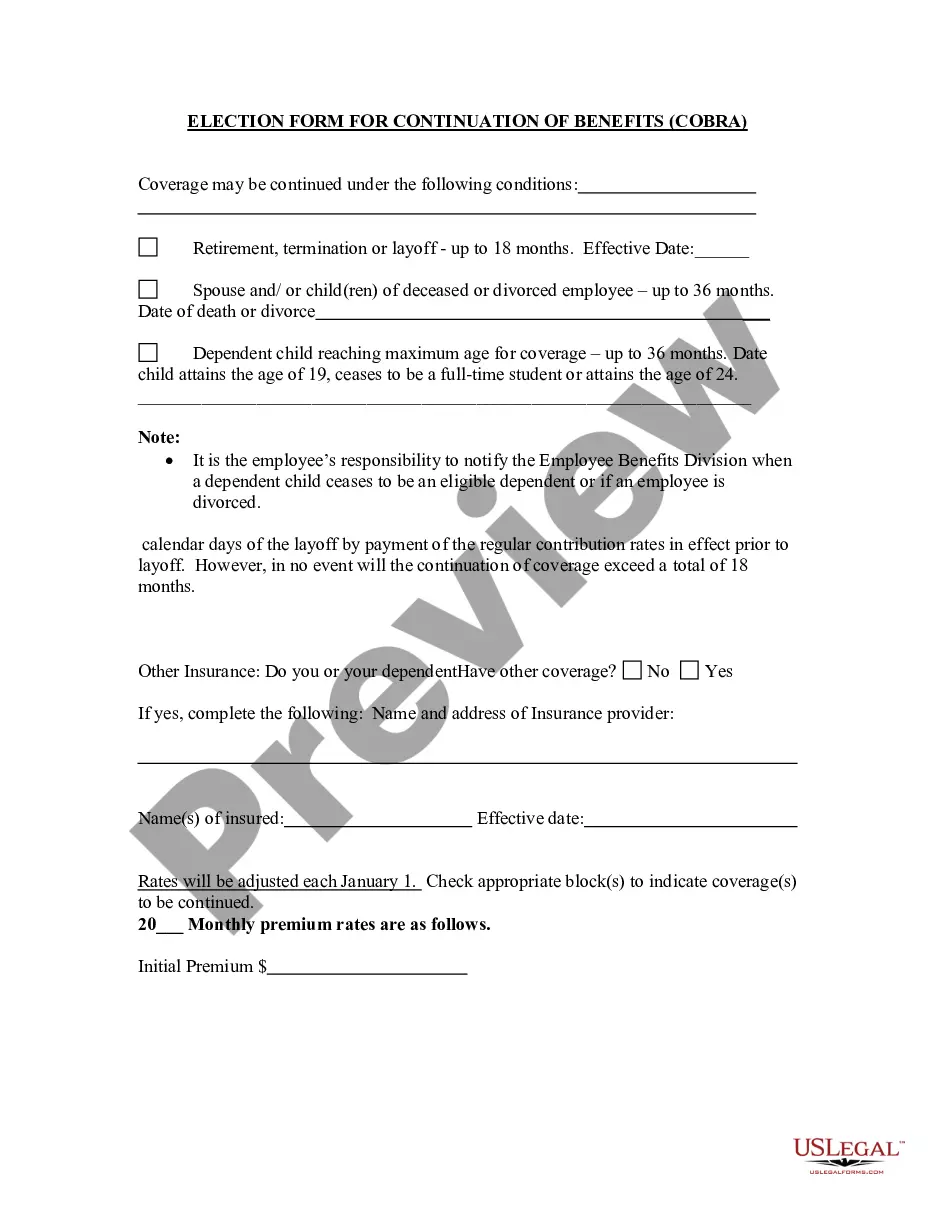
Connecticut Election Form for Continuation of Benefits - COBRA
Description
How to fill out Election Form For Continuation Of Benefits - COBRA?
Are you presently in a situation where you require documents for potentially organizational or personal purposes almost every day.
There are numerous legal document templates available online, but finding reliable ones can be challenging.
US Legal Forms offers a vast collection of form templates, including the Connecticut Election Form for Continuation of Benefits - COBRA, which can be tailored to comply with federal and state regulations.
Once you find the correct form, click Acquire now.
Select the pricing plan you prefer, fill in the necessary information to create your account, and pay for the order using your PayPal or credit card. Choose a convenient file format and download your copy.
