District of Columbia General Notice of Preexisting Condition Exclusion
Description
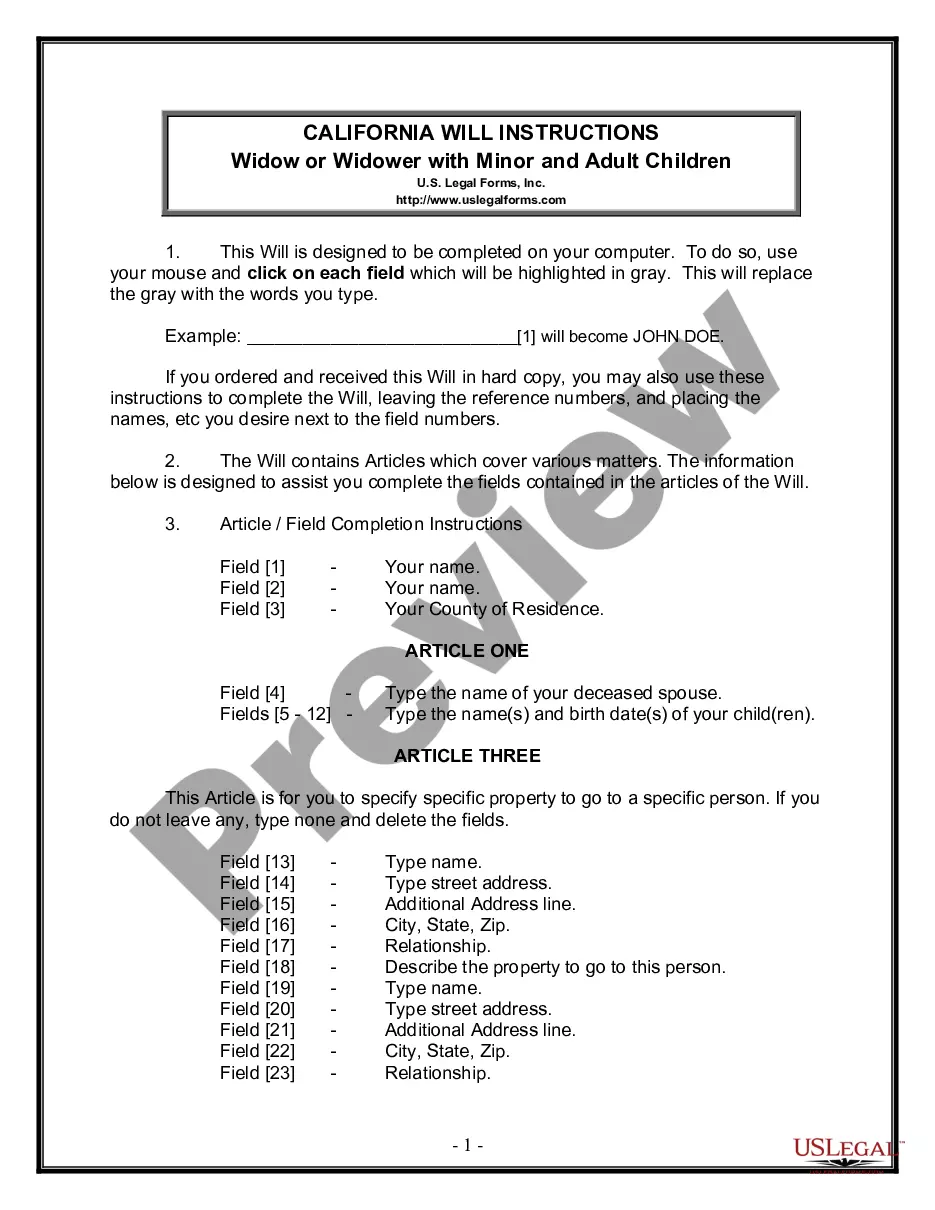
How to fill out General Notice Of Preexisting Condition Exclusion?
