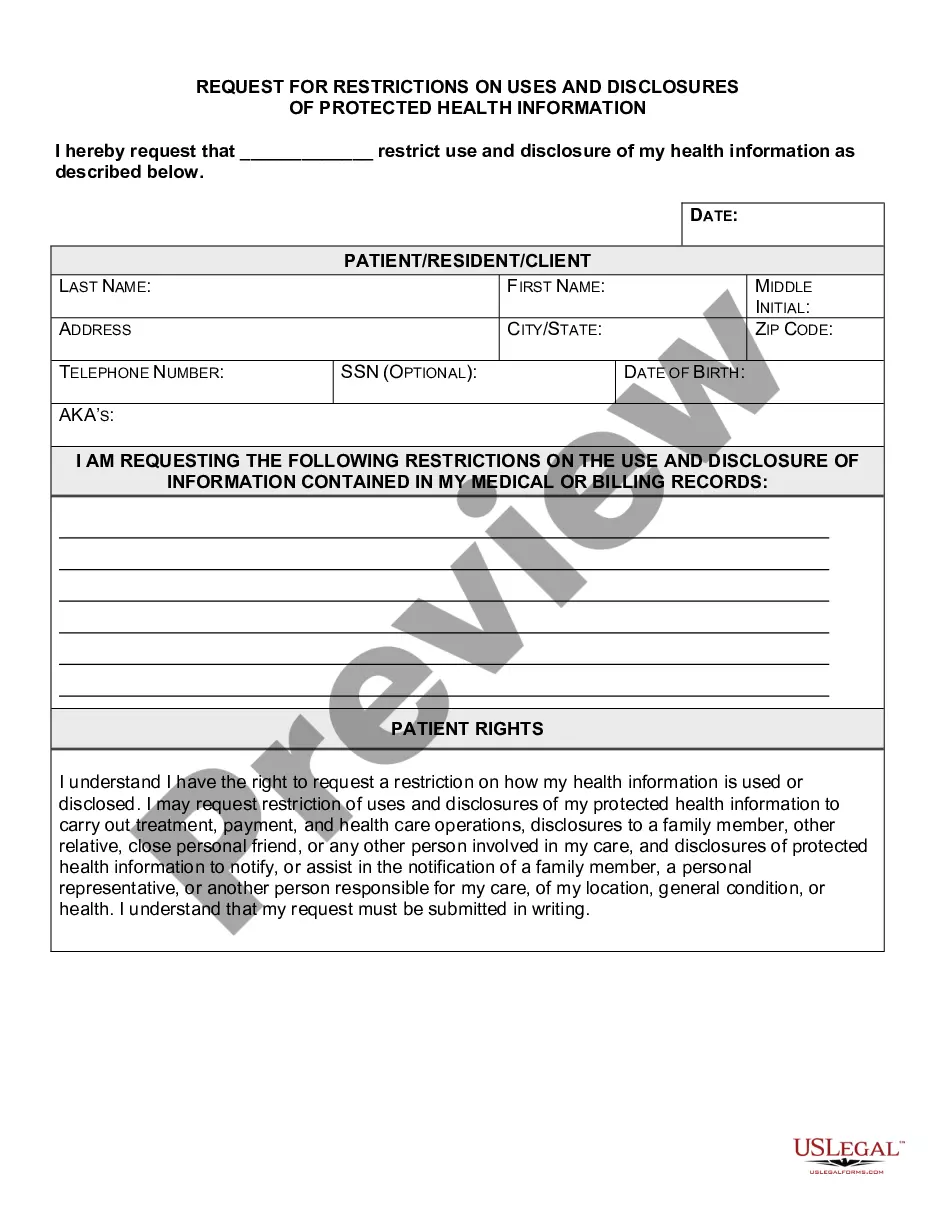
Delaware Request for Restrictions on Uses and Disclosures of Protected Health Information
Description
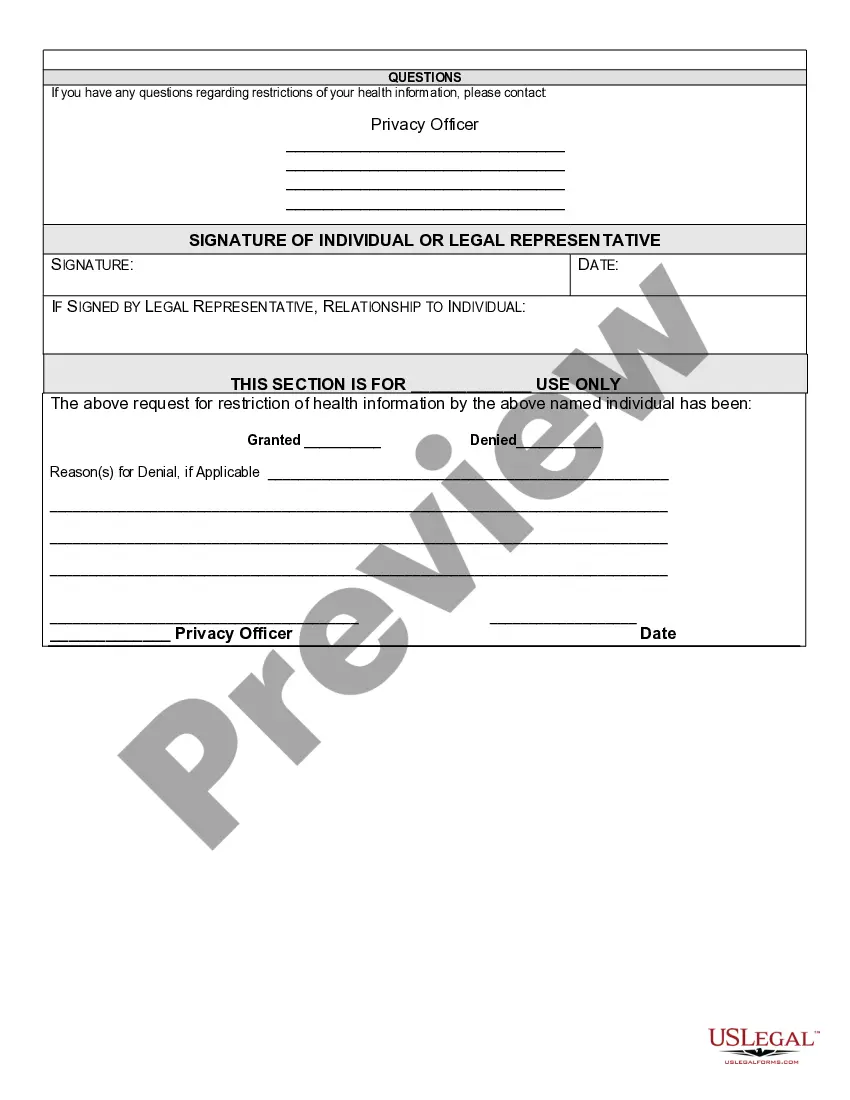
How to fill out Request For Restrictions On Uses And Disclosures Of Protected Health Information?
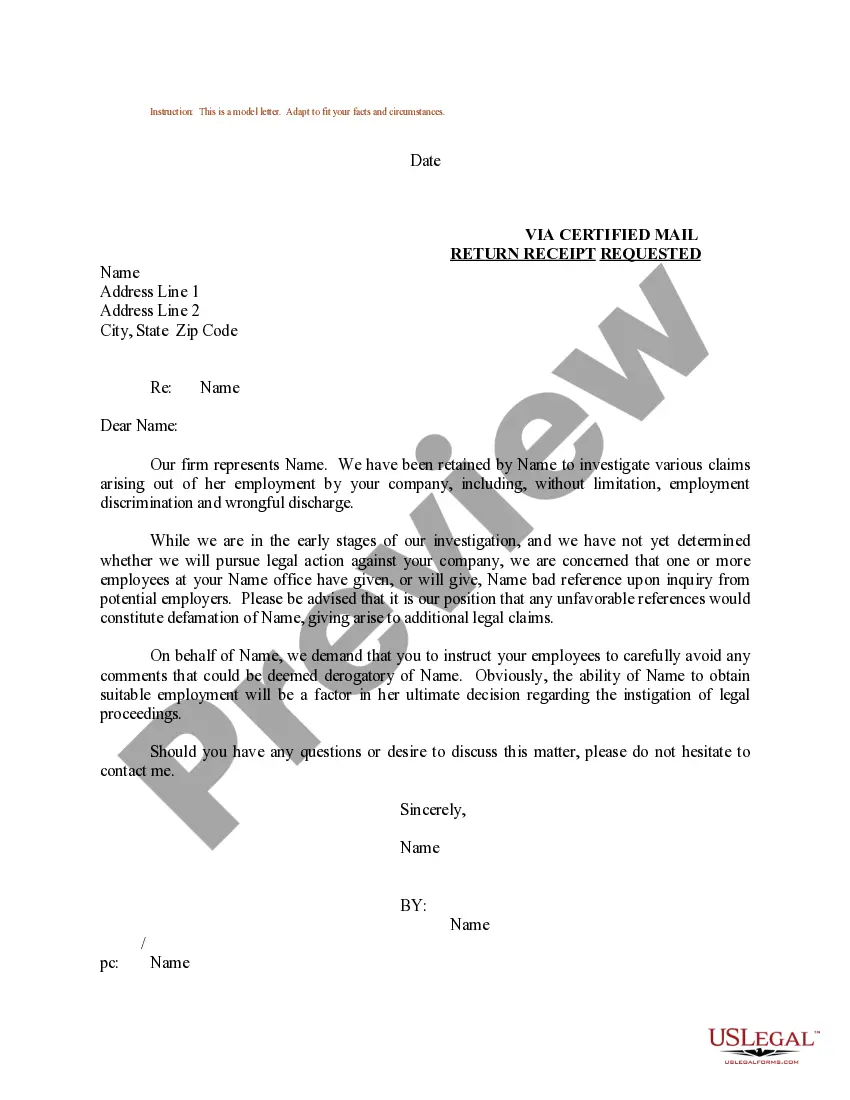
You can spend several hours online searching for the appropriate legal document template that meets the requirements of both federal and state regulations you require.
