. External durable items.
A coverage position letter is a letter communicating a coverage position to the insured. There are three basic types: Those letters that inform the insured there is a question of coverage. Those letters that inform the insured there is no coverage. Those letters that inform the insured there is no question of coverage.
When is Evidence of Insurability required? EOI is generally required for coverage in excess of any applicable guarantee-issue amount, late entrants, reinstatements if required, members and dependents eligible but not insured under the prior plan, and re- applications for previously-declined coverage.
A. The Evidence of Coverage (EOC) is a document that describes in detail the health care benefits covered by the health plan. It provides documentation of what that plan covers and how it works, including how much you pay.
Loss of Coverage means a complete loss of coverage under, or elimination of, a Component Plan or a Medical or Dental Plan, including the elimination of a Component Plan.
Loss of Coverage Letter Letter from your previous health carrier indicating an involuntary loss of coverage. The supporting document must indicate your name, the names of any dependents that were covered under the prior plan and the date the previous health coverage ended.
A letter from an employer, on official letterhead or stationery, that confirms one of these about you or your spouse or dependent family member:That your employer dropped or will drop your coverage or benefits. That your employer stopped or will stop contributing to your cost of coverage.
Without evidence of insurability means an insurance provider underwrote a policy, such as for life or health insurance, without verifying that the policyholder was eligible for that coverage. Some group plans may not require proof of insurability if the applicant applies during the open enrollment period.