Arkansas COBRA Continuation Coverage Election Form
Description
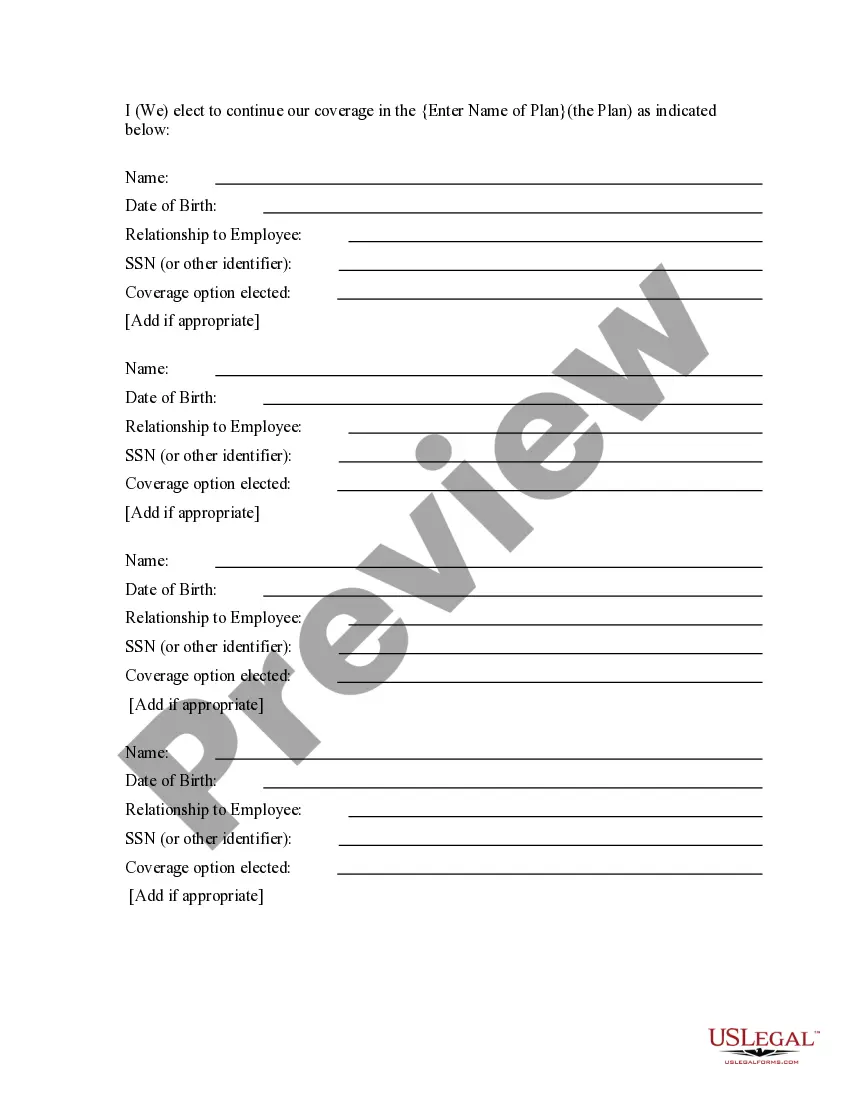
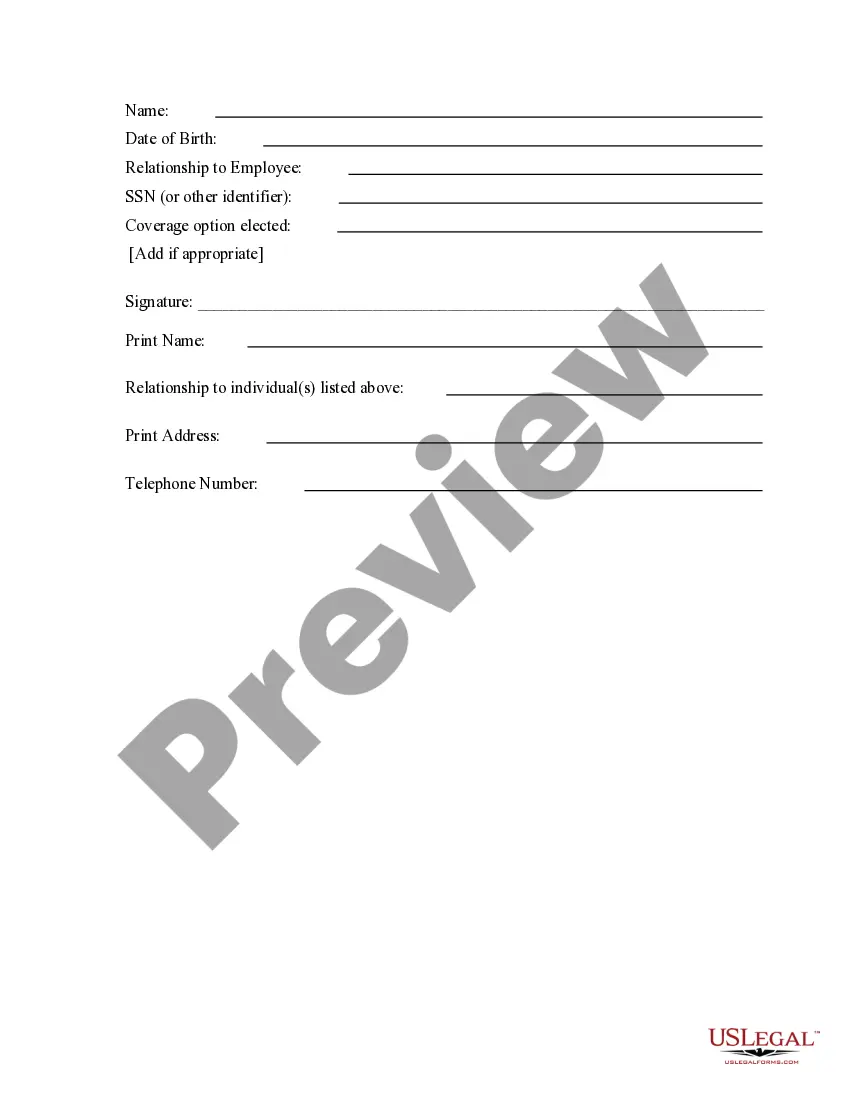
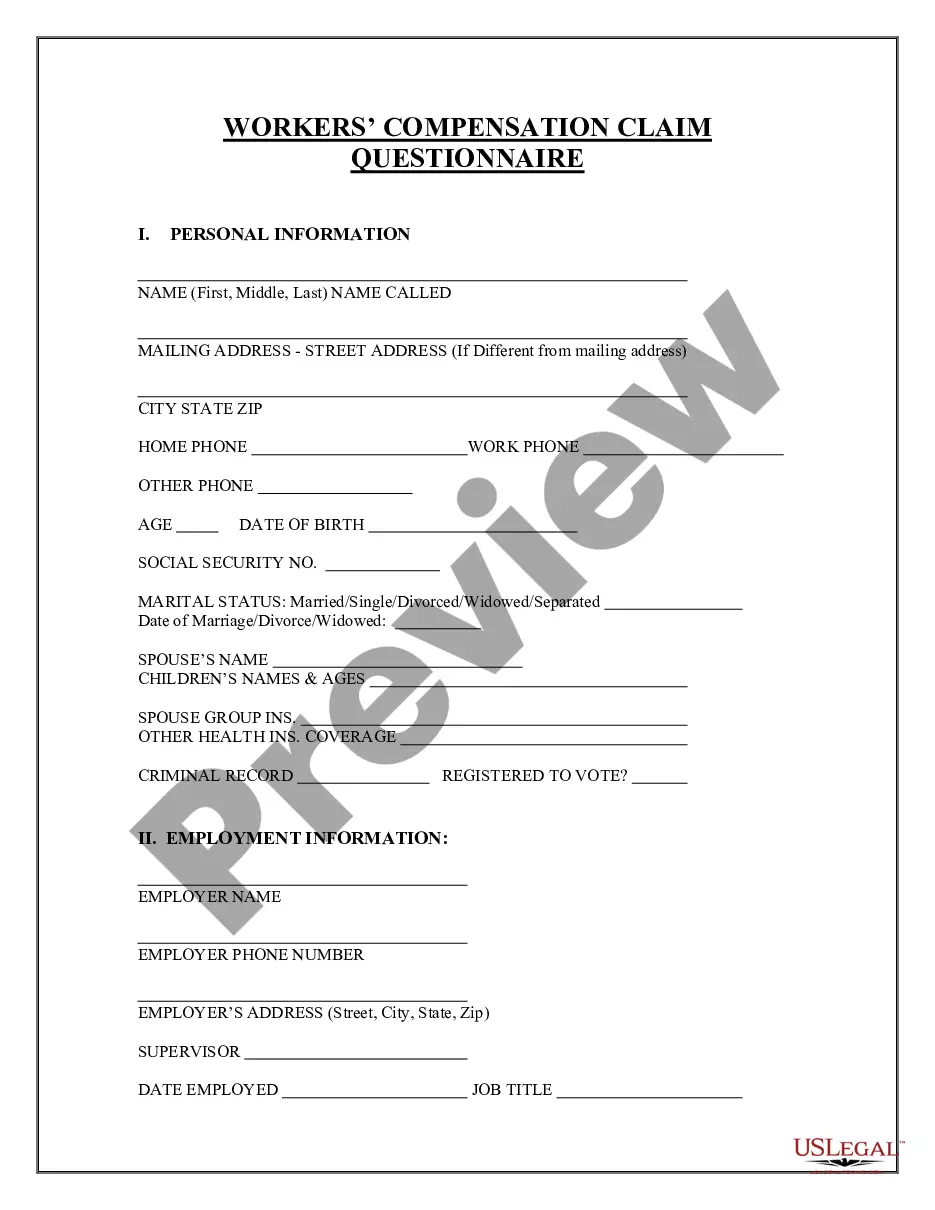
How to fill out COBRA Continuation Coverage Election Form?
US Legal Forms - one of the largest collections of legal documents in the USA - offers a diverse selection of legal form templates that you can download or print.
By using the website, you can access thousands of forms for business and personal use, categorized by types, states, or keywords. You can find the latest versions of forms like the Arkansas COBRA Continuation Coverage Election Form in no time.
If you have a subscription, Log In to download the Arkansas COBRA Continuation Coverage Election Form from the US Legal Forms library. The Download button will appear on each form you view. You can access all previously downloaded forms from the My documents section of your account.
Once downloaded, you can fill out, edit, print, and sign the Arkansas COBRA Continuation Coverage Election Form.
All templates you added to your account have no expiration date and are yours permanently. Therefore, to download or print another copy, simply visit the My documents section and click on the form you need.
- If you are using US Legal Forms for the first time, here are simple steps to get started.
- Ensure you have selected the correct form for your region/county. Click the Review button to check the contents of the form. Look at the form summary to confirm you have chosen the right document.
- If the form does not meet your requirements, utilize the Search area at the top of the page to find one that does.
- Once you are satisfied with the form, confirm your selection by clicking the Purchase now button. Then, choose the payment plan you prefer and provide your details to register for an account.
- Process the payment. Use your credit card or PayPal account to complete the transaction.
- Select the format and download the document to your device.