- If you are familiar with the US Legal Forms site and have an account, simply Log In.
- Then, you can download the Connecticut Election Form for Continuation of Benefits - COBRA format.
- If you do not have an account and wish to start using US Legal Forms, follow these steps.
- Find the form you need and ensure it is for your correct city/region.
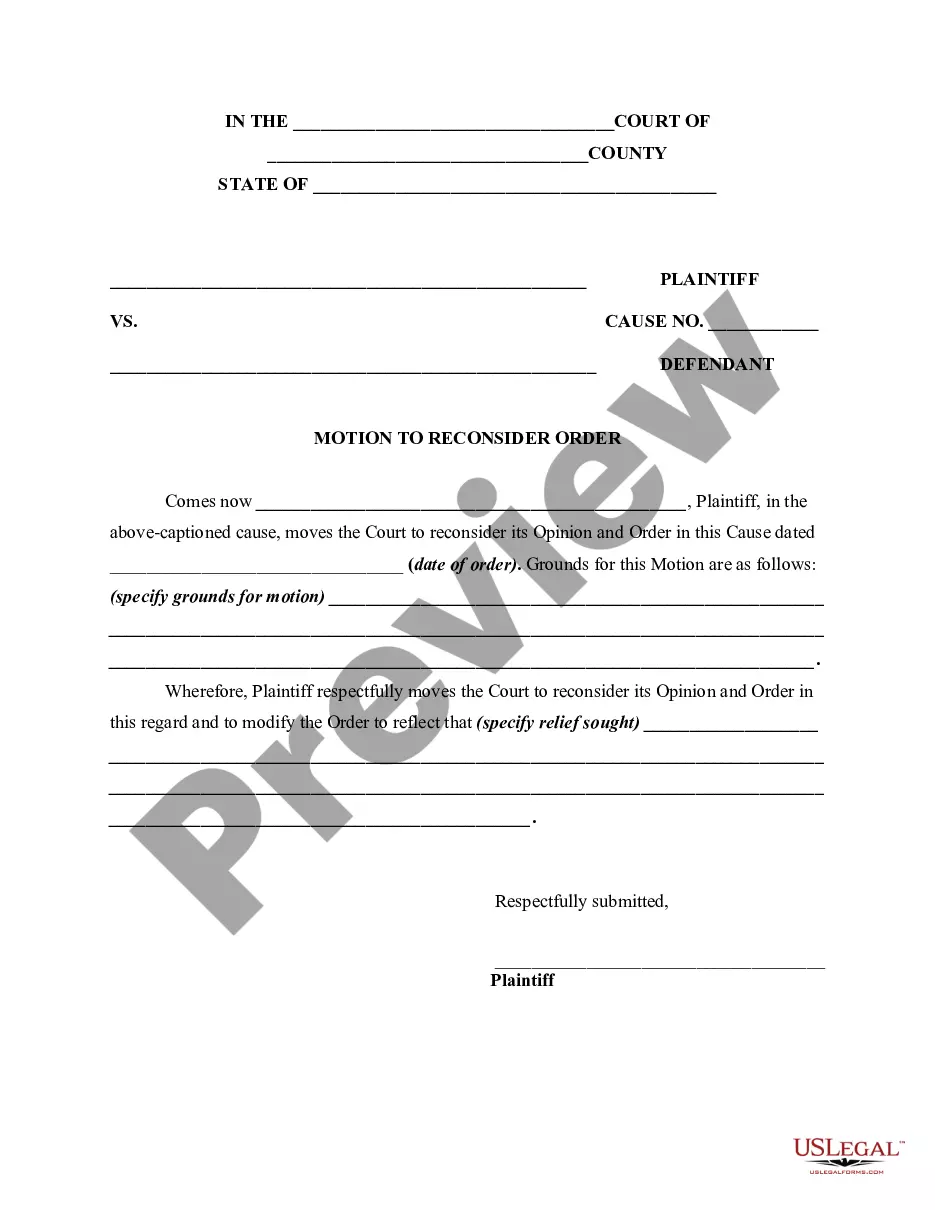