US Legal Forms offers a vast array of legal forms that are vetted by experts.
You can easily download or print the Delaware Request for Restrictions on Uses and Disclosures of Protected Health Information from their service.
If available, use the Preview feature to examine the document template as well.
- If you possess a US Legal Forms account, you can sign in and select the Download option.
- Then, you can complete, modify, print, or sign the Delaware Request for Restrictions on Uses and Disclosures of Protected Health Information.
- Every legal document template you purchase is yours for an extended period.
- To obtain another copy of any acquired form, visit the My documents tab and click the appropriate link.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure you have selected the correct document template for your chosen state or city.
- Review the form description to confirm you have selected the correct form.
Form popularity
FAQ
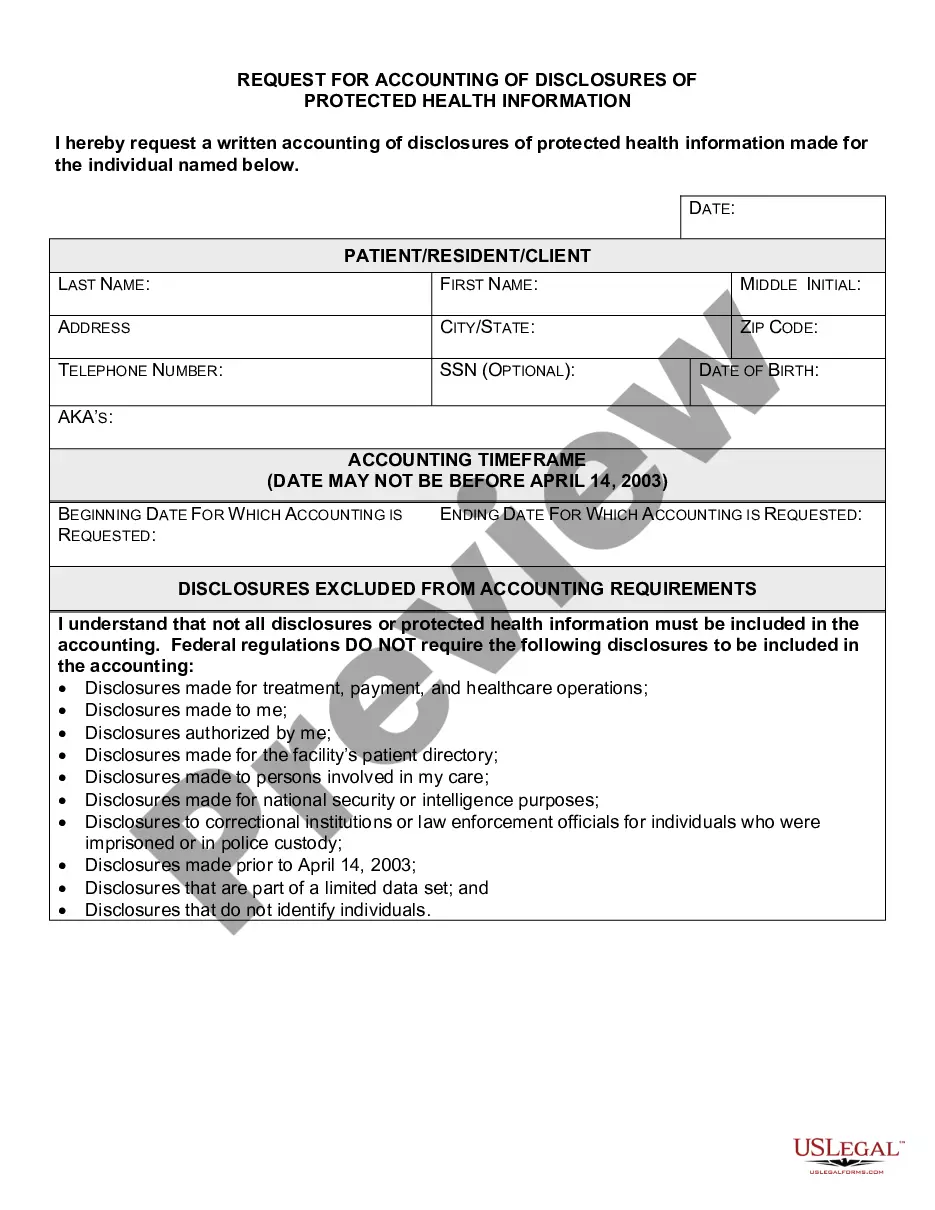
