Denied Claim Agreement For Authorization In Travis
Description
Form popularity
FAQ
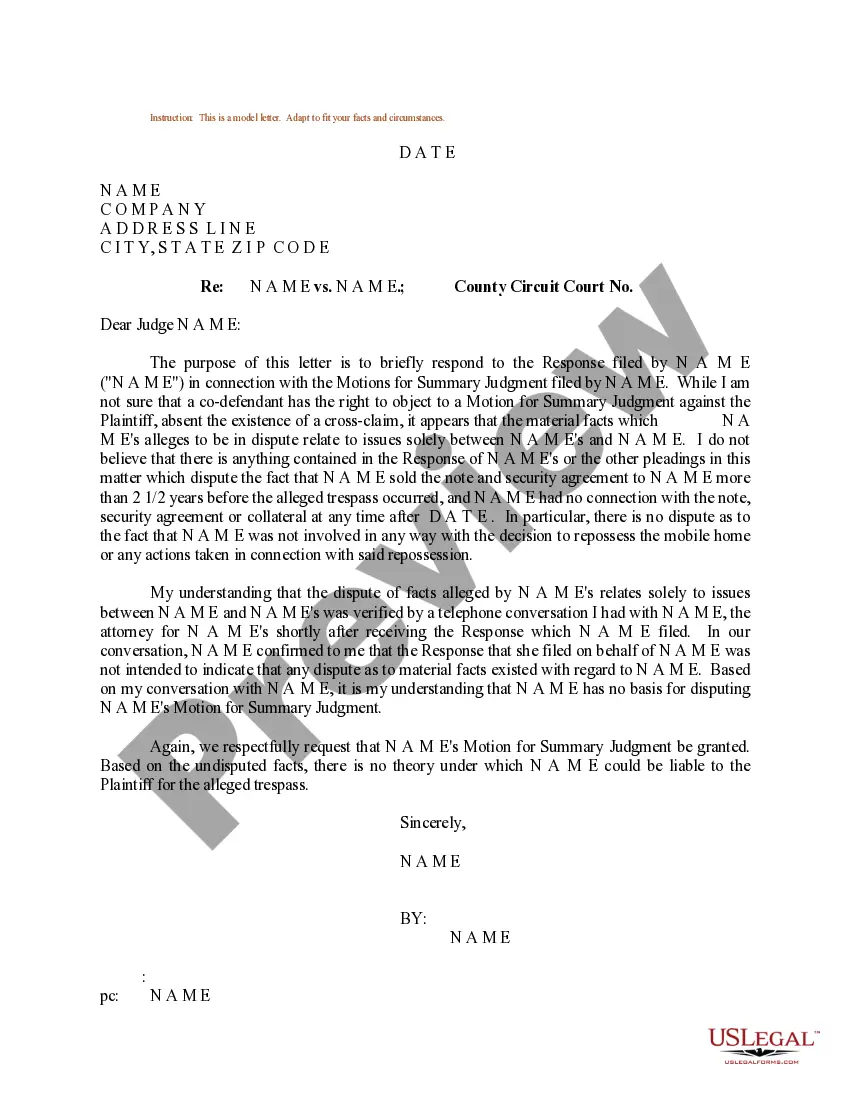
Be persistent Your appeal should include an explanation of your reconsideration request, along with any necessary supporting documentation, such as a copy of the claim in question and copies of earlier communication to the company about the matter.
Ans: You can file a complaint with the IRDAI's Grievance Cell of Consumer Affairs via phone or email to complaints@irdai.in if you do not agree with the rejection of your health insurance claim. You can also file a complaint on the Integrated Grievance Management System (IGMS) online on their website.
Try contacting the person who approved the procedure and explain that the claims department is refusing to cover despite the approval. Better yet, do a conference call between the medical director and a claims representative. That should hopefully solve any miscommunication.