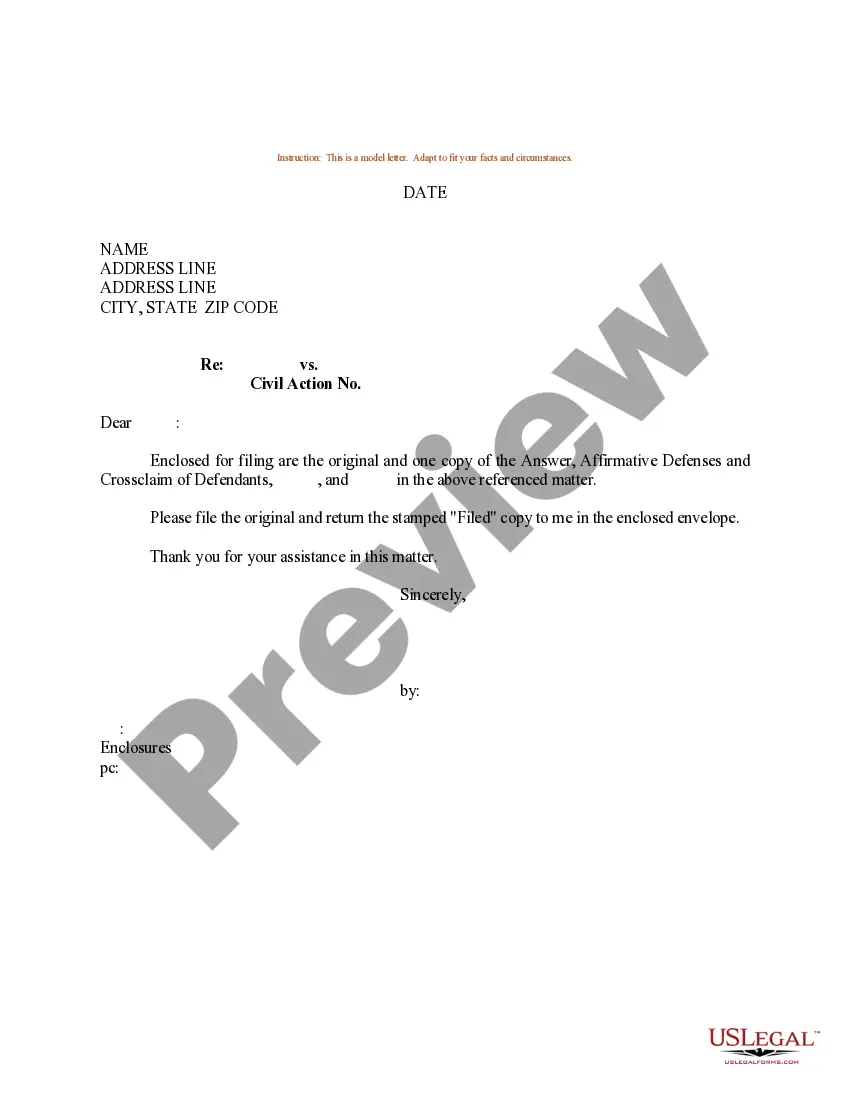
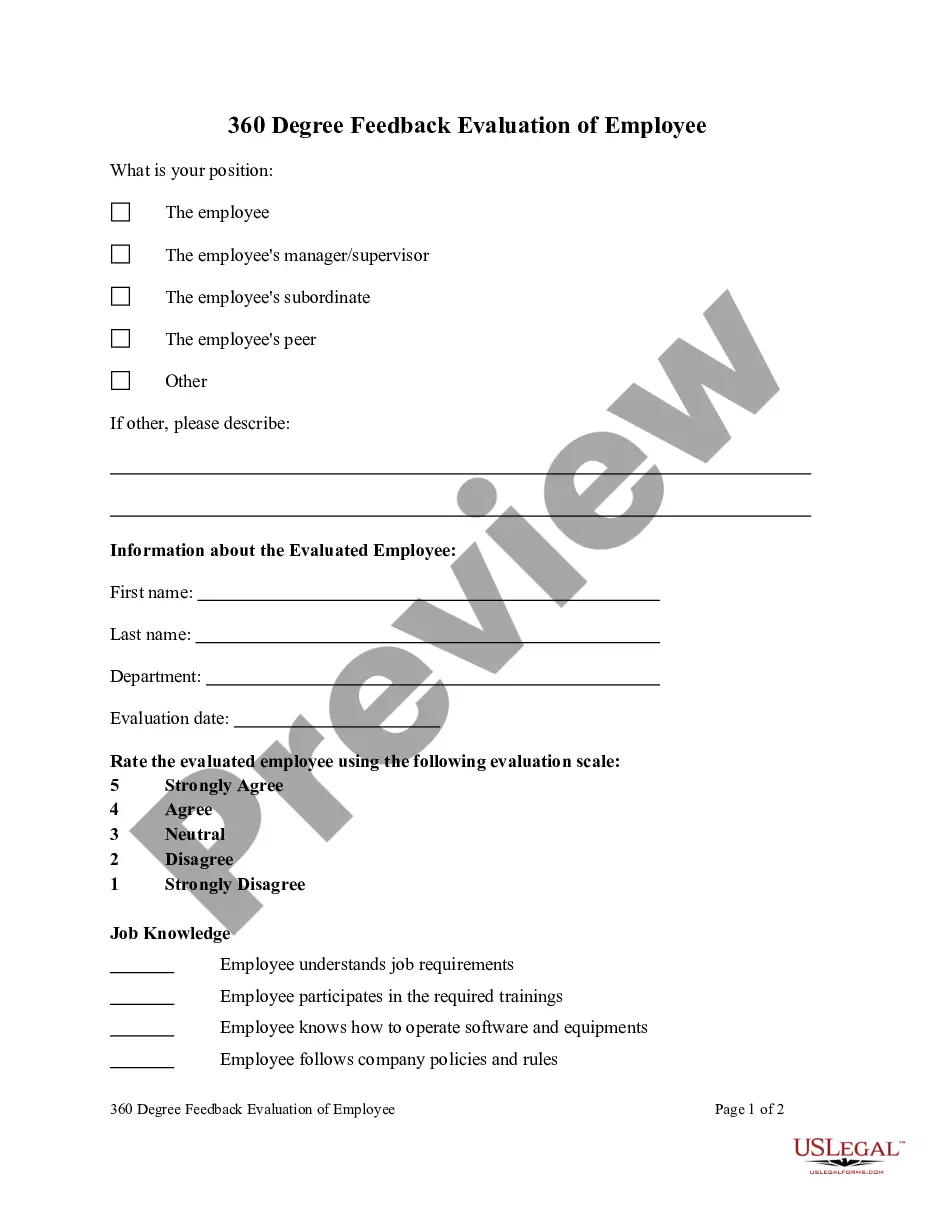
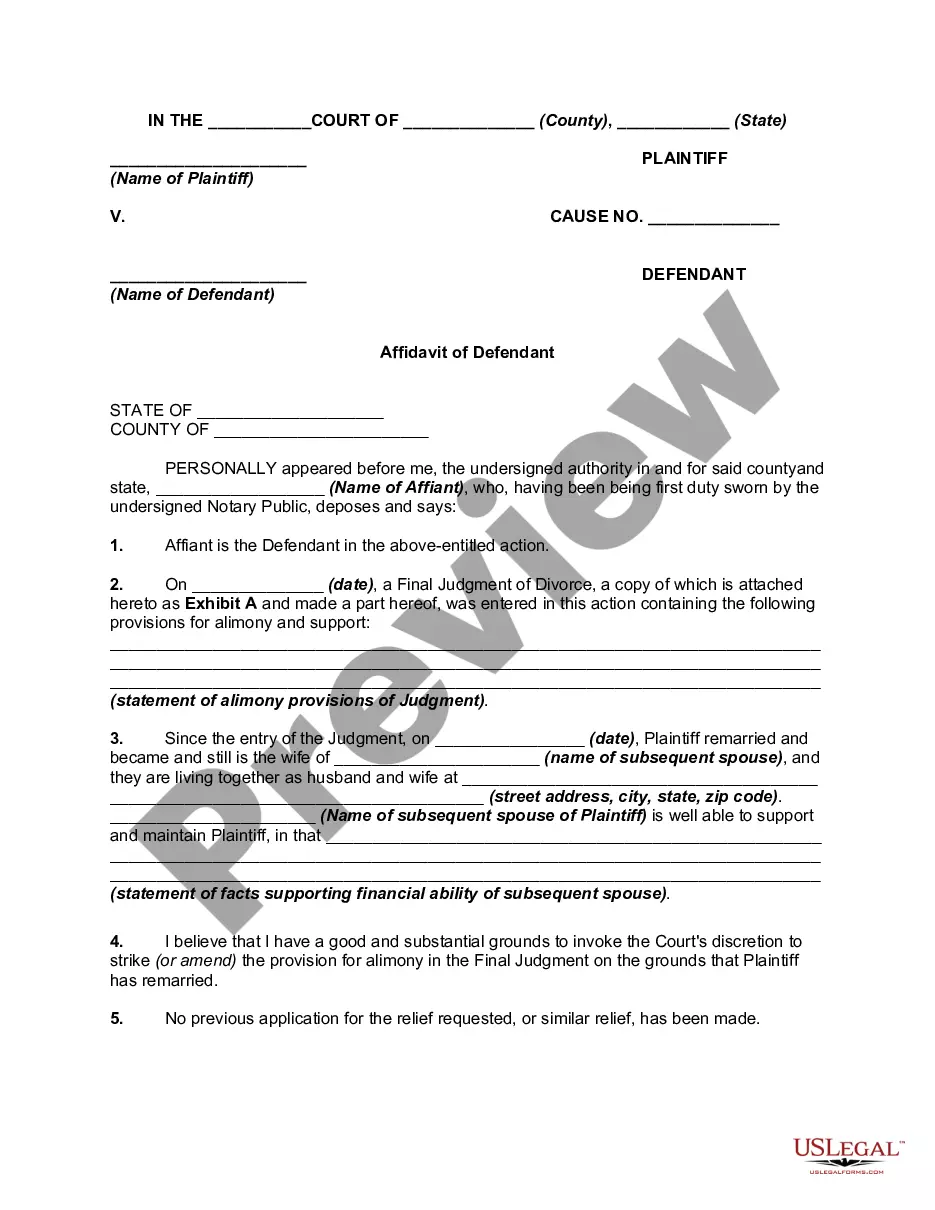
- Use the Review button to examine the form.
- Check the description to confirm you have selected the right form.
- If the form is not what you’re looking for, use the Search field to find the form that meets your needs and requirements.
Form popularity
FAQ
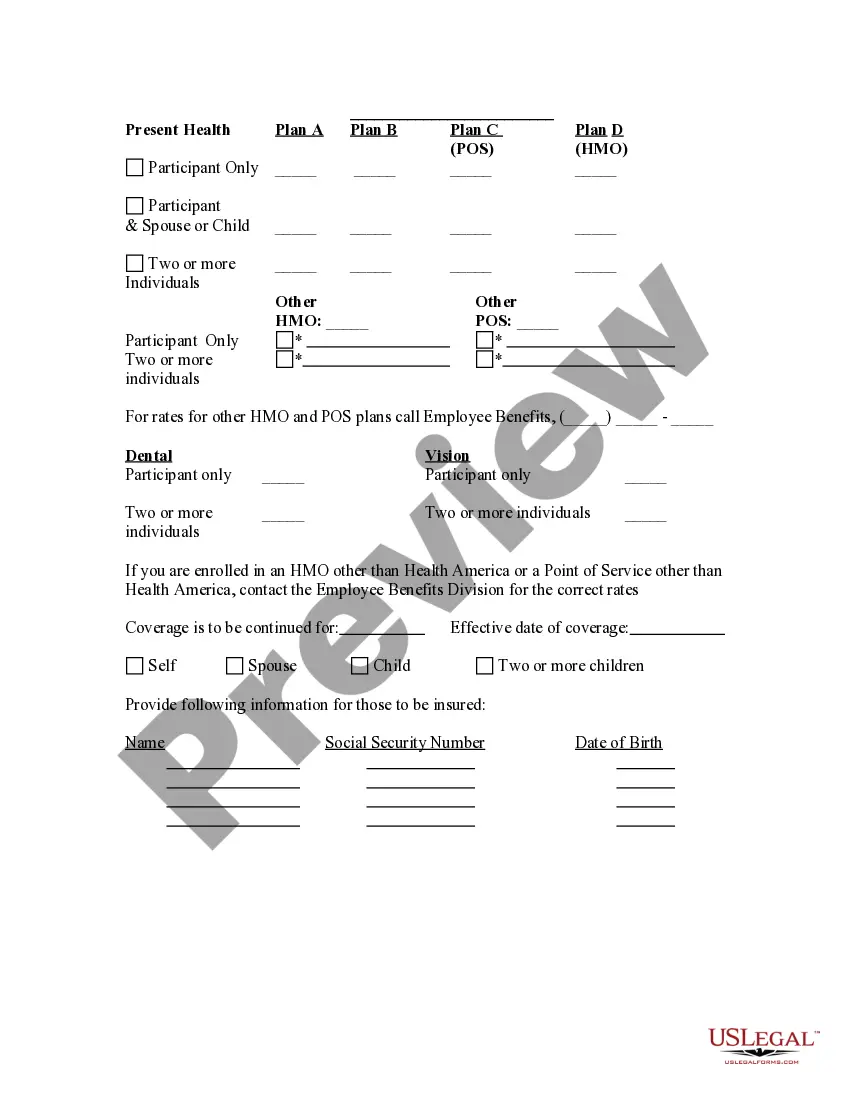
