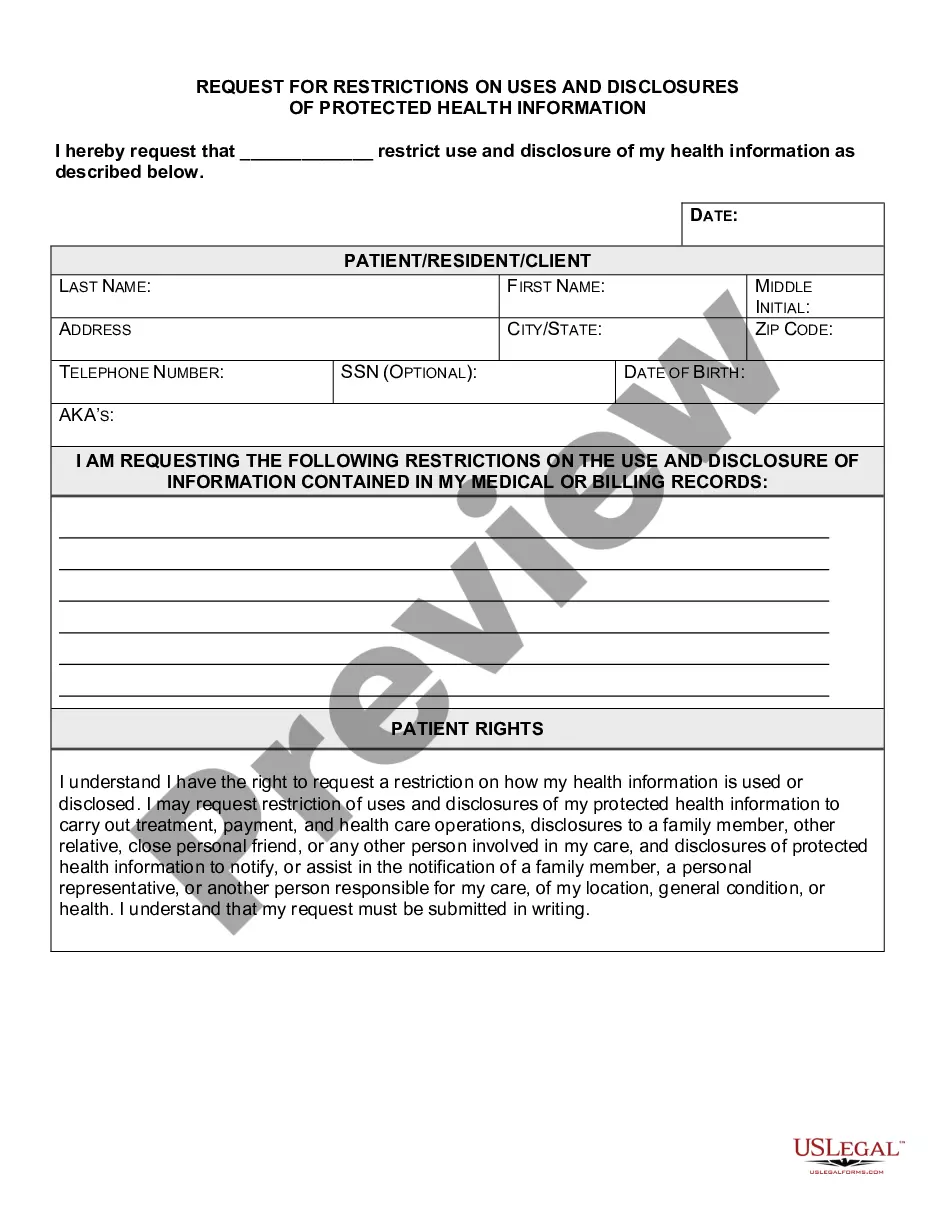
Illinois Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
Locating the appropriate legal document template can be a challenge.
Naturally, there is a wide range of formats accessible online, but how will you discover the legal document you seek.
Utilize the US Legal Forms platform.
First, ensure you have selected the correct form for your area/region. You can preview the form using the Review button and examine the form description to confirm it is suitable for your needs.
- This service offers a multitude of templates, including the Illinois Request for Limitations on Uses and Disclosures of Protected Health Information, suitable for business and personal needs.
- All forms are reviewed by professionals and meet federal and state regulations.
- If you're already registered, Log In to your account and click the Download button to obtain the Illinois Request for Limitations on Uses and Disclosures of Protected Health Information.