I am writing to file an appeal regarding insurance company name's denial of a pre-authorization for medication name. I received a denial letter dated provide date stating provide denial reason directly from letter. As you are aware, I was diagnosed with migraine/chronic migraine on date.
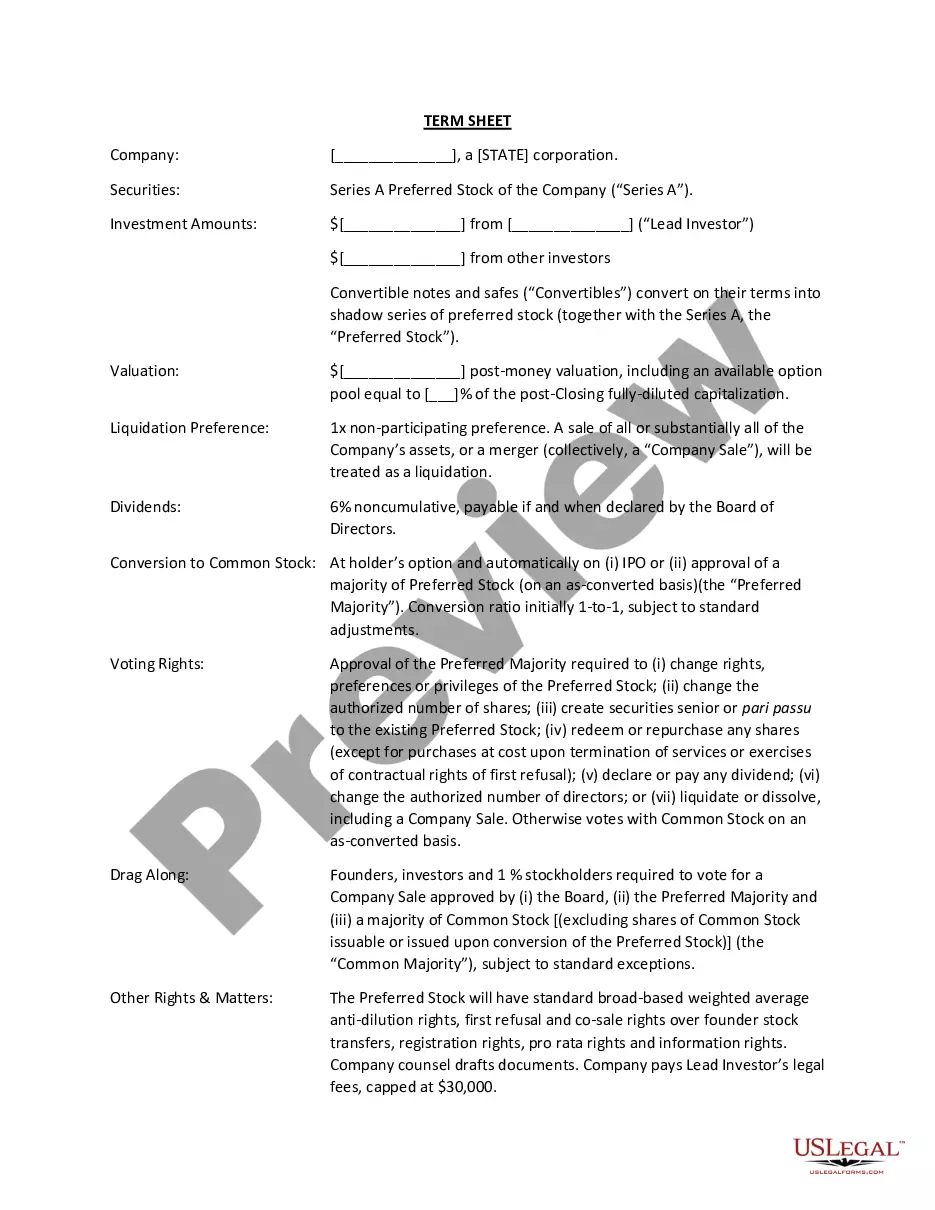
Thorough documentation based on a respected clinical source is the best way to obtain preauthorization or appeal a denial. In addition to government sources such as AHRQ, it may be worth asking your most frequent payers what guidelines they use. Clearly document any deviation from evidence-based guidelines.
