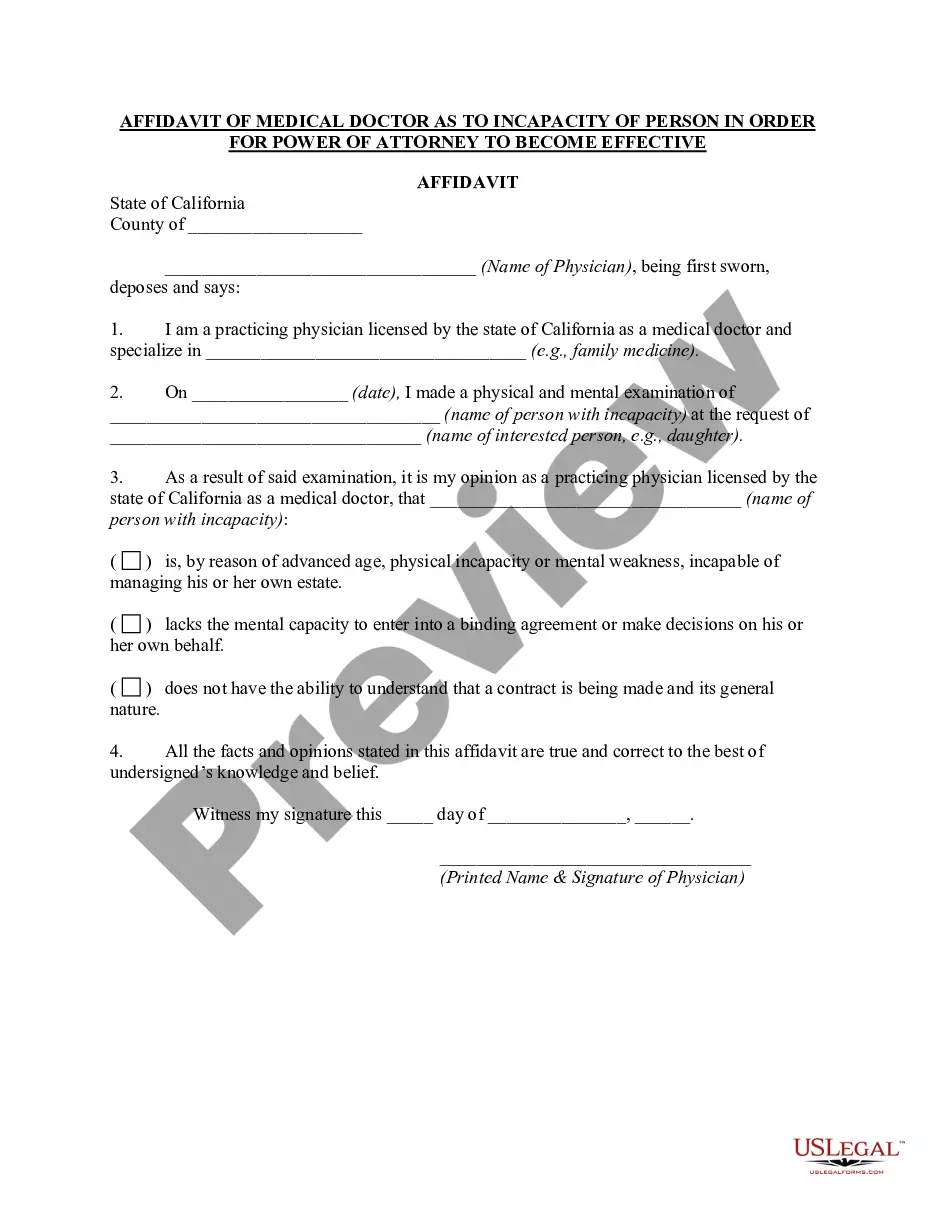