- Use your account to browse through the legal forms you have acquired previously.
- Navigate to the My documents section of your account to download another copy of the document you need.
- If you are a new user of US Legal Forms, here are simple instructions for you to follow.
Form popularity
FAQ
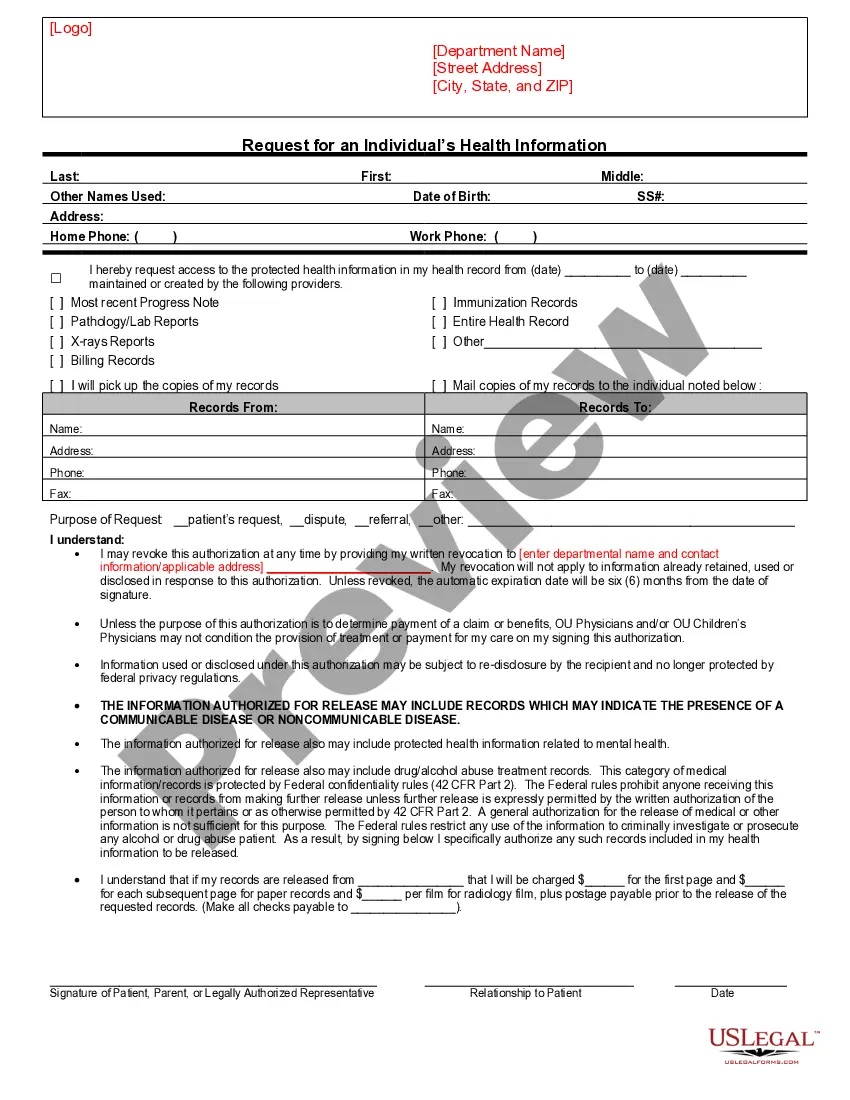
What is a patient required to do in order for a request to restrict the use or disclosure of their PHI to their health plan to be granted? The Privacy Rule allows for a patient to request that no information be shared with others even to the point of not acknowledging the patient's presence in the covered entity.
4 ways of protecting patient privacyBuild a security culture in your organization.Perform a security risk assessment.Create a PHI security improvement plan.Encrypt all patient data.
