Release Of Information Without Consent In Los Angeles
Description
Form popularity
FAQ
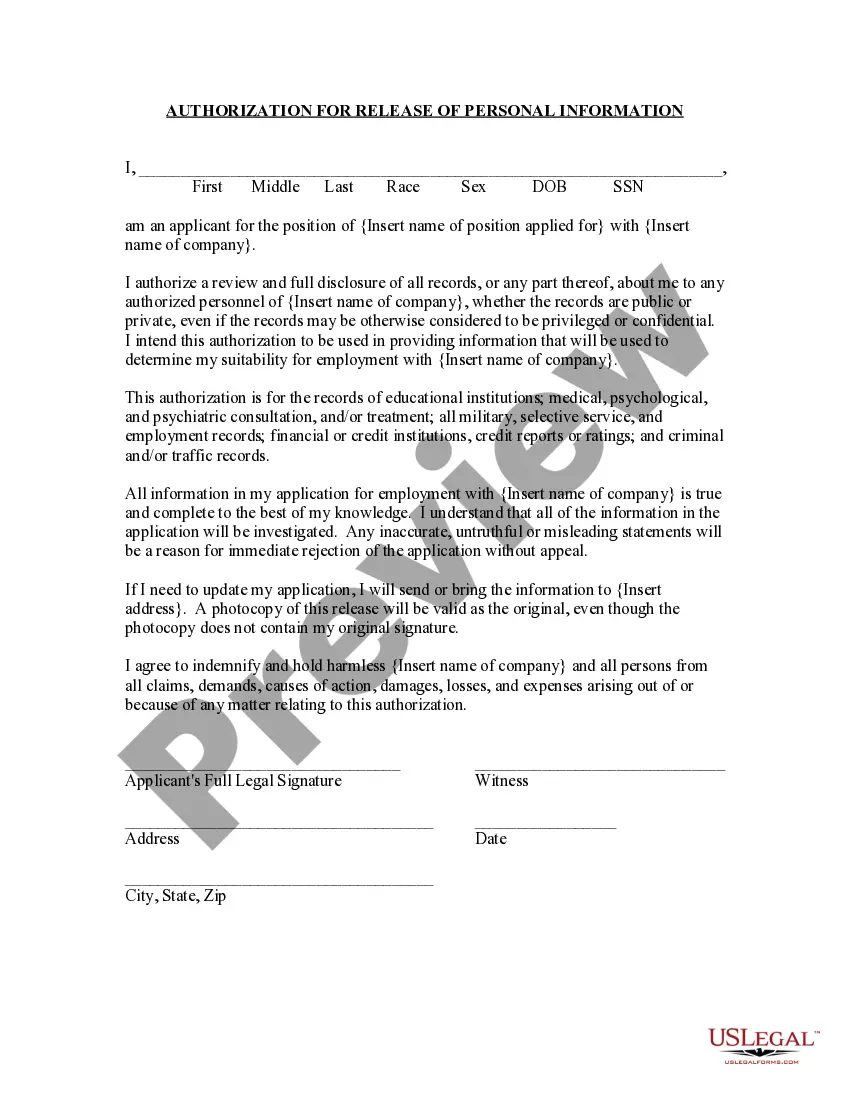
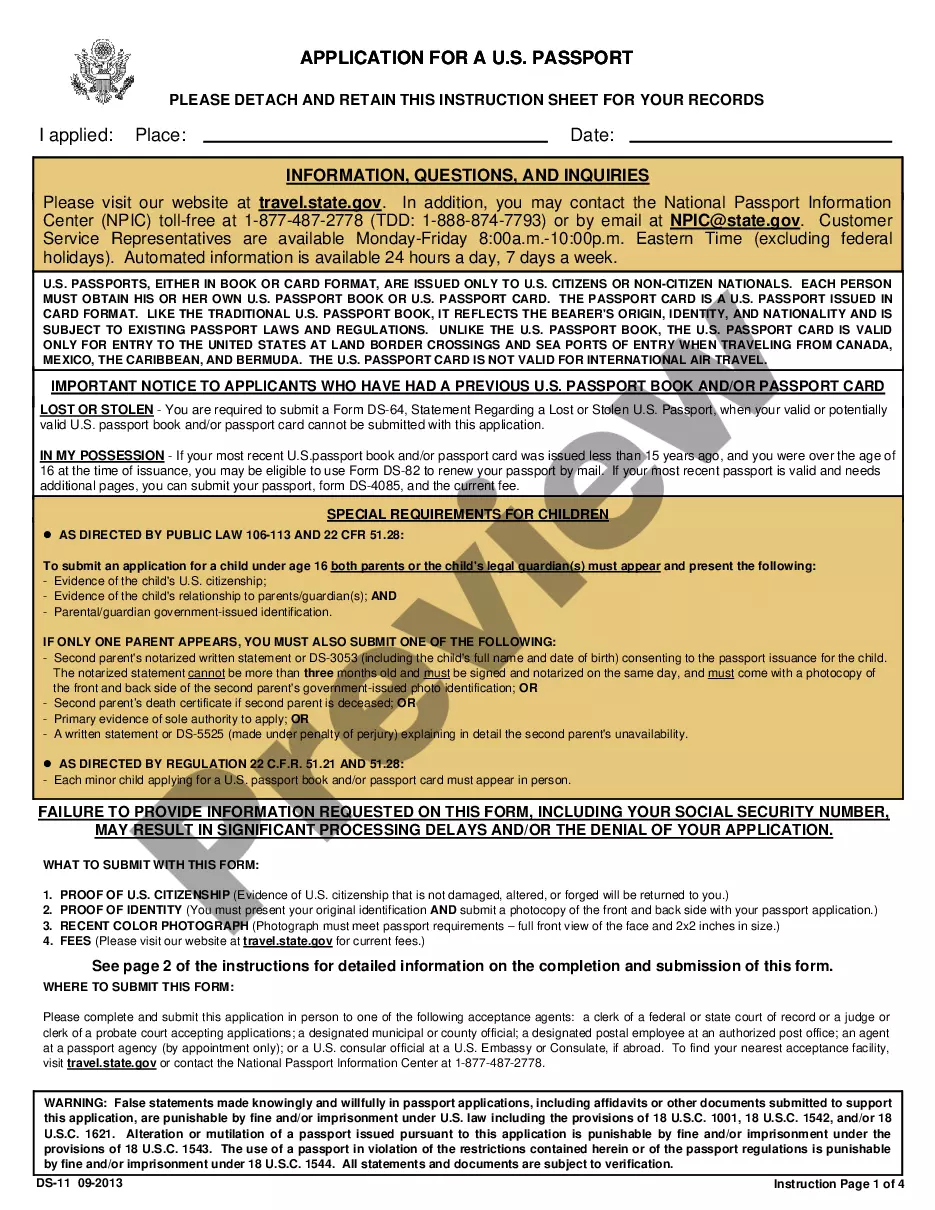
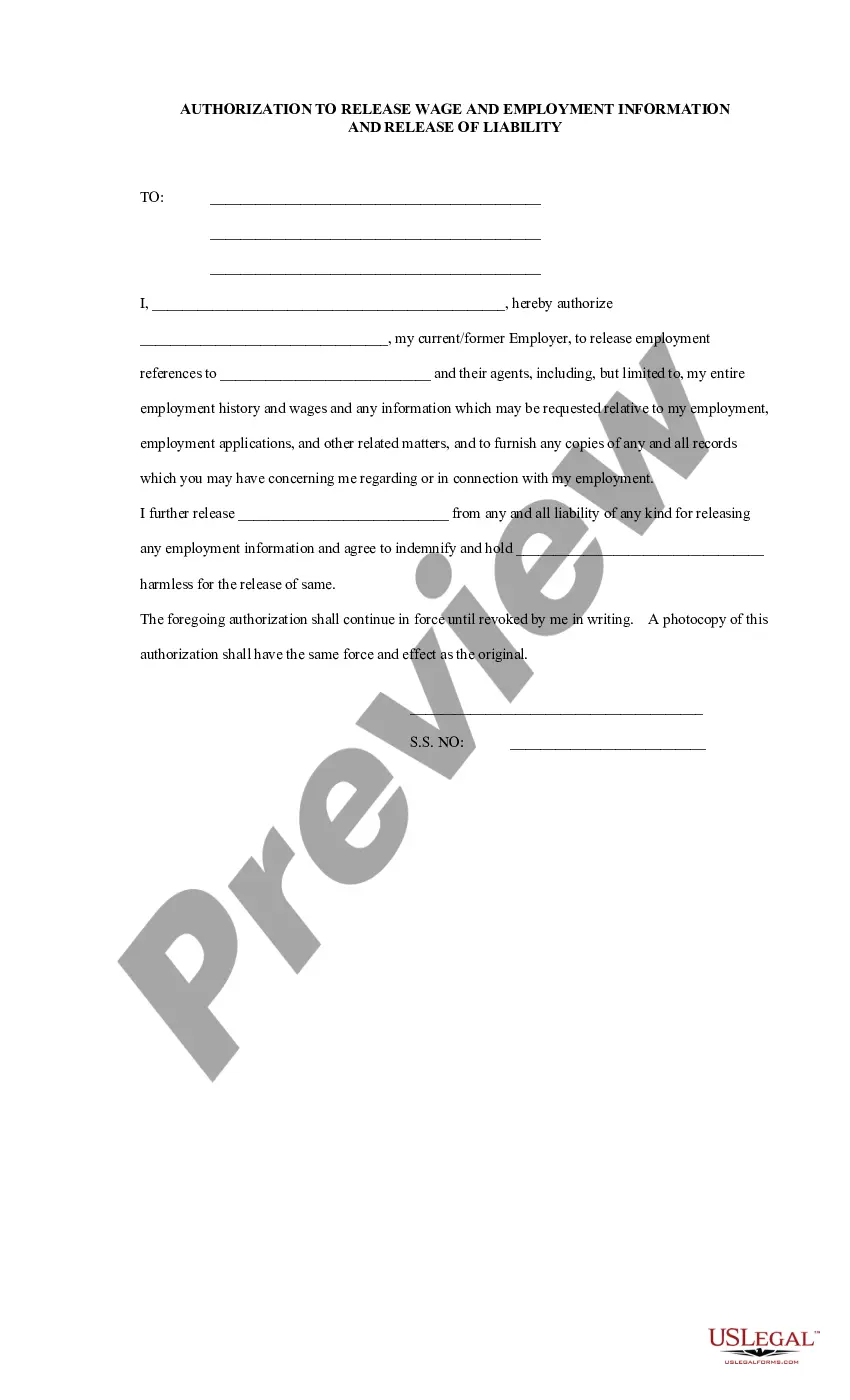
(a) Patients may authorize the release of their health care information by completing the CDCR 7385, Authorization for Release of Protected Health Information , to allow a family member or friend to request and receive an update when there is a significant change in the patient 's health care condition.
(a) Patients may authorize the release of their health care information by completing the CDCR 7385, Authorization for Release of Protected Health Information, to allow a family member or friend to request and receive an update when there is a significant change in the patient's health care condition.
All health records of discharged patients shall be completed and filed within 30 days after discharge date and such records shall be kept for a minimum of 7 years, except for minors whose records shall be kept at least until 1 year after the minor has reached the age of 18 years, but in no case less than 7 years.
The patient may enter the date he/she wants the authorization to expire. The patient may enter an expiration event. The patient may enter a date range of information to be shared. If no expiration date is specified, this authorization is good for 12 months from the date signed in Section IX.
All health records of discharged patients shall be completed and filed within 30 days after discharge date and such records shall be kept for a minimum of 7 years, except for minors whose records shall be kept at least until 1 year after the minor has reached the age of 18 years, but in no case less than 7 years.
Applicability. CCPA: Applies to businesses that collect personal information from California residents, even if they have no physical presence in California. HIPAA: Applies only to entities directly involved in healthcare, focusing on PHI, and primarily applies to the healthcare industry.
Federal laws govern the privacy protection of medical records, along with some state laws. California medical records laws state that a patient's information may not be disclosed without authorization unless it is pursuant to a court order, or for purposes of communicating important medical data to other health care ...