Generally, there are no restrictions on the use or disclosure of de-identified health information. This means that if health information does not include identifying details, it can be shared freely. However, when dealing with protected health information, it’s important to understand your rights. A Delaware Request for Restrictions on Uses and Disclosures of Protected Health Information can help you specify how your identifiable data should be handled.
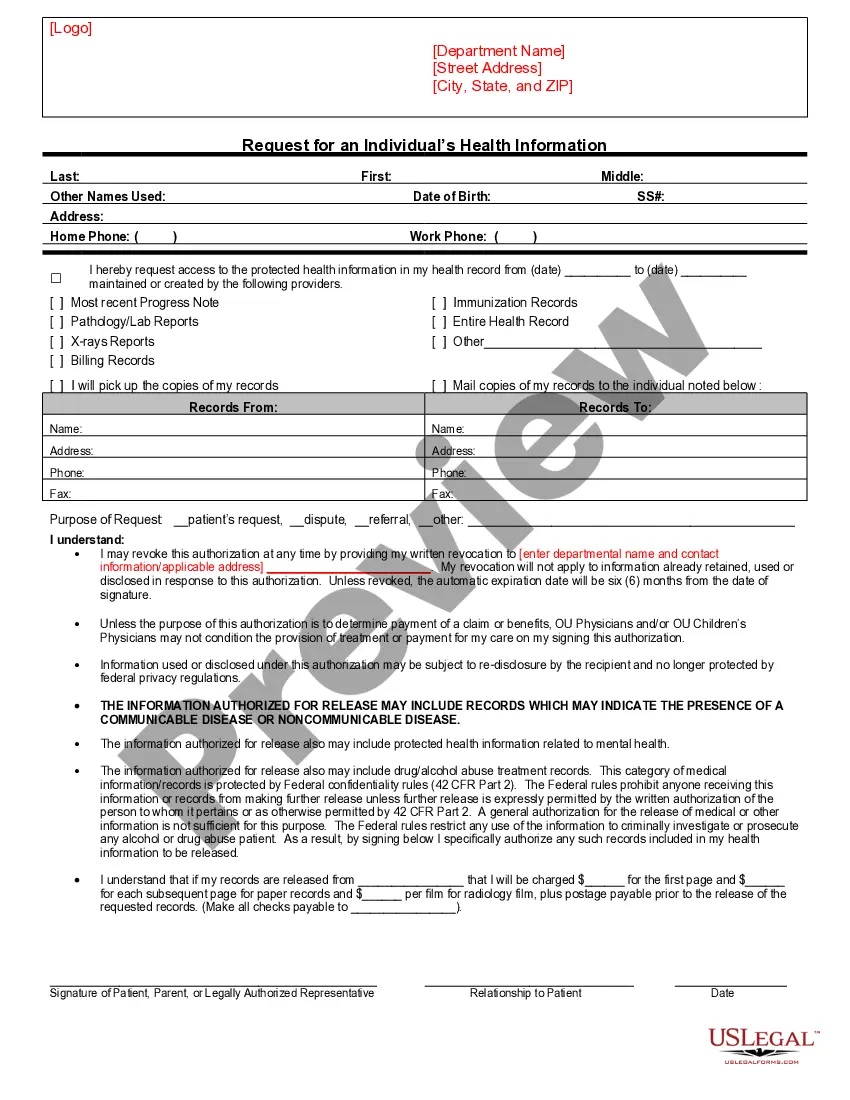
