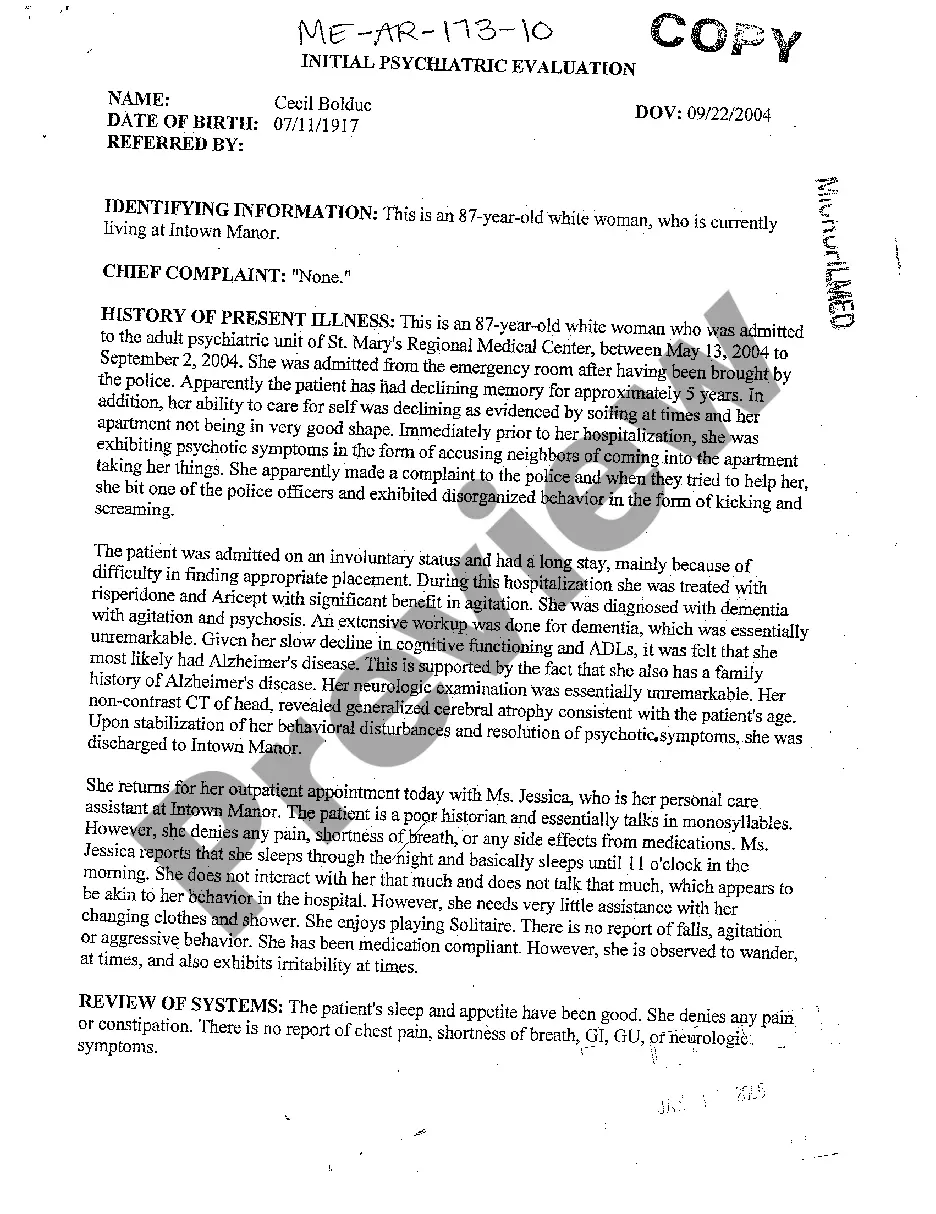
Initial Psychiatric Evaluation Template With Lines
Description
How to fill out Maine Initial Psychiatric Evaluation?
It’s no secret that you can’t become a legal professional immediately, nor can you learn how to quickly prepare Initial Psychiatric Evaluation Template With Lines without the need of a specialized background. Creating legal forms is a long venture requiring a certain training and skills. So why not leave the creation of the Initial Psychiatric Evaluation Template With Lines to the pros?