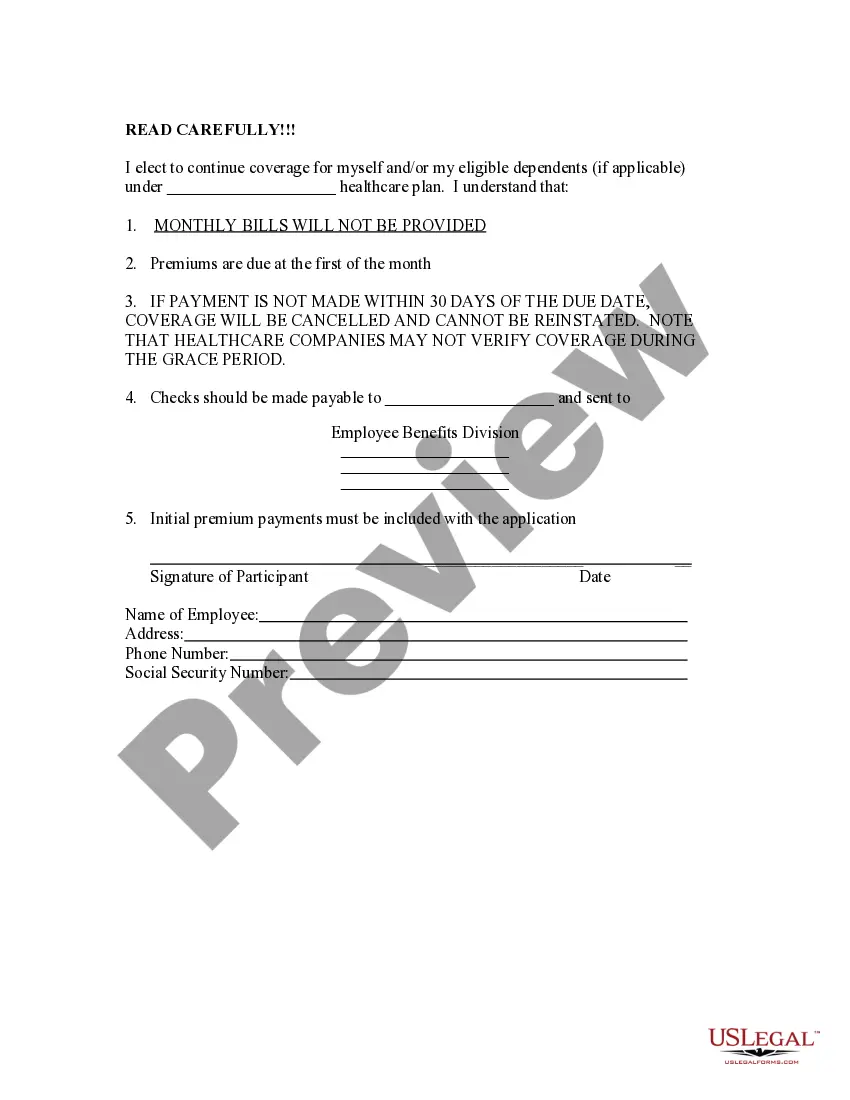
COBRA permits you and your dependents to continue in your employer's group health plan after your job ends. If your employer has 20 or more employees, you may be eligible for COBRA continuation coverage when you retire, quit, are fired, or work reduced hours.
COBRA continuation coverage generally lasts 18 months, or 36 months for dependents in certain circumstances.
How Long Does COBRA Last After You Quit? You may remain on your former employer's COBRA insurance plan for up to 18 months. Depending on your circumstances you or your qualified dependents may be eligible for up to 36 months of continuing coverage.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
COBRA continuation coverage lets you stay on your employer's group health insurance plan after leaving your job. COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. It's shorthand for the law change that required employers to extend temporary group health insurance to departing employees.
Employees covered under employer groups with 20 or more employees are granted the right to continue coverage subject to Federal COBRA provisions for 18 months.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.