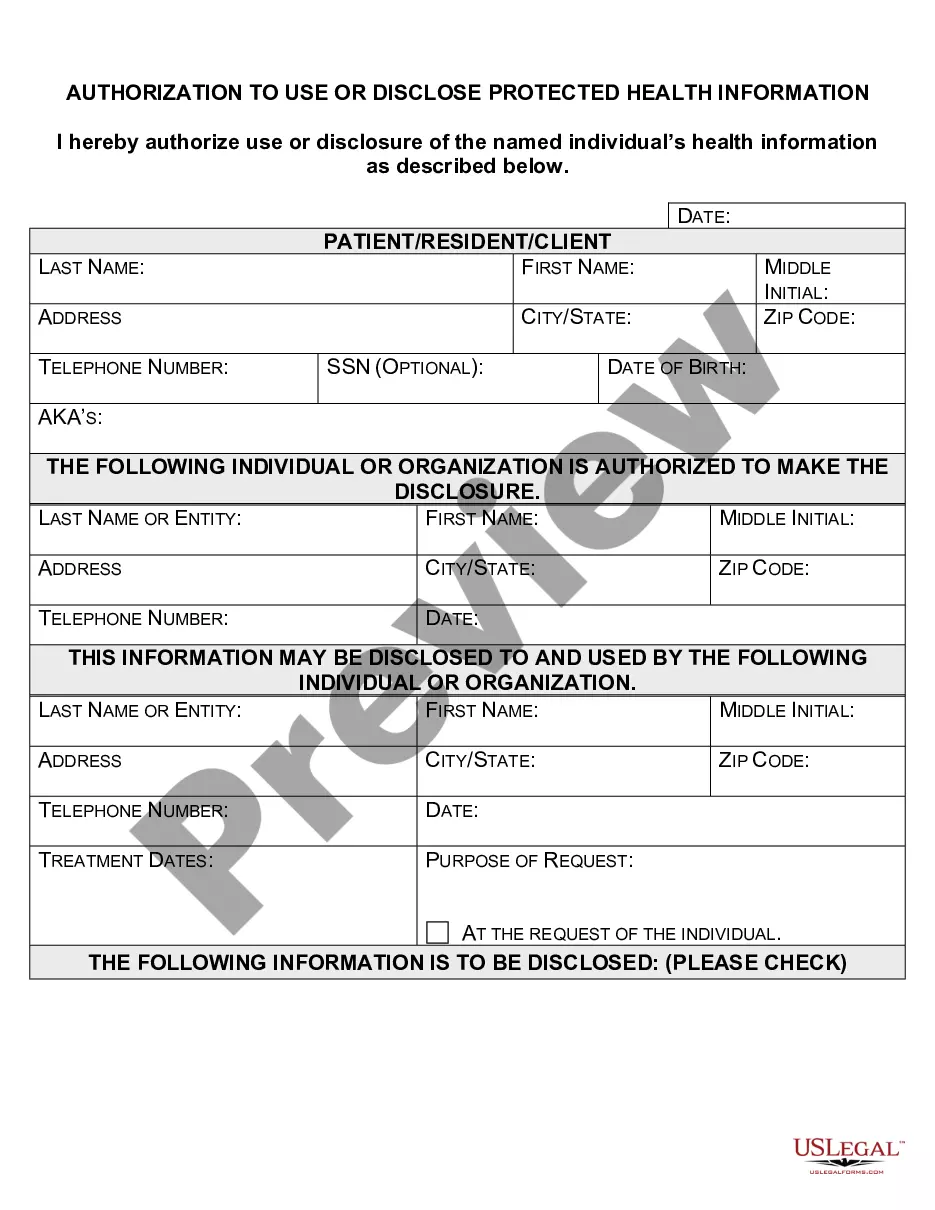
Under the new rule, individuals now have a right to obtain restrictions on the disclosure of health information (protected health information or PHI) in electronic or any other form to a health plan for payment or healthcare operations with respect to specific items and services for which the individual has paid the
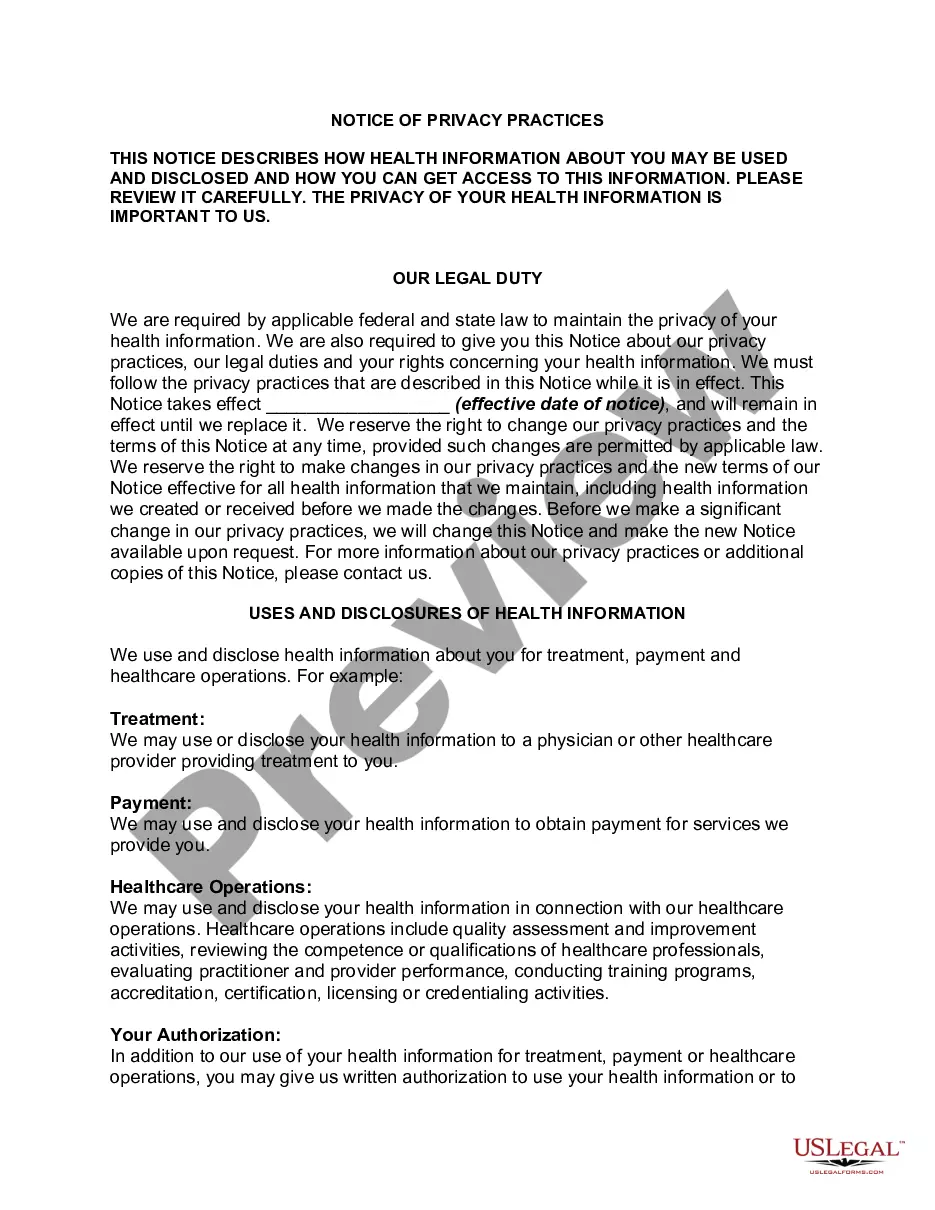
Use or disclose protected health information for its own treatment, payment, and health care operations activities. For example: A hospital may use protected health information about an individual to provide health care to the individual and may consult with other health care providers about the individual's treatment.
Covered entities may disclose protected health information that they believe is necessary to prevent or lessen a serious and imminent threat to a person or the public, when such disclosure is made to someone they believe can prevent or lessen the threat (including the target of the threat).