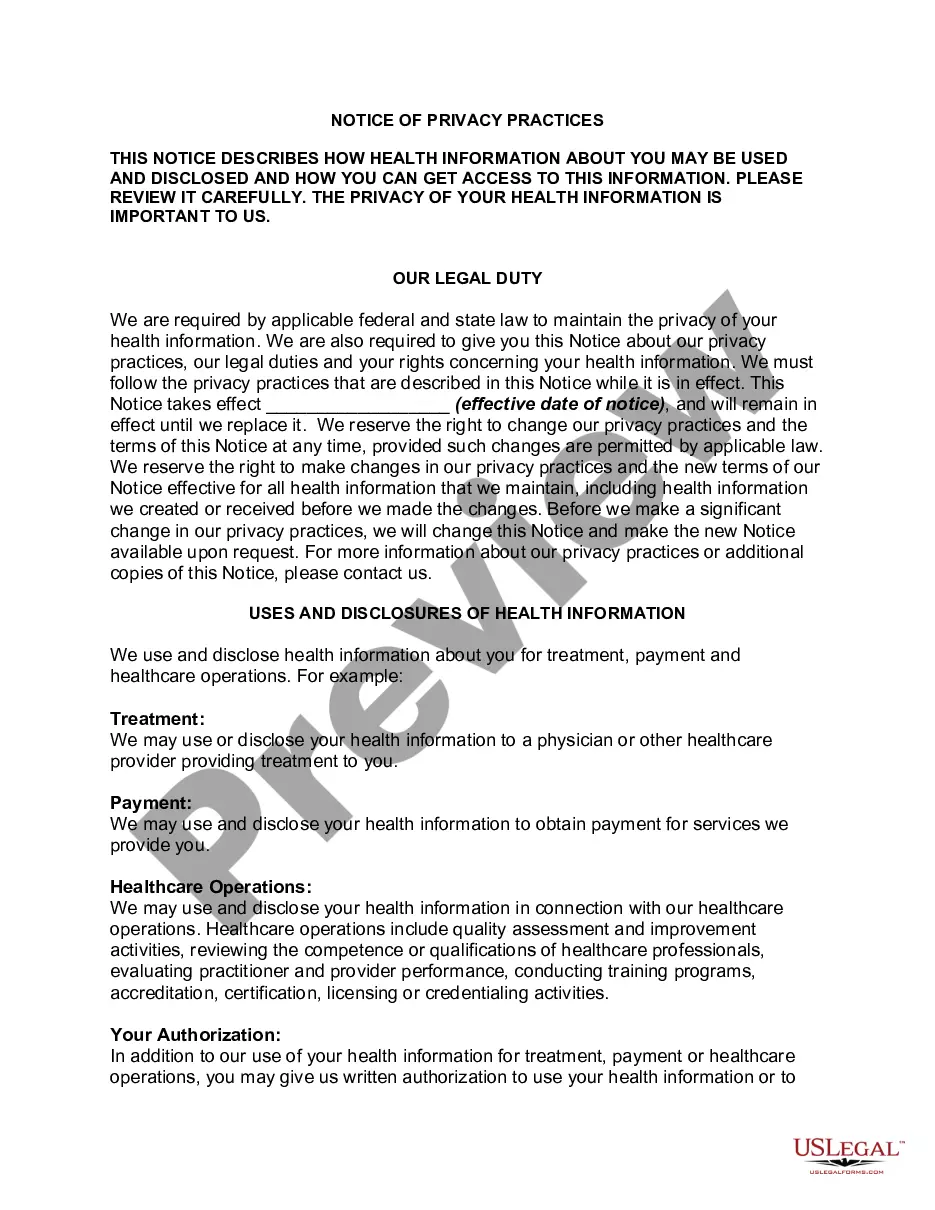
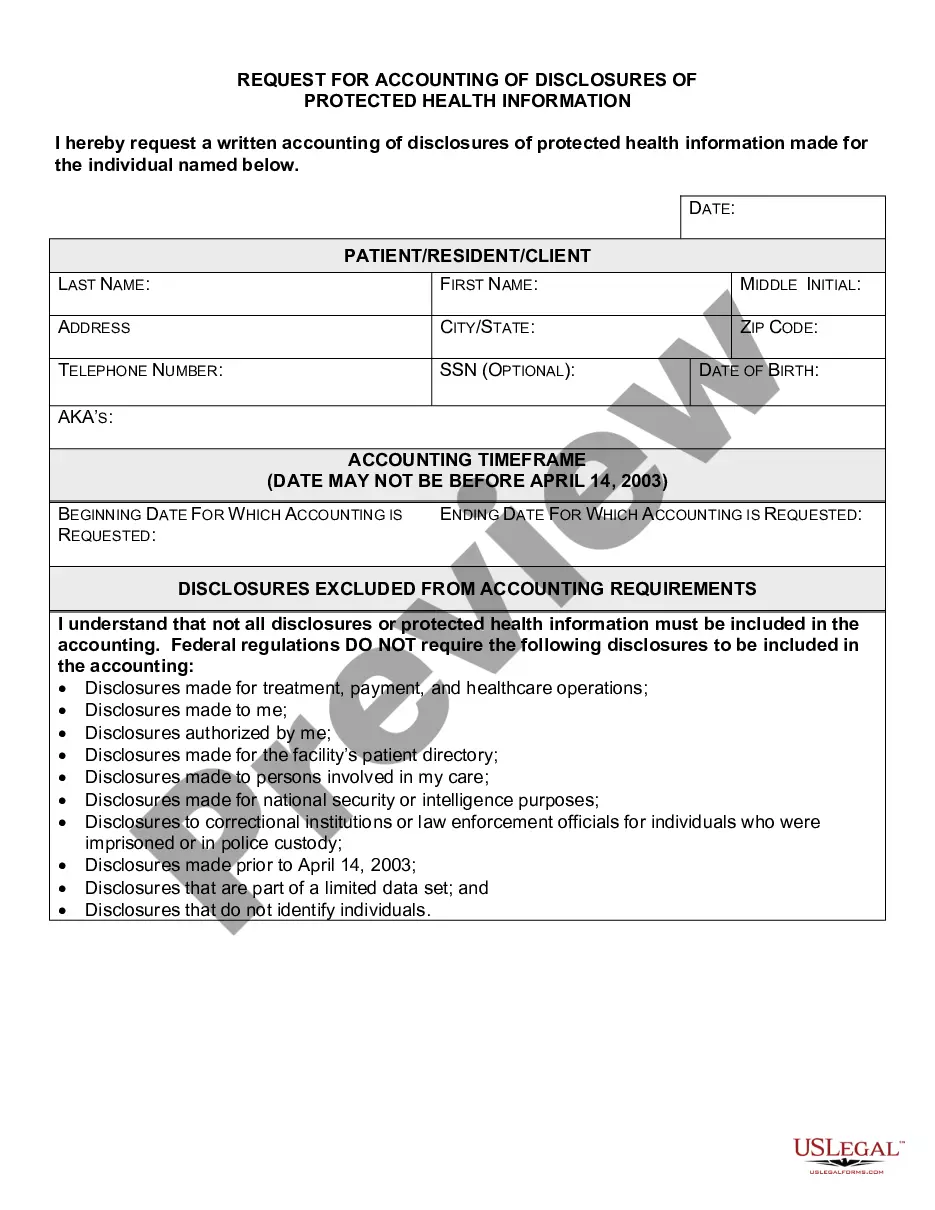
"Minimum Necessary" means, when protected health information is used, disclosed, or requested, reasonable efforts must be taken to determine how much information will be sufficient to serve the intended purpose.
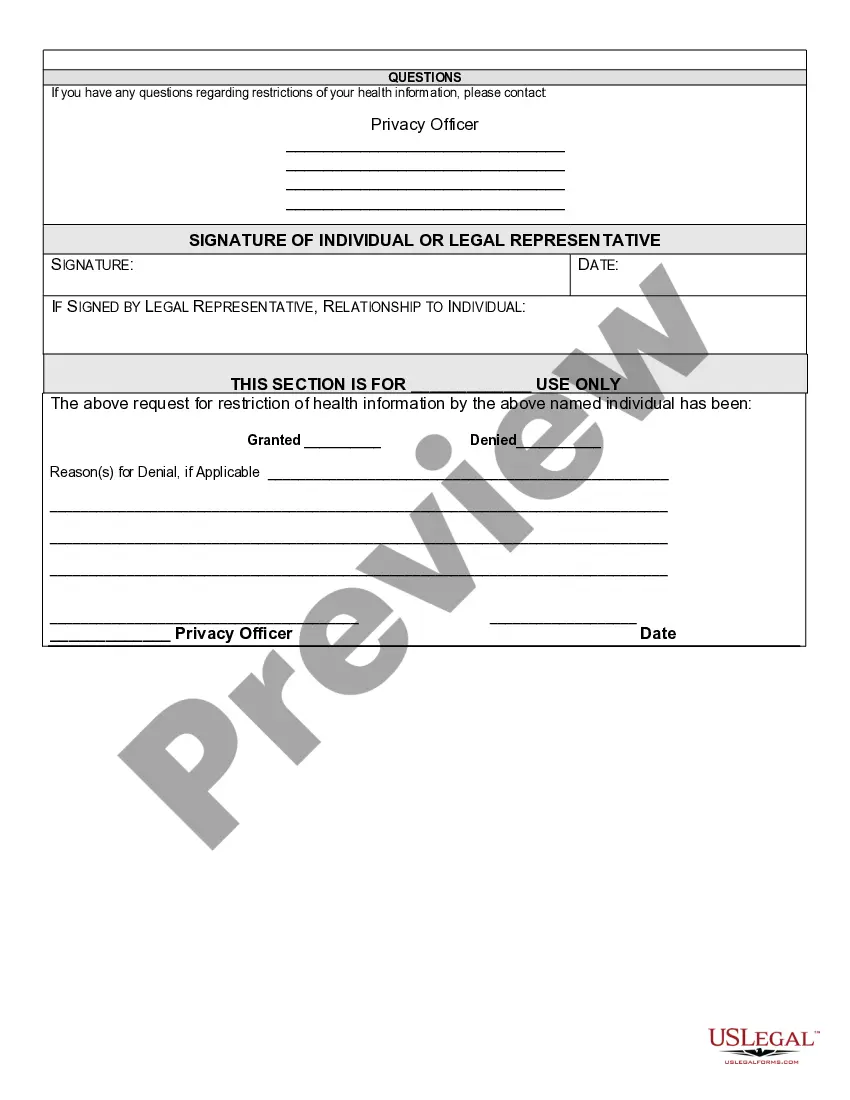
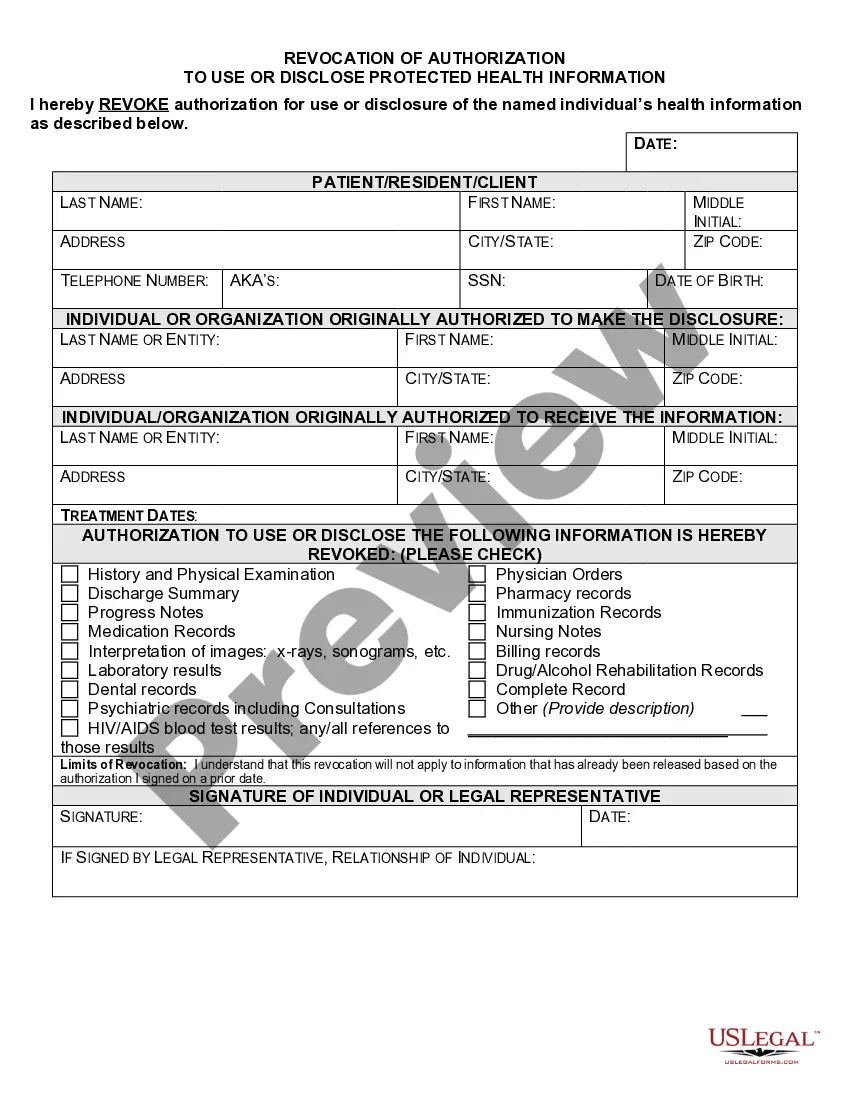
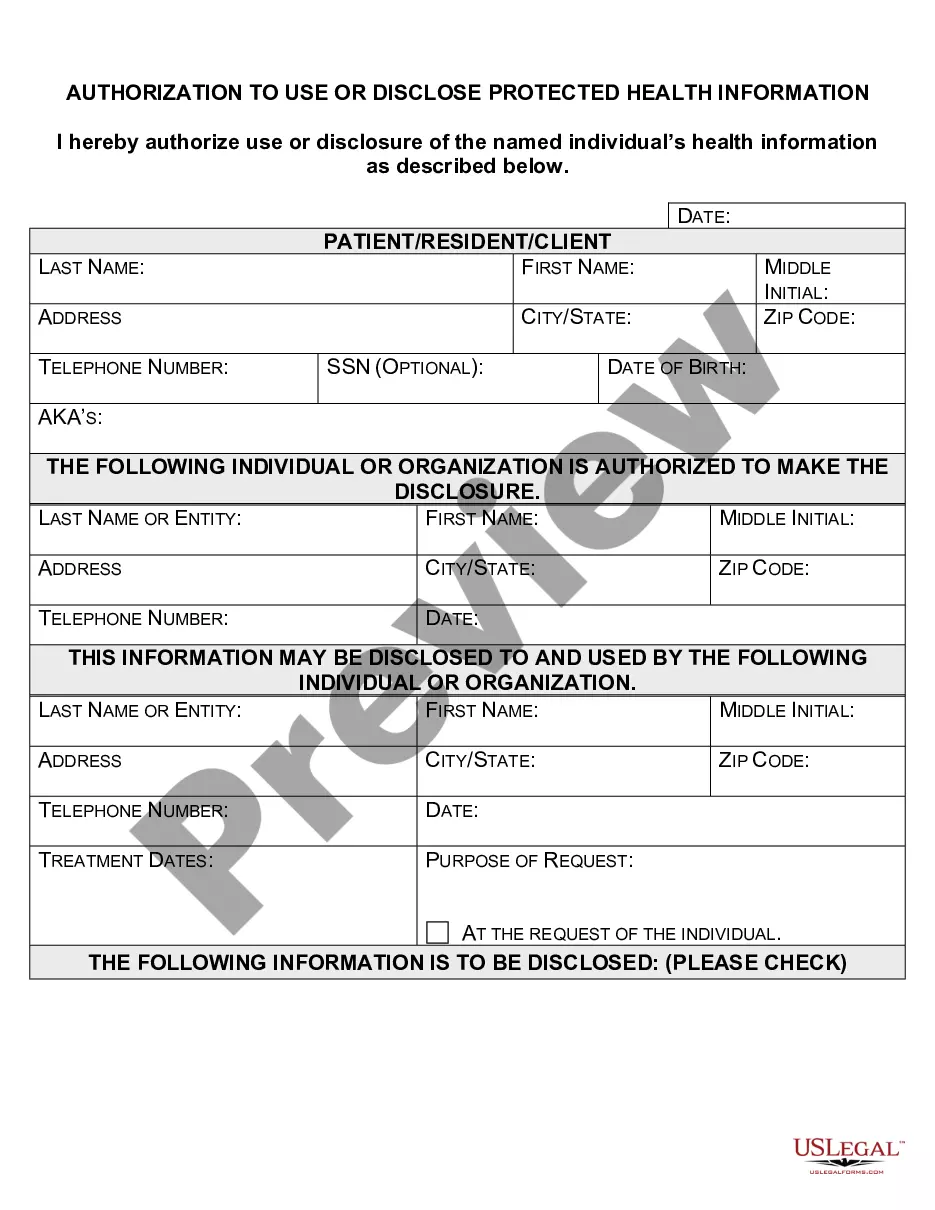
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the
General Right. The Privacy Rule generally requires HIPAA covered entities (health plans and most health care providers) to provide individuals, upon request, with access to the protected health information (PHI) about them in one or more designated record sets maintained by or for the covered entity.
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item
Under the new rule, individuals now have a right to obtain restrictions on the disclosure of health information (protected health information or PHI) in electronic or any other form to a health plan for payment or healthcare operations with respect to specific items and services for which the individual has paid the
When a patient requests that information not be disclosed to a specified individual or entity, the Request Restrictions on Use and Disclosure of PHI form must be completed and signed. An authorized healthcare professional will review the request and determine if it can be accommodated.
Illinois law works in tandem with federal regulations regarding medical records, under the federal law known as the Health Insurance Portability and Accountability Act (HIPAA). HIPAA requires doctors and their staff to keep your medical records strictly confidential.
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item