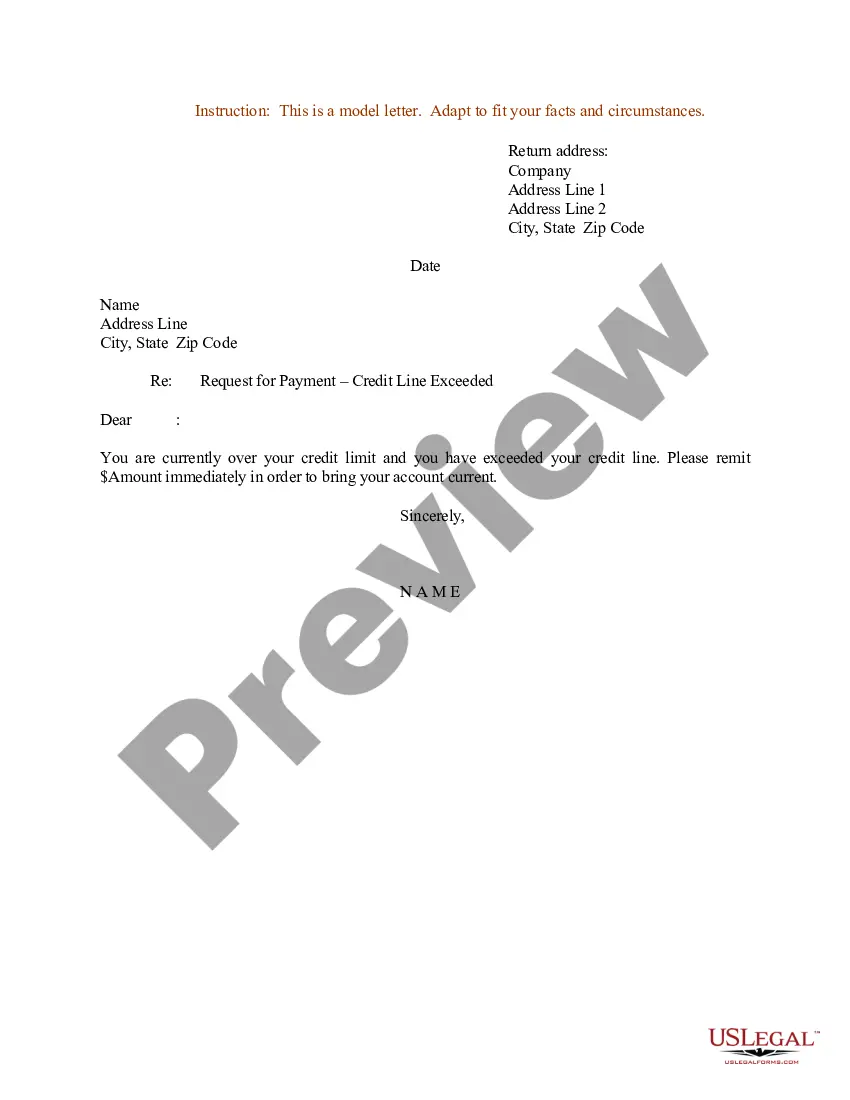
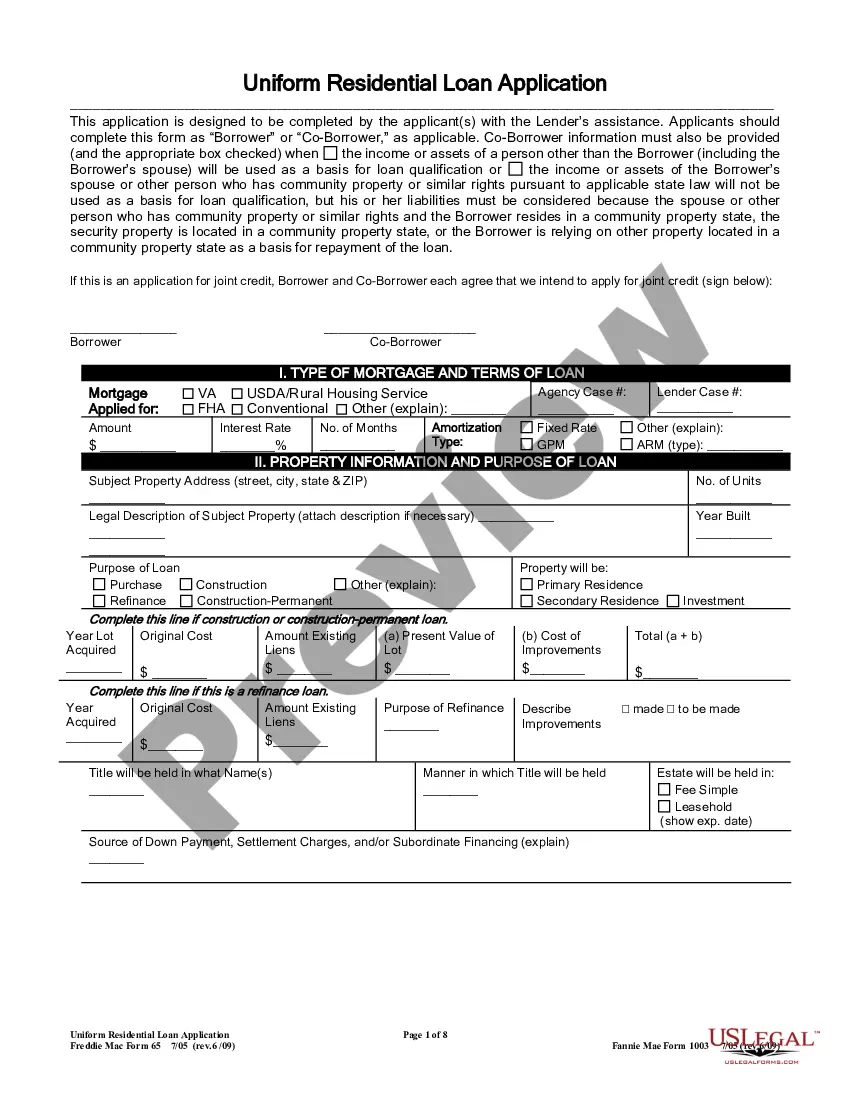
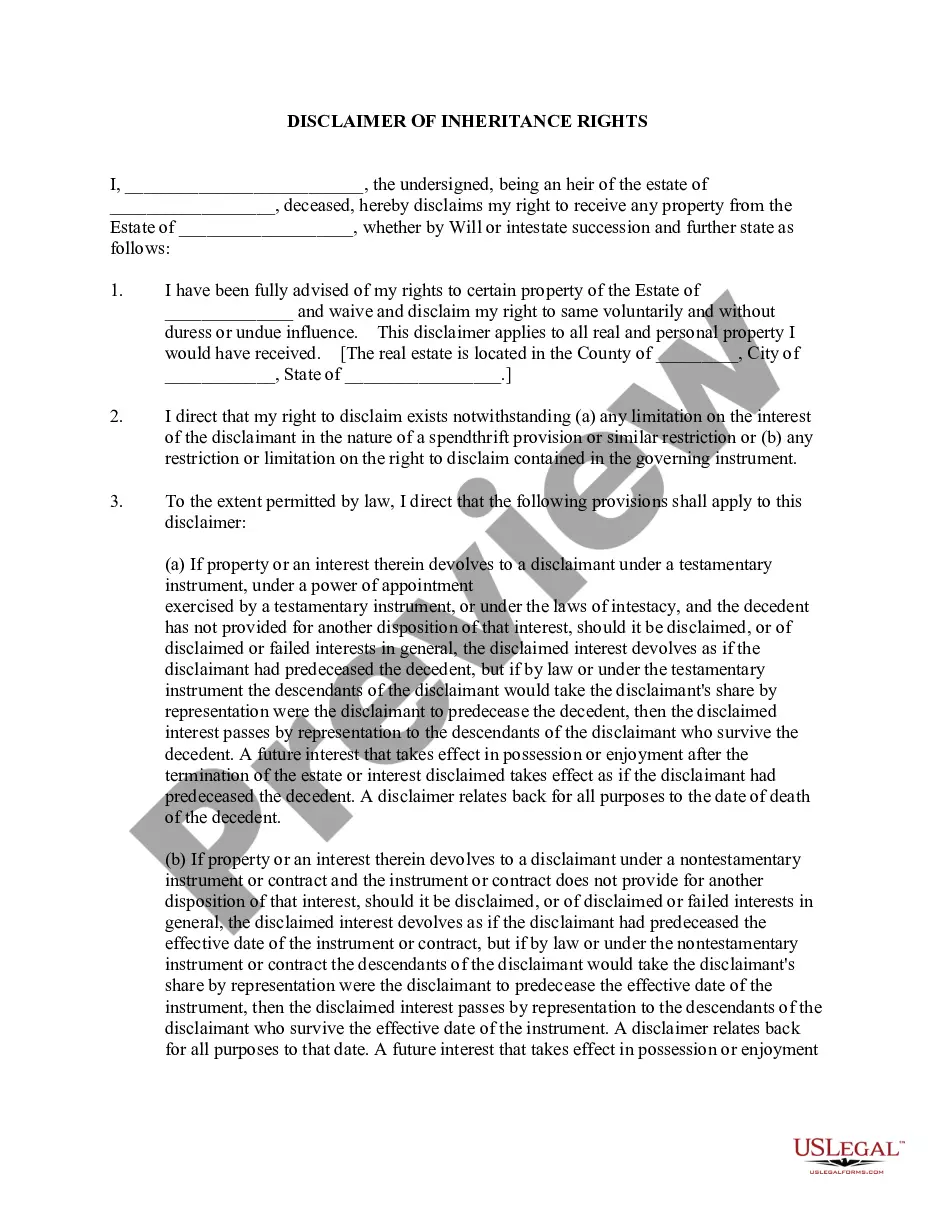
US Legal Forms - one of the largest collections of legal documents in the United States - offers a diverse selection of legal document templates that you can download or print.
By utilizing the website, you can access thousands of forms for business and personal applications, organized by categories, states, or keywords.
You can find the most recent versions of documents such as the District of Columbia General Notice of Preexisting Condition Exclusion in mere moments.
If the form does not meet your requirements, utilize the Search bar at the top of the page to find one that does.
Once you are satisfied with the form, confirm your selection by clicking the Get now button. Then, choose your preferred payment plan and provide your information to create an account.
- If you already possess a subscription, Log In to download the District of Columbia General Notice of Preexisting Condition Exclusion from your US Legal Forms library.
