Anthem Claim Dispute Form With Provider
Description
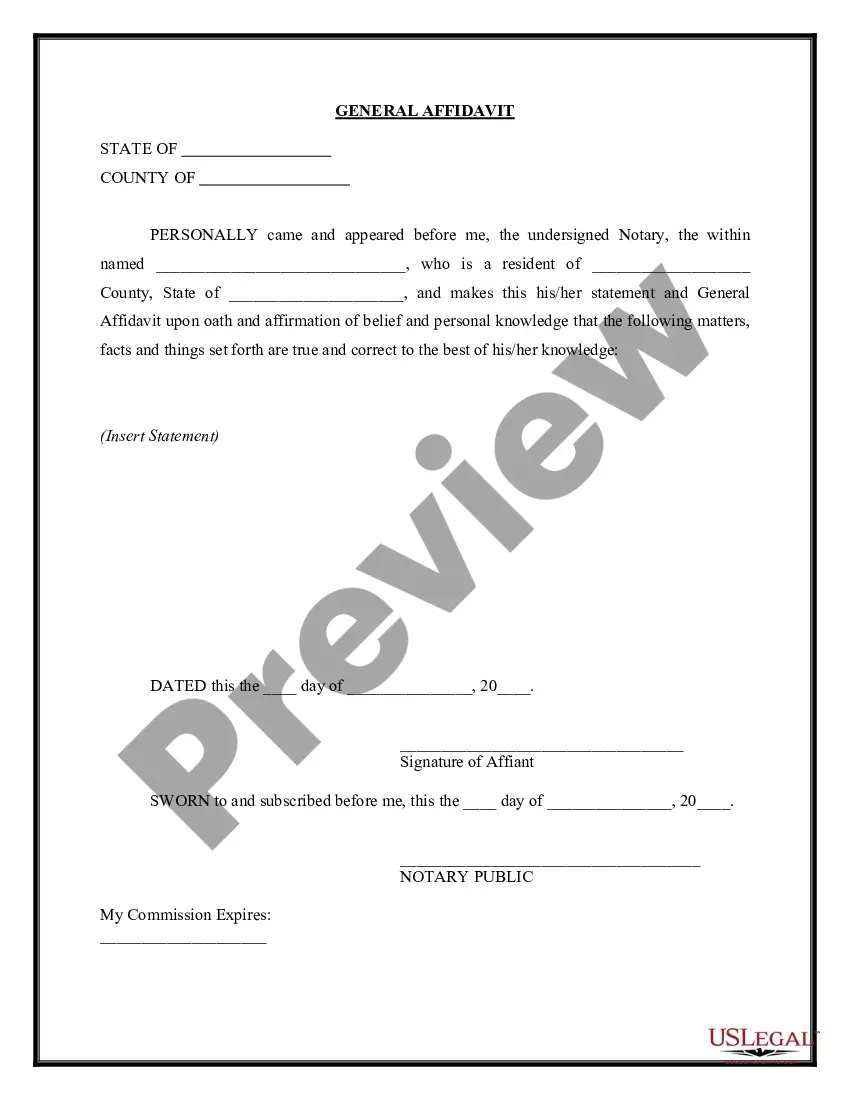
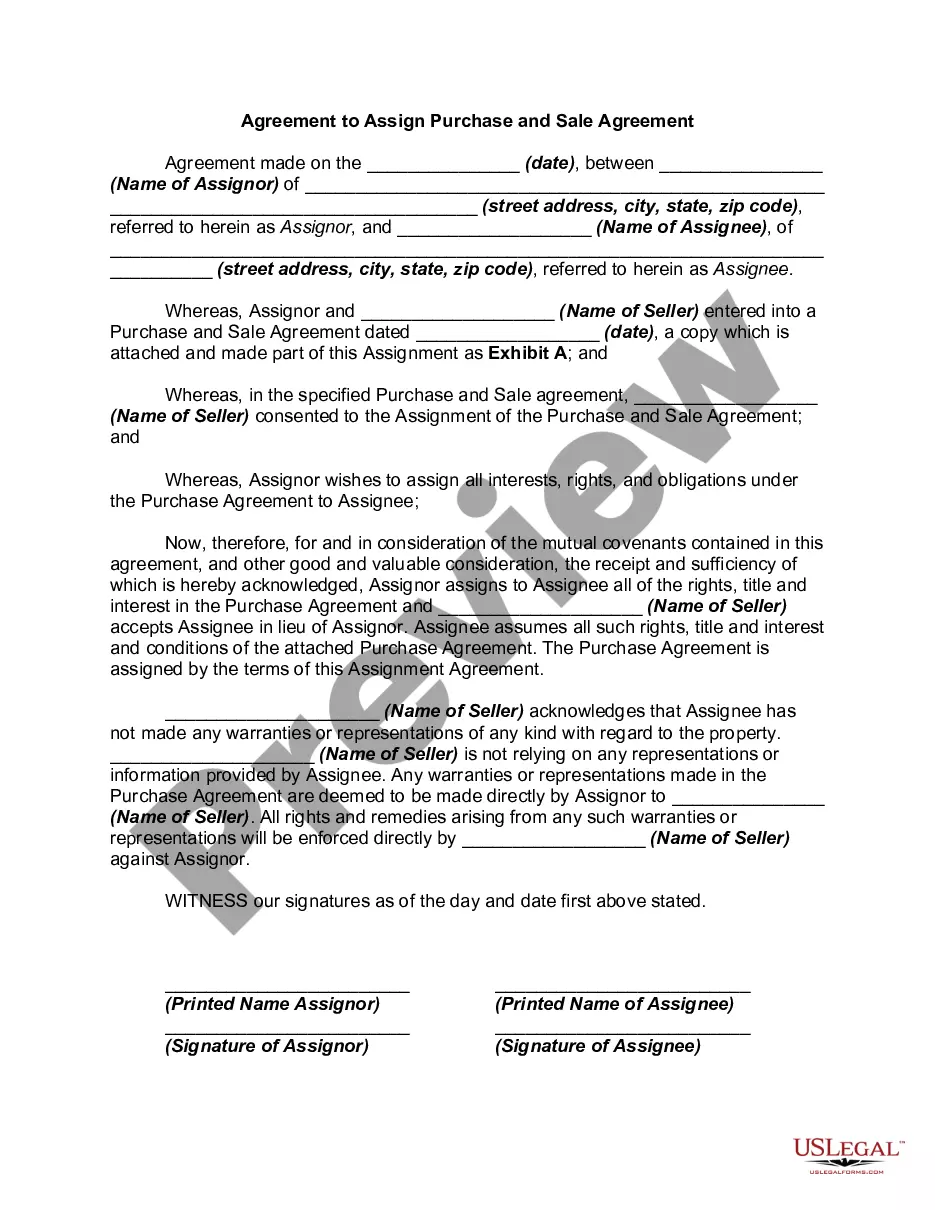
How to fill out Agreement For Accord And Satisfaction Of A Disputed Claim?
Whether for business purposes or for individual matters, everybody has to deal with legal situations at some point in their life. Completing legal papers demands careful attention, starting with choosing the correct form sample. For instance, when you choose a wrong edition of a Anthem Claim Dispute Form With Provider, it will be turned down once you send it. It is therefore important to have a dependable source of legal files like US Legal Forms.
If you have to obtain a Anthem Claim Dispute Form With Provider sample, follow these easy steps:
- Find the template you need by utilizing the search field or catalog navigation.
- Look through the form’s information to ensure it matches your situation, state, and region.
- Click on the form’s preview to view it.
- If it is the wrong form, get back to the search function to find the Anthem Claim Dispute Form With Provider sample you require.
- Download the file when it matches your requirements.
- If you already have a US Legal Forms profile, simply click Log in to access previously saved files in My Forms.
- In the event you do not have an account yet, you can obtain the form by clicking Buy now.
- Select the correct pricing option.
- Finish the profile registration form.
- Select your transaction method: use a credit card or PayPal account.
- Select the document format you want and download the Anthem Claim Dispute Form With Provider.