With US Legal Forms, one of the most extensive legal document libraries, you can access anything from court papers to templates for in-office communication. We understand how important compliance and adherence to federal and state laws are. That’s why, on our platform, all forms are location specific and up to date.
Here’s start off with our website and obtain the form you require in mere minutes:
- Find the form you need by using the search bar at the top of the page.
- Preview it (if this option provided) and read the supporting description to figure out whether Initial Psychiatric Evaluation Template With Lines is what you’re searching for.
- Start your search again if you need a different form.
- Register for a free account and select a subscription plan to buy the form.
- Choose Buy now. Once the payment is through, you can get the Initial Psychiatric Evaluation Template With Lines, fill it out, print it, and send or send it by post to the necessary people or organizations.
You can re-gain access to your documents from the My Forms tab at any time. If you’re an existing client, you can simply log in, and locate and download the template from the same tab.
Regardless of the purpose of your forms-be it financial and legal, or personal-our website has you covered. Try US Legal Forms now!
Form popularity
FAQ
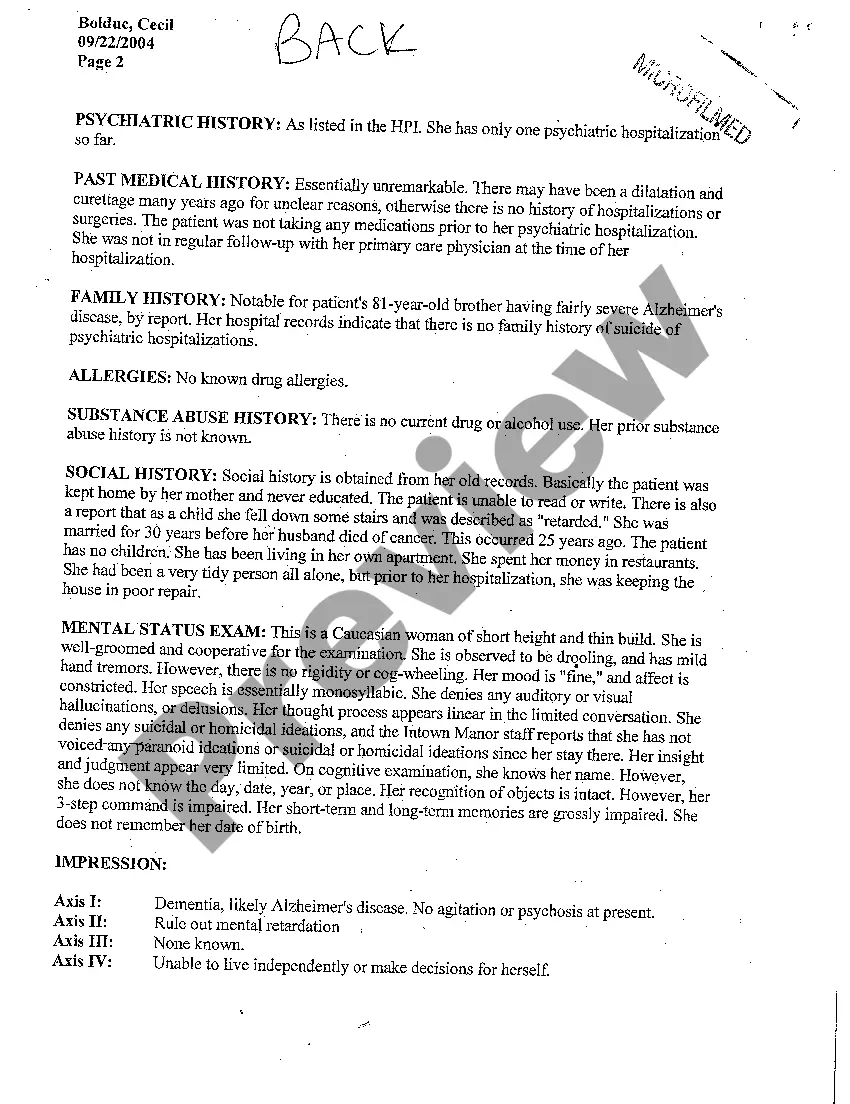
The summary should include: Demographic data like name, age, gender. Reasons for referral to psychiatry. History of present illness. History of previous illnesses. Family history. Personal history - birth and development, childhood, education, occupation, sexual and marital history. Premorbid personality. Physical examination.
