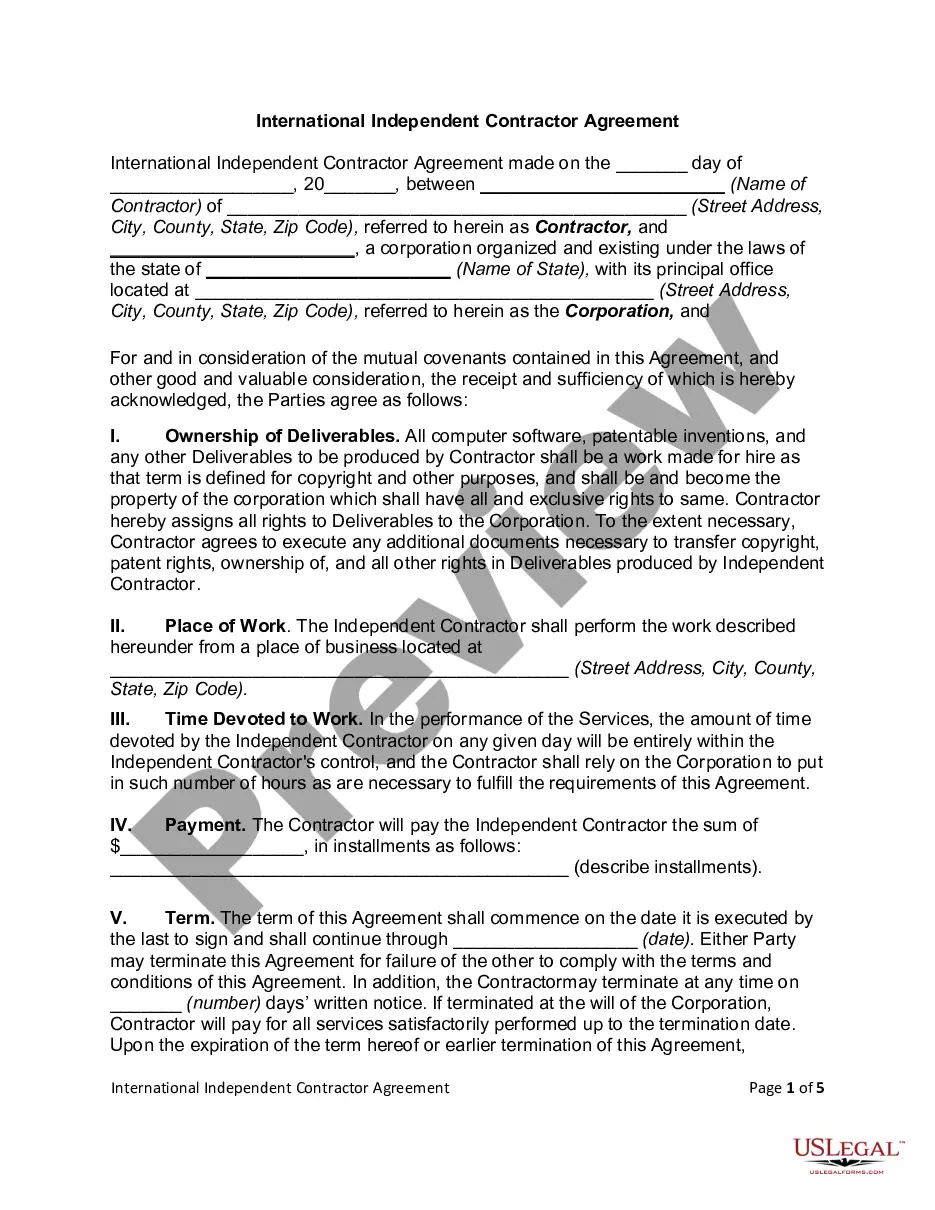
Alaska Level 2 Appeal of Medical Necessity Denial — Request for External Review is a process by which an individual or organization may challenge a denial of coverage for a medical service or supply by their insurance provider. This appeal is completed by submitting a written request to the Alaska Division of Insurance. The request must include the denial letter from the insurance provider, the reasons for the denial, and the reason(s) for the appeal. The division will then forward the request to an independent external review organization, who will review the denial and provide a recommendation to the division. The division will then make a decision based on the recommendation. There are two types of external review: expedited and standard. The expedited review process is completed within seven days, while the standard review process can take up to 45 days.
Alaska Level 2 Appeal of Medical Necessity Denial - Request for External Review
Instant download
Public form
Description
This official form is a level 2 appeal of medical necessity denial - request for external review.
How to fill out Alaska Level 2 Appeal Of Medical Necessity Denial - Request For External Review?
If you’re seeking a method to adequately finalize the Alaska Level 2 Appeal of Medical Necessity Rejection - Request for External Review without engaging a legal representative, then you’re in the perfect location.
US Legal Forms has established itself as the most extensive and dependable repository of official templates for every individual and business context. Each document you discover on our online platform is crafted in accordance with nationwide and state regulations, ensuring that your paperwork is in order.
Another excellent benefit of US Legal Forms is that you won’t lose the paperwork you obtained - you can access any of your downloaded templates in the My documents section of your profile whenever you require it.
- Verify that the document displayed on the page aligns with your legal circumstances and state regulations by reviewing its text description or exploring the Preview mode.
- Enter the document title in the Search tab at the top of the page and select your state from the dropdown to locate another template if there are any discrepancies.
- Repeat the content validation and click Buy now when you are assured of the paperwork’s compliance with all the stipulations.
- Log In to your account and select Download. If you haven’t registered yet, sign up for the service and choose a subscription plan.
- Utilize your credit card or the PayPal option to settle the payment for your US Legal Forms subscription. The document will be available for download immediately after.
- Decide in which format you wish to receive your Alaska Level 2 Appeal of Medical Necessity Rejection - Request for External Review and download it by clicking the relevant button.
- Import your template to an online editor for quick completion and signing or print it out to prepare your hard copy manually.