California Notice of Qualifying Event from Employer to Plan Administrator
Description
How to fill out Notice Of Qualifying Event From Employer To Plan Administrator?
If you want to thoroughly access, acquire, or print authorized document templates, use US Legal Forms, the largest array of legal forms available online.
Take advantage of the site's straightforward and user-friendly search feature to locate the documents you require.
Various templates for both business and personal purposes are organized by categories and states, or by keywords.
Step 4. Once you have found the required form, click on the Purchase now button. Choose the pricing plan you prefer and enter your details to create an account.
Step 5. Complete the transaction. You can use your credit card or PayPal account to finalize the purchase.
- Employ US Legal Forms to quickly find the California Notice of Qualifying Event from Employer to Plan Administrator.
- If you are already a US Legal Forms customer, Log Into your account and click the Download button to access the California Notice of Qualifying Event from Employer to Plan Administrator.
- You can also view forms you have previously purchased in the My documents section of your account.
- If you are using US Legal Forms for the first time, follow these instructions.
- Step 1. Ensure that you have selected the form for the correct area/state.
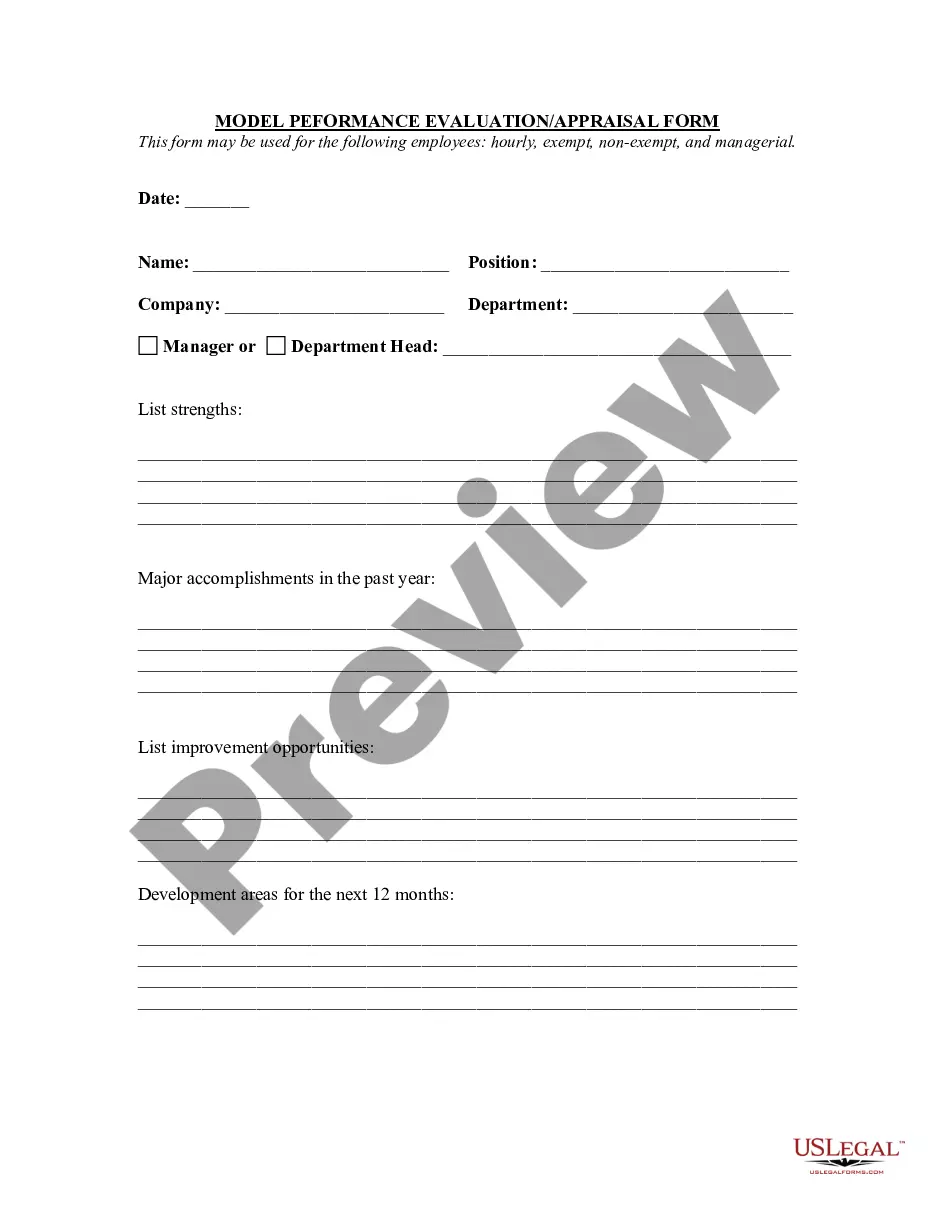
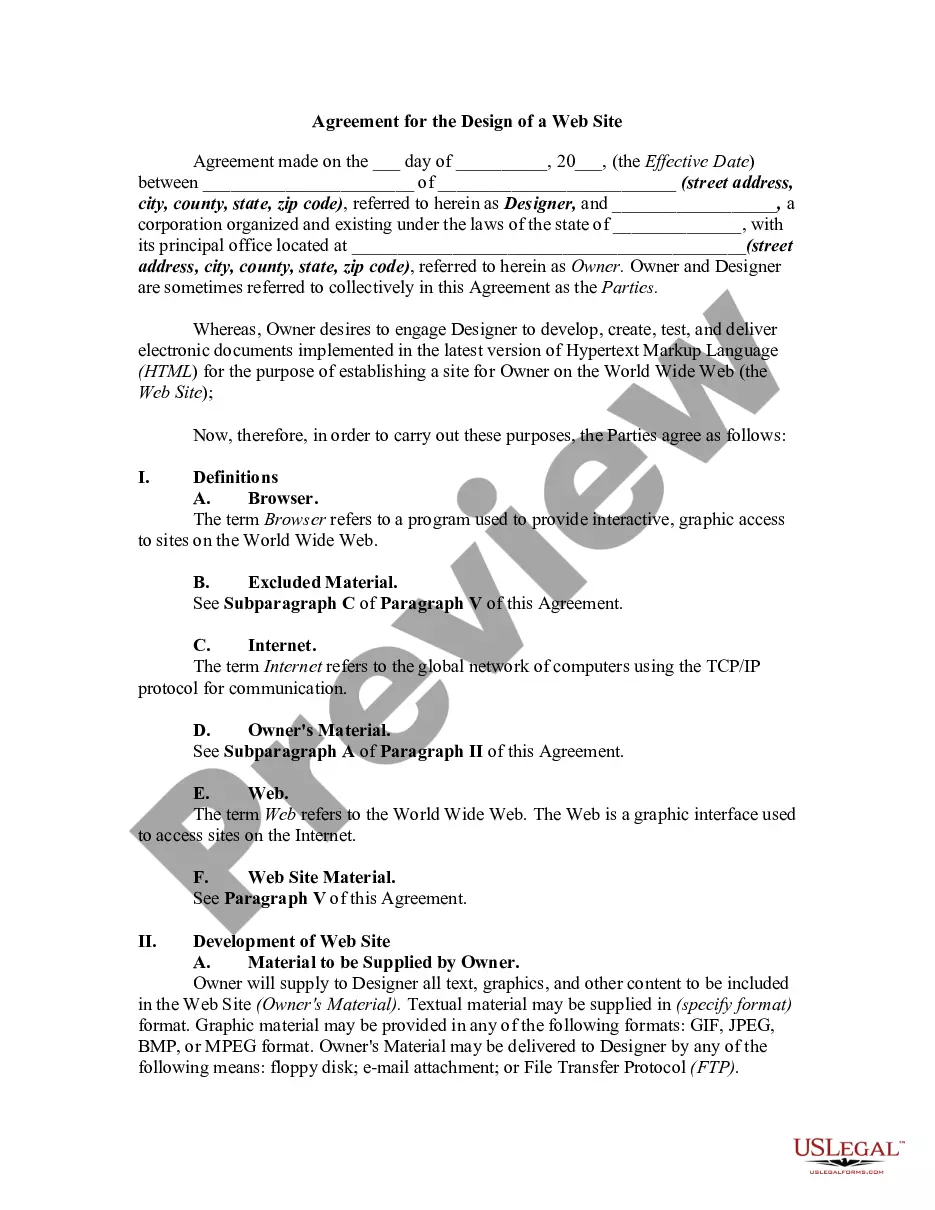
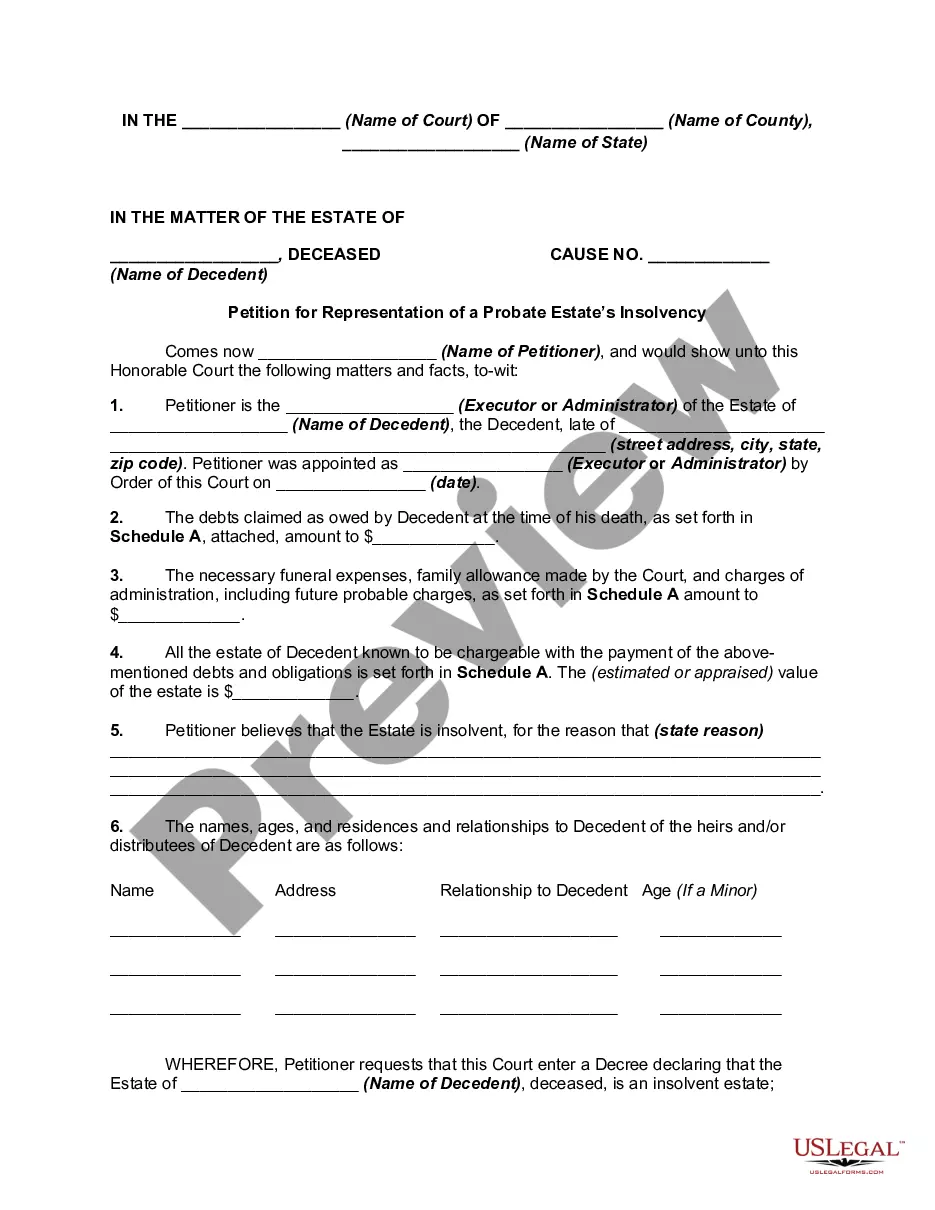
- Step 2. Use the Review option to examine the form's content. Remember to read the details.
- Step 3. If you are not satisfied with the form, utilize the Search field at the top of the screen to find different types within the legal form category.
Form popularity
FAQ
Cal-COBRA administration requires four basic compliance components: Notifying all eligible group health care participants of their Cal-COBRA rights. Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.
Losing COBRA Benefits Here's the good news: Rolling off of COBRA coverage is a qualifying event that opens a special enrollment period for you to purchase your own health coverage. And you'll have more options, flexibility and control of your health plan outside of COBRA with an individual health insurance plan.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Model COBRA notices are provided on the U.S. Department of Labor's COBRA Continuation webpage under the Regulations section.Step 1: Initial Notification.Step 2: Qualifying Event Notices.Step 3: Insurance Carrier Notification.Step 4: Election and Payment.Step 5 (if needed): Late or Missing Payments.More items...
How to Administer Cal-COBRANotifying all eligible group health care participants of their Cal-COBRA rights.Providing timely notice of Cal-COBRA eligibility, enrollment forms, and notice of the duration of coverage and terms of payment after a qualifying event has occurred.More items...
Covered Employers Under federal COBRA, employers with 20 or more employees are usually required to offer COBRA coverage. COBRA applies to plans maintained by private-sector employers (including self-insured plans) and those sponsored by most state and local governments.
When the qualifying event is the covered employee's termination of employment or reduction in hours of employment, qualified beneficiaries are entitled to 18 months of continuation coverage.
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
Second qualifying events may include the death of the covered employee, divorce or legal separation from the covered employee, the covered employee becoming entitled to Medicare benefits (under Part A, Part B or both), or a dependent child ceasing to be eligible for coverage as a dependent under the group health plan.
COBRA Qualifying Event Notice The employer must notify the plan if the qualifying event is: Termination or reduction in hours of employment of the covered employee, 2022 Death of the covered employee, 2022 Covered employee becoming entitled to Medicare, or 2022 Employer bankruptcy.