Form popularity
FAQ
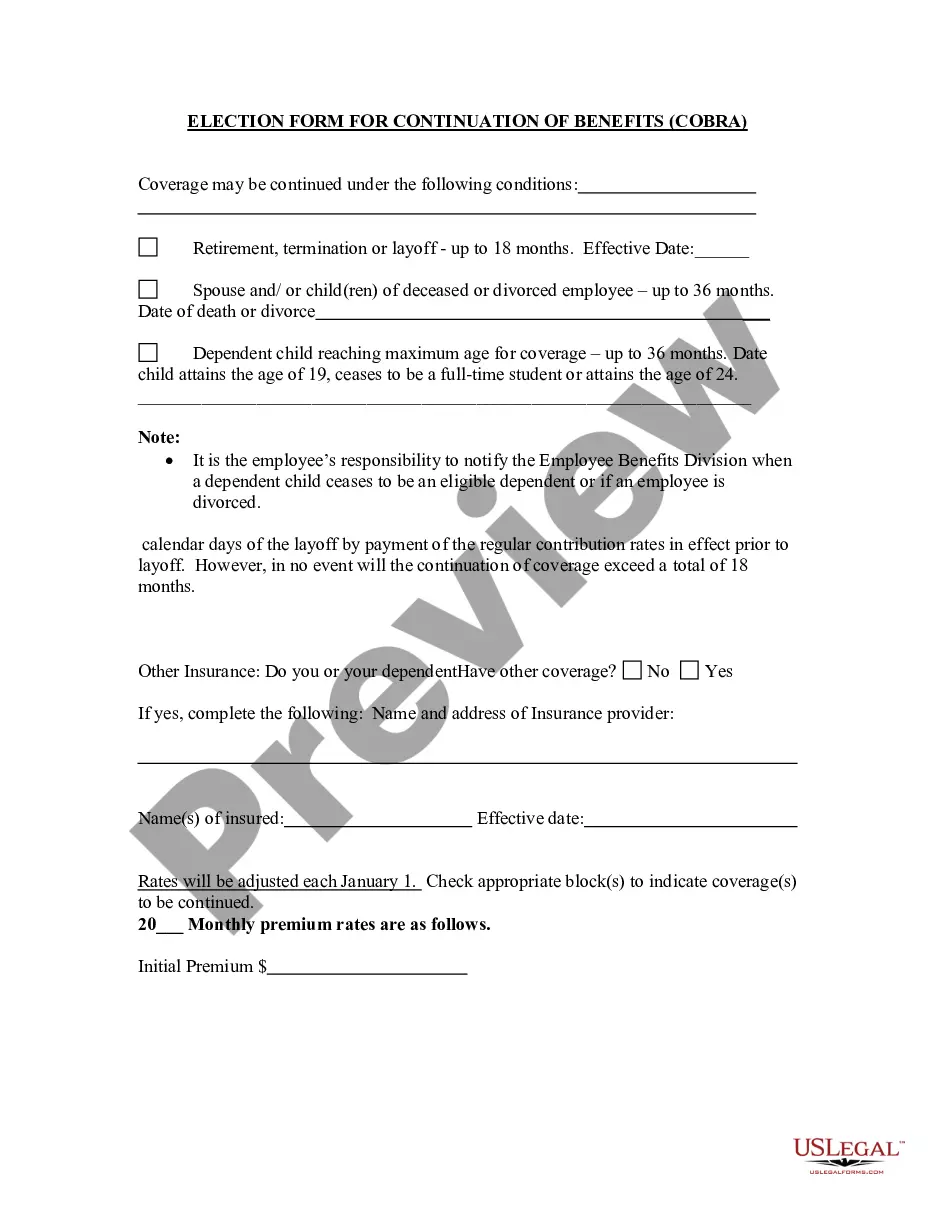
When does COBRA continuation coverage startCOBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
COBRA is always retroactive to the day after your previous coverage ends, and you'll need to pay your premiums for that period too. One advantage of enrolling right away is that you can keep seeing doctors and filling prescriptions without a break in coverage. COBRA allows you to keep the exact same benefits as before.
The qualifying event for COBRA purposes is the employee's loss of employment date. However, the election period does not end until 60 days from the sent date of the election form to the employee or until 60 days after the loss of coverage, whichever is later.
Qualified beneficiaries must be given an election period of at least 60 days during which each qualified beneficiary may choose whether to elect COBRA coverage. This period is measured from the later of the date of the qualifying event or the date the COBRA election notice is provided.
COBRA requires that continuation coverage extend from the date of the qualifying event for a limited period of 18 or 36 months. The length of time depends on the type of qualifying event that gave rise to Page 6 6 the COBRA rights.
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
State continuation coverage refers to state laws that allow people to extend their employer-sponsored health insurance even if they're not eligible for extension via COBRA. As a federal law, COBRA applies nationwide, but only to employers with 20 or more employees.