- The Obtain button will be displayed on every form you encounter.
- You can access all previously downloaded forms in the My documents section of your account.
- To utilize US Legal Forms for the first time, here are some simple instructions to begin.
- Ensure you have selected the correct form for your city/state.
- Click the Review button to examine the form's content.
Form popularity
FAQ
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
Conditions for Exclusion HIPAA did allow insurers to refuse to cover pre-existing medical conditions for up to the first 12 months after enrollment, or 18 months in the case of late enrollment.
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
It limits the time a new employer plan can exclude the pre-existing condition from being covered. An employer health plan can avoid covering costs of medical care for a pre-existing condition for no more than 12 months after the person is accepted into the plan.
A health problem, like asthma, diabetes, or cancer, you had before the date that new health coverage starts. Insurance companies can't refuse to cover treatment for your pre-existing condition or charge you more.
What Is the Pre-existing Condition Exclusion Period? The pre-existing condition exclusion period is a health insurance provision that limits or excludes benefits for a period of time. The determination is based on the policyholder having a medical condition prior to enrolling in a health plan.
Yes. Under the Affordable Care Act, health insurance companies can't refuse to cover you or charge you more just because you have a pre-existing condition that is, a health problem you had before the date that new health coverage starts.
The time period during which a health plan won't pay for care relating to a pre-existing condition. Under a job-based plan, this cannot exceed 12 months for a regular enrollee or 18 months for a late-enrollee.