History of Present Illness (HPI): In this section, you should outline details pertaining to the patient's psychiatric symptoms: their duration, severity, and any triggering or exacerbating factors. This section should, ideally, mirror the patient's functional and emotional impairments that brought them to you.
Elicit specific information, including a history of the presenting problems, pertinent medical information, family background, social history, and specific symptom and behavioral patterns. Formally test mental status (see that Chapter). Ask if the patient has any questions or unmentioned concerns.
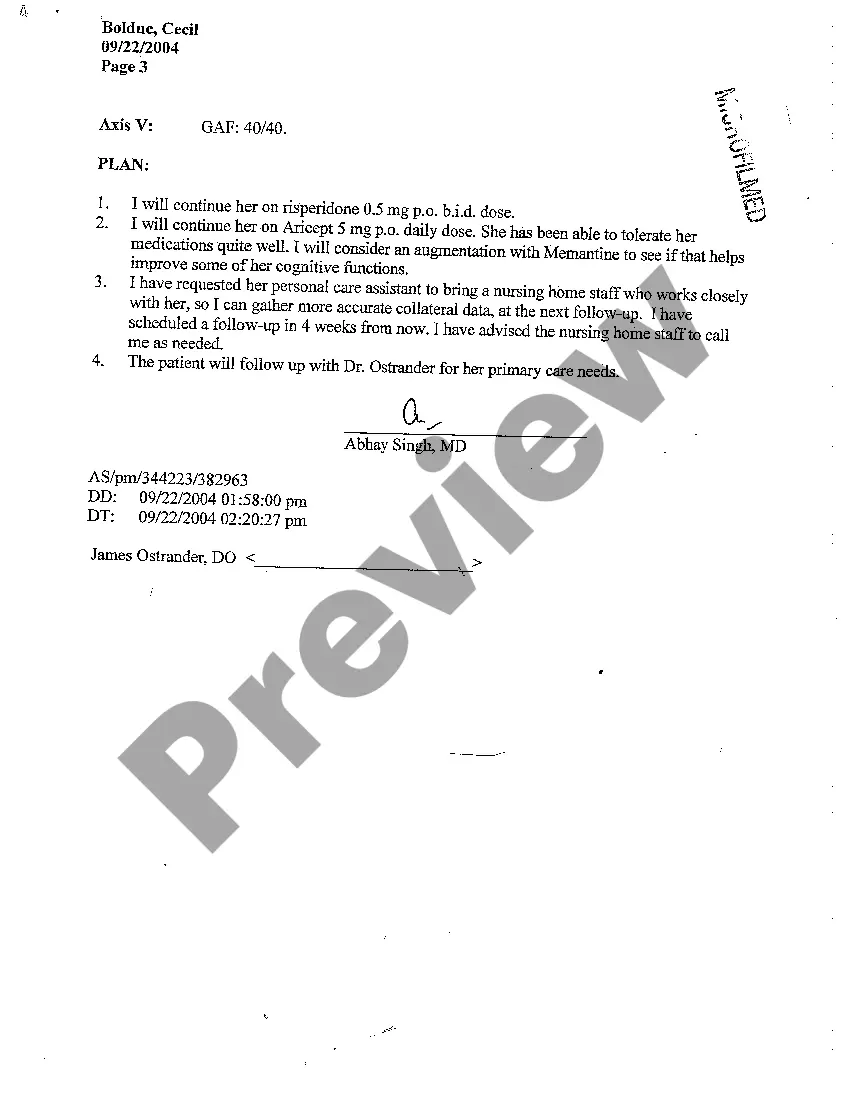
Components of a clinical encounter which should be documented include: Chief Complaint or Reason for Encounter. Referral Source. History of Present Illness. Current Treatments including medications and ongoing therapies. Mental Status Examination. Diagnoses. Treatment Plan including.
Here are 13 things you should never say to a therapist: Telling Lies & Half-Truths. ... Leaving Out Important Details. ... Testing Your Therapist. ... Apologizing for Feelings You Express in Therapy. ... ?I Didn't Do My Homework? ... Detailing Every Minute Detail of Your Day. ... Just Stating the Facts. ... Asking Them What You Should Do.