You can start the appeal process by calling your insurance provider. Ask for more details about the denial and review your appeal options. Your insurance agent can walk you through the appeals process to help get you started.
You may be able to appeal to your insurance company multiple times based on the evidence you provide. If the outcome is not satisfactory, you can consider contacting a public adjuster to advocate on your behalf or file a complaint with your state's insurance department to act as an intermediary for the dispute.
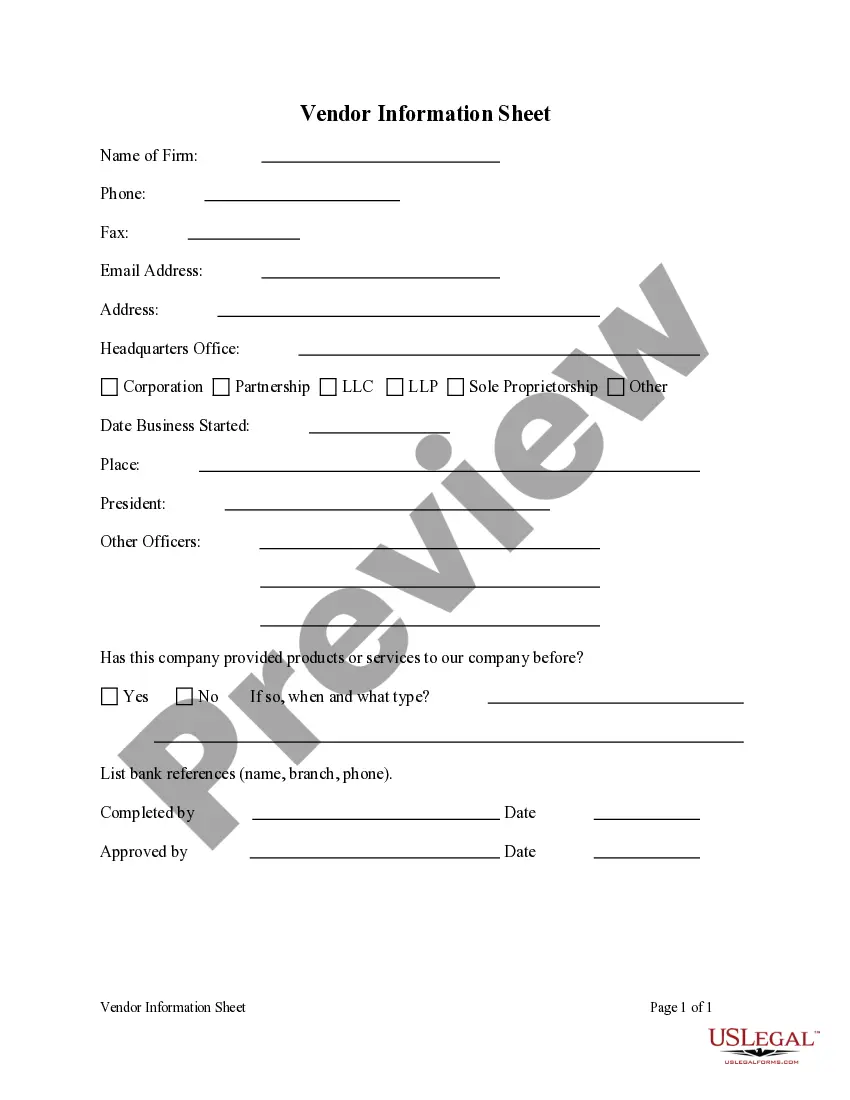
Some basic pointers for handling claims denials are outlined below. Carefully review all notifications regarding the claim. Be persistent. Don't delay. Get to know the appeals process. Maintain records on disputed claims. Remember that help is available.