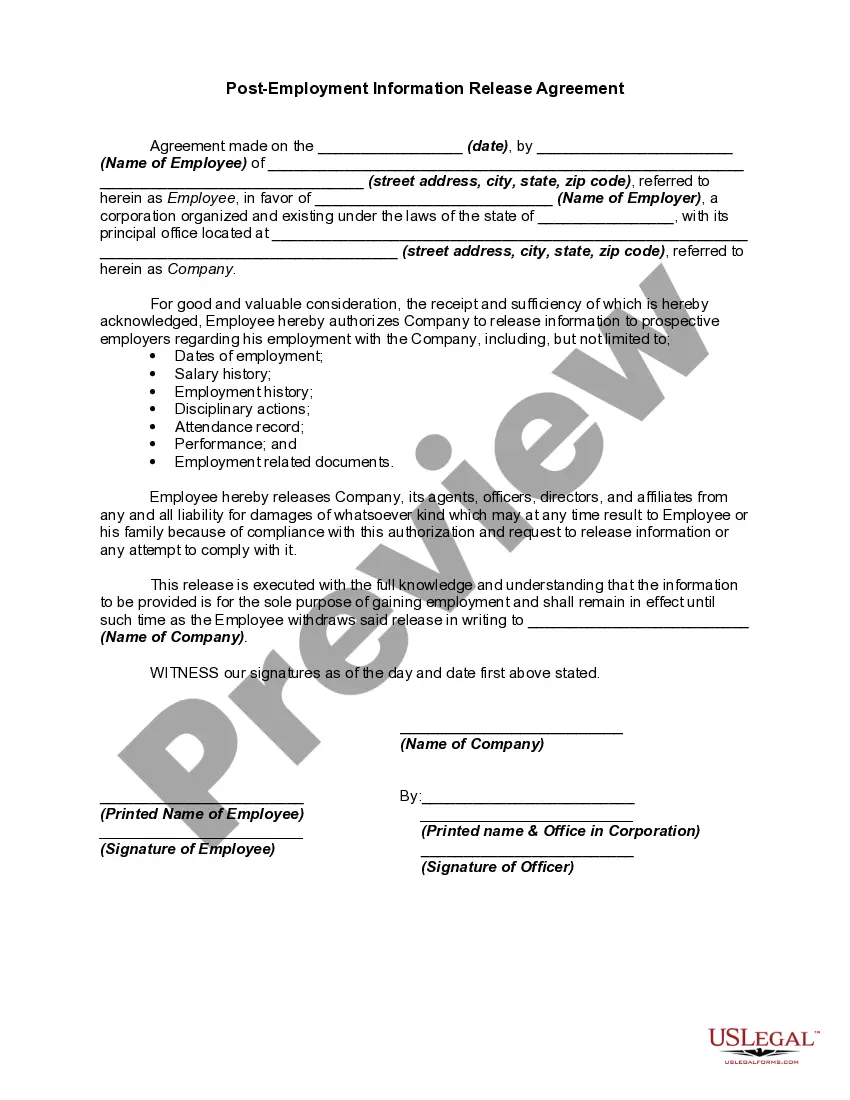
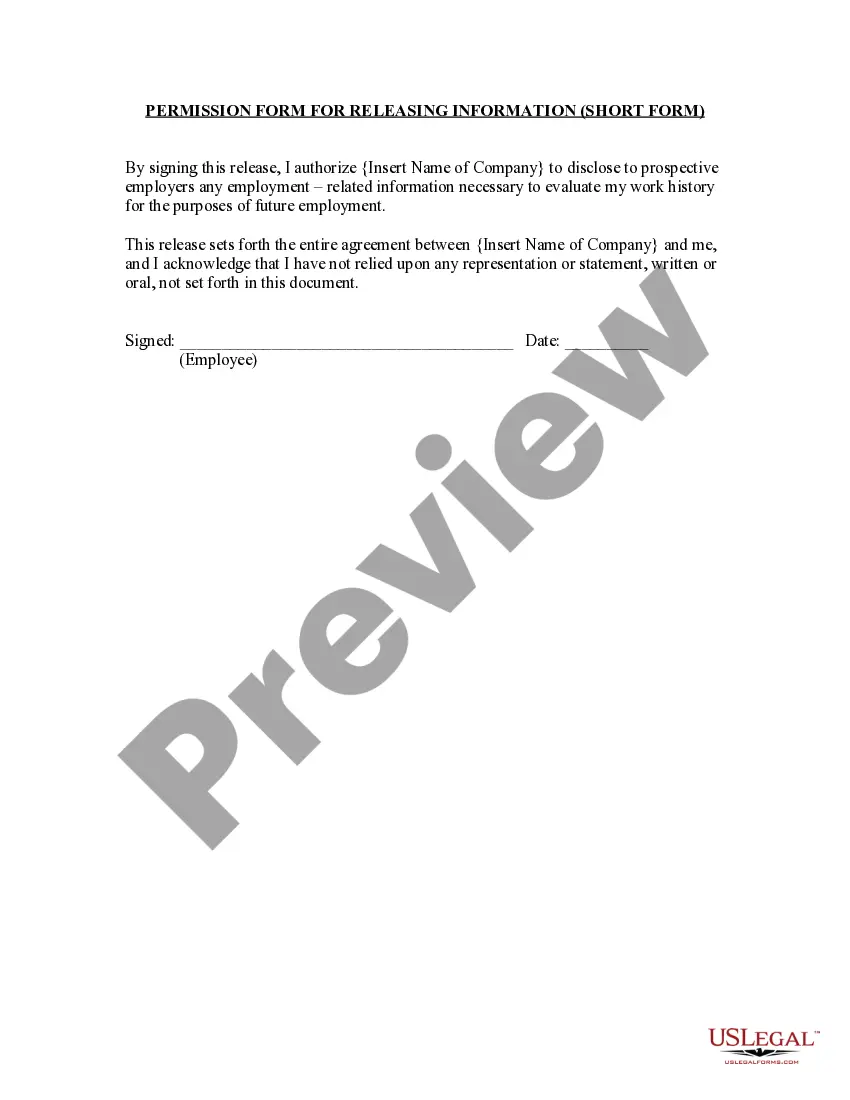
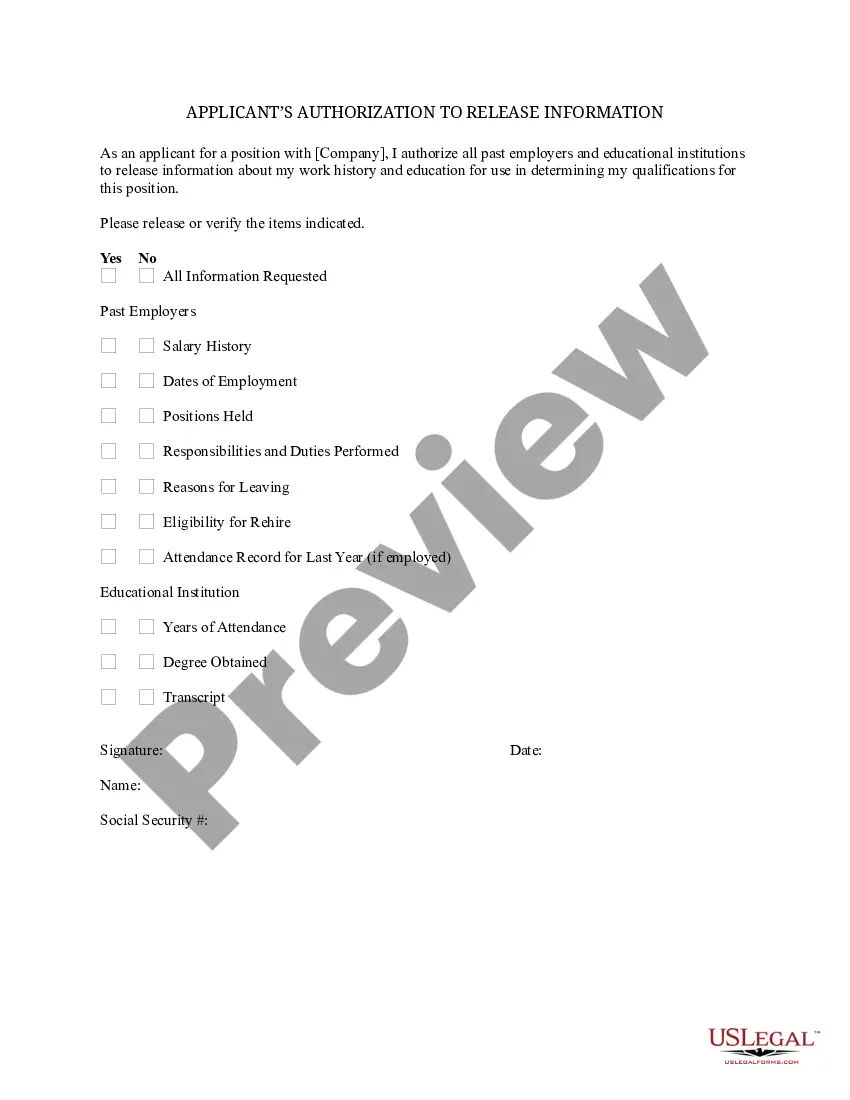
Generally, health care providers cannot disclose information protected by HIPAA and without a signed authorization. An authorization form must include specific elements to be valid under HIPAA and CMIA. (See Requirements for Release of Information Forms in Additional Resources.)
By law, a patient's records are defined as records relating to the health history, diagnosis, or condition of a patient, or relating to treatment provided or proposed to be provided to the patient. Physicians must provide patients with copies within 15 days of receipt of the request.
However, within the remaining 11 states including California and Washington—also known as “all-party jurisdiction states”—state law dictates that all parties recorded must express their consent.