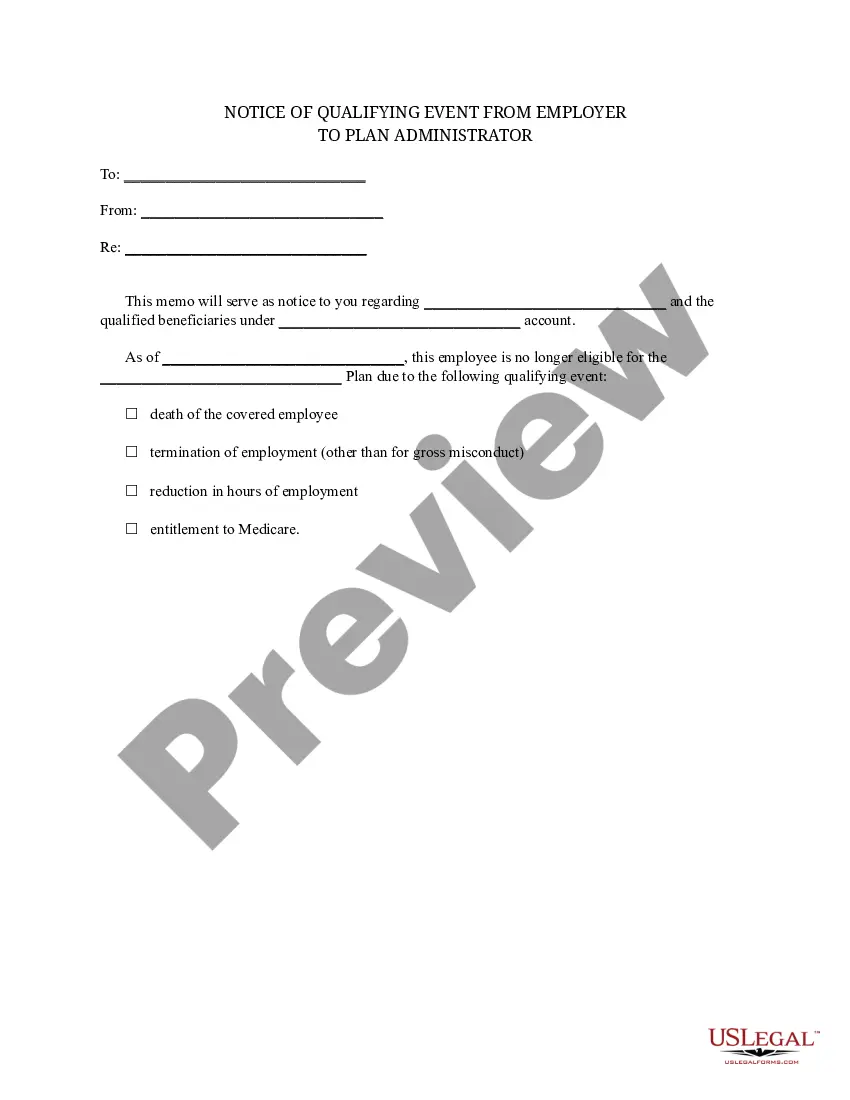
Colorado Notice of Qualifying Event from Employer to Plan Administrator
Description
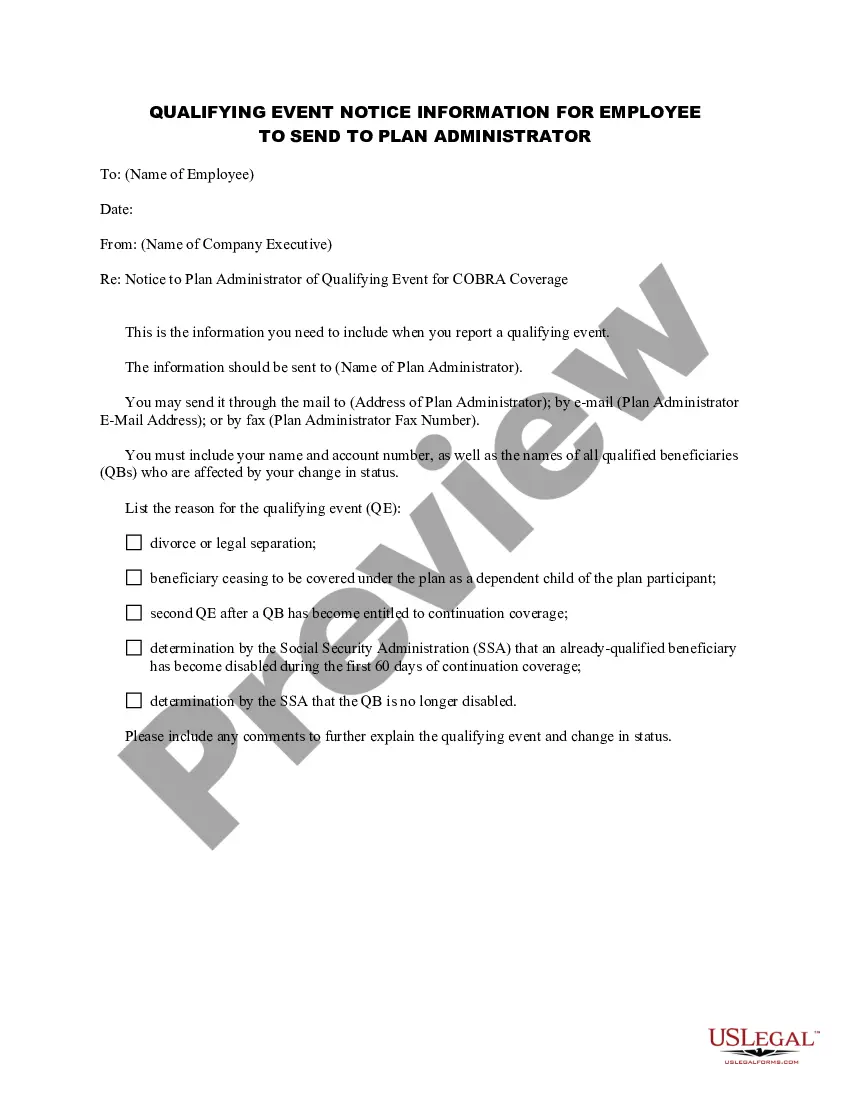
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
You can spend hours online trying to locate the legal document template that meets the federal and state specifications you require.
US Legal Forms offers thousands of legal forms that can be reviewed by experts.
You can easily download or print the Colorado Notice of Qualifying Event from Employer to Plan Administrator from our service.
If available, utilize the Preview button to view the document template as well.
- If you already possess a US Legal Forms account, you may Log In and click the Download button.