- After it is saved, you are able to complete the form with the help of editing software or print it and finish it manually.
With a substantial US Legal Forms catalog at hand, you never need to spend time searching for the appropriate template across the web. Take advantage of the library’s easy navigation to get the appropriate form for any situation.
Form popularity
FAQ
You or your provider can request an expedited appeal. Call Member Services toll-free at 844-912-0938 (TTY 711), Monday through Friday from 8 a.m. to 7 p.m. Eastern time.
Claims dispute From the Availity home page, select Claims & Payments from the top navigation. Select Claim Status Inquiry from the drop-down menu. Submit an inquiry and review the Claims Status Detail page. If the claim is denied or final, there will be an option to dispute the claim.
Common Reasons Anthem Gives for Insurance Denials Reasons for Anthem insurance claims denials include: The filing deadline has expired. The insured mad a late payment to COBRA. The medical device or treatment sought is not medically necessary.
Where can an appeal be filed? Mail your written appeal to: Anthem Blue Cross Cal MediConnect Plan. MMP Complaints, Appeals and Grievances. 4361 Irwin Simpson Road. ... Call Member Services at 1-855-817-5785 (TTY: 711) Monday through Friday from 8 a.m. to 8 p.m. This call is free. Fax your written appeal to 1-888-458-1406.
Please fax to 1-855-516-1083. You may ask us to rush your appeal if your health needs it. We'll let you know we got your appeal within 24 hours from the time we received it.