A covered entity may disclose protected health information to the individual who is the subject of the information. (2) Treatment, Payment, Health Care Operations. A covered entity may use and disclose protected health information for its own treatment, payment, and health care operations activities.
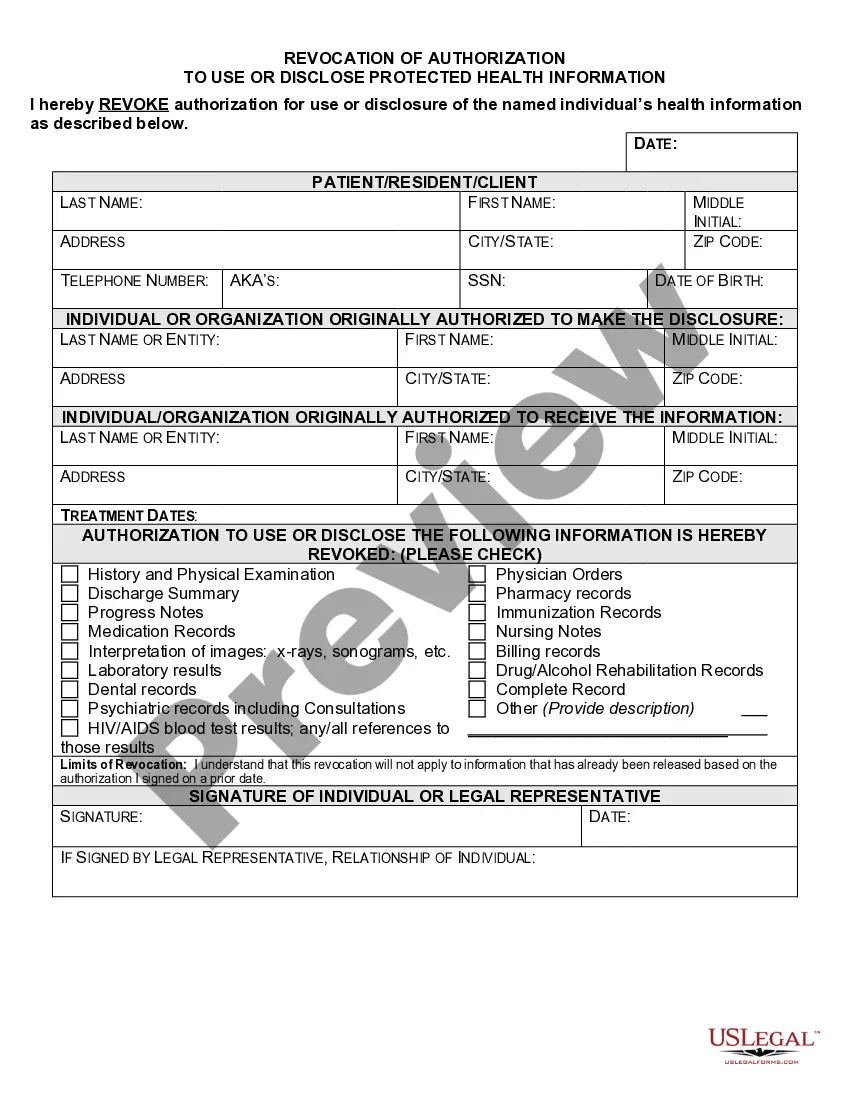
An authorization must specify a number of elements, including a description of the protected health information to be used and disclosed, the person authorized to make the use or disclosure, the person to whom the covered entity may make the disclosure, an expiration date, and, in some cases, the purpose for which the
Covered entities may disclose protected health information to: Public health authorities authorized by law to collect or receive such information for preventing or controlling disease, injury, or disability. Public health or other government authorities authorized to receive reports of child abuse and neglect.
Which of the following is an example of a permissible disclosure of protected health information (PHI) for payment purposes? Submitting a claim to the patient's insurance company with health information that is required to get the claim paid.
A covered entity is required to agree to an individual's request to restrict the disclosure of their PHI to a health plan when both of the following conditions are met: (1) the disclosure is for payment or health care operations and is not otherwise required by law; and (2) the PHI pertains solely to a health care item
Since its initial adoption, the Health Insurance Portability and Accountability Act of 1996 (HIPAA) Privacy Rule has granted individuals the right to request restrictions regarding the use and disclosure of their protected health information (PHI) for treatment, payment, and healthcare operations (TPO).