- Then, you can complete, modify, print, or sign the Colorado Notice of Qualifying Event from Employer to Plan Administrator.
- Every legal document template you purchase is yours indefinitely.
- To obtain another copy of any purchased form, navigate to the My documents tab and click the corresponding button.
- If you are using the US Legal Forms website for the first time, follow the simple instructions below.
- First, ensure that you have selected the correct document template for the county/city of your choice.
- Review the form description to confirm you have chosen the correct document.
Form popularity
FAQ
Colorado Continuation is the state alternative to COBRA intended to fill some gaps such as when a company has fewer than 20 employees or the covered employee's termination was due to gross misconduct. Unlike COBRA, the Colorado Continuation Coverage is available as an option only if the employee has been
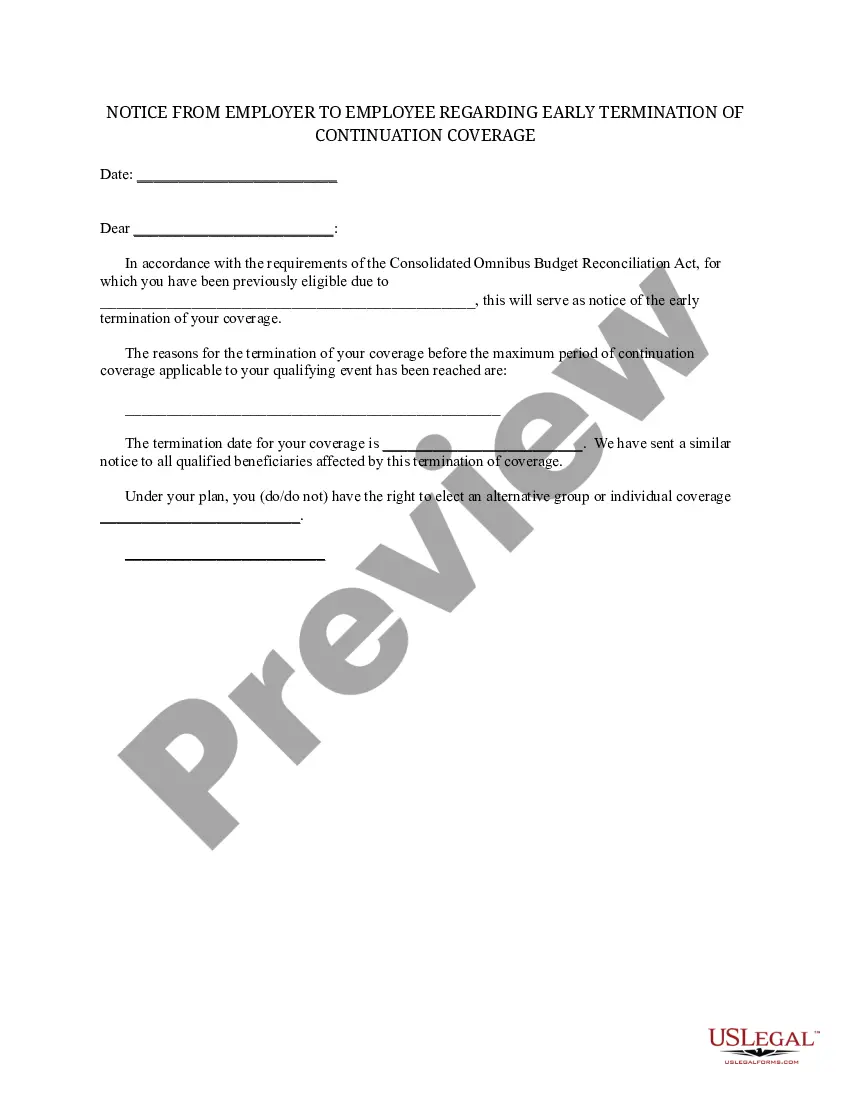
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
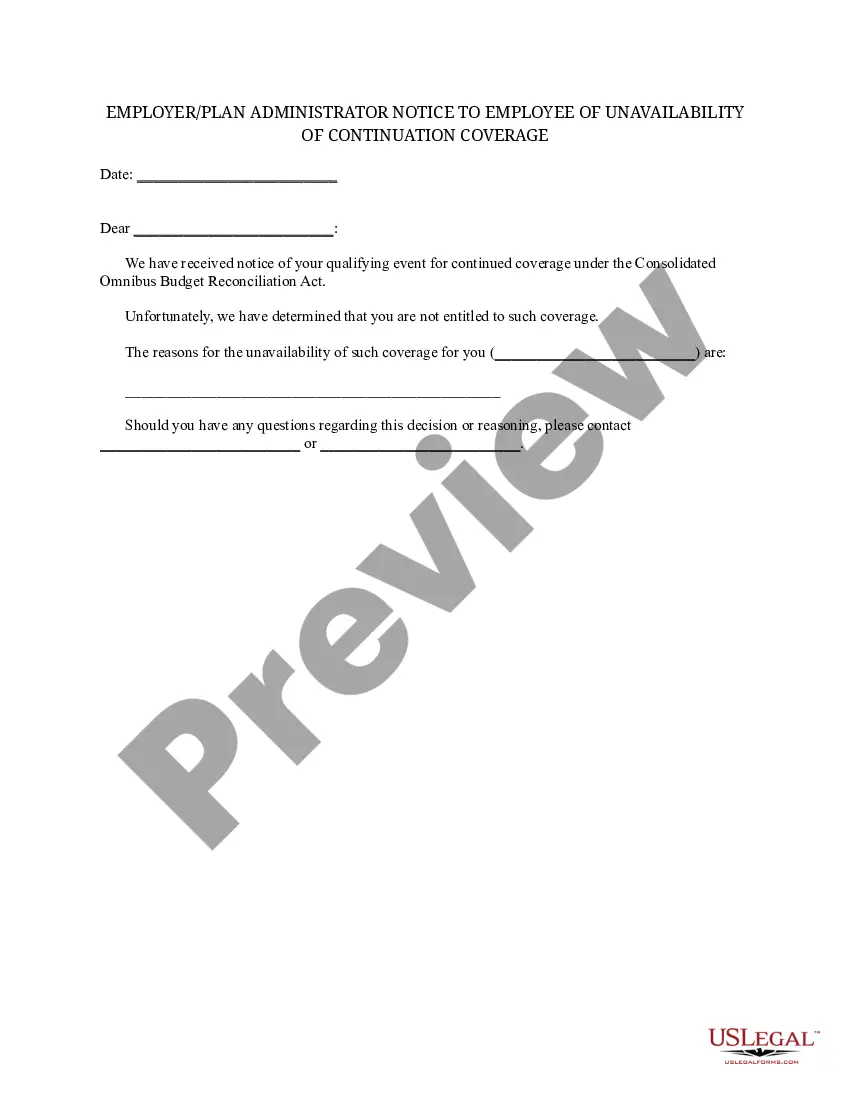
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.
COBRA and Colorado Continuation Coverage allow you to keep the same employer-provided plan you know, with the same benefits and doctors, for up to 18 months (in some cases you can extend COBRA up to 36 months).
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Colorado Continuation Coverage is available if an employee has been continuously covered under the employer's plan for six consecutive months. If covered for less than six months but more than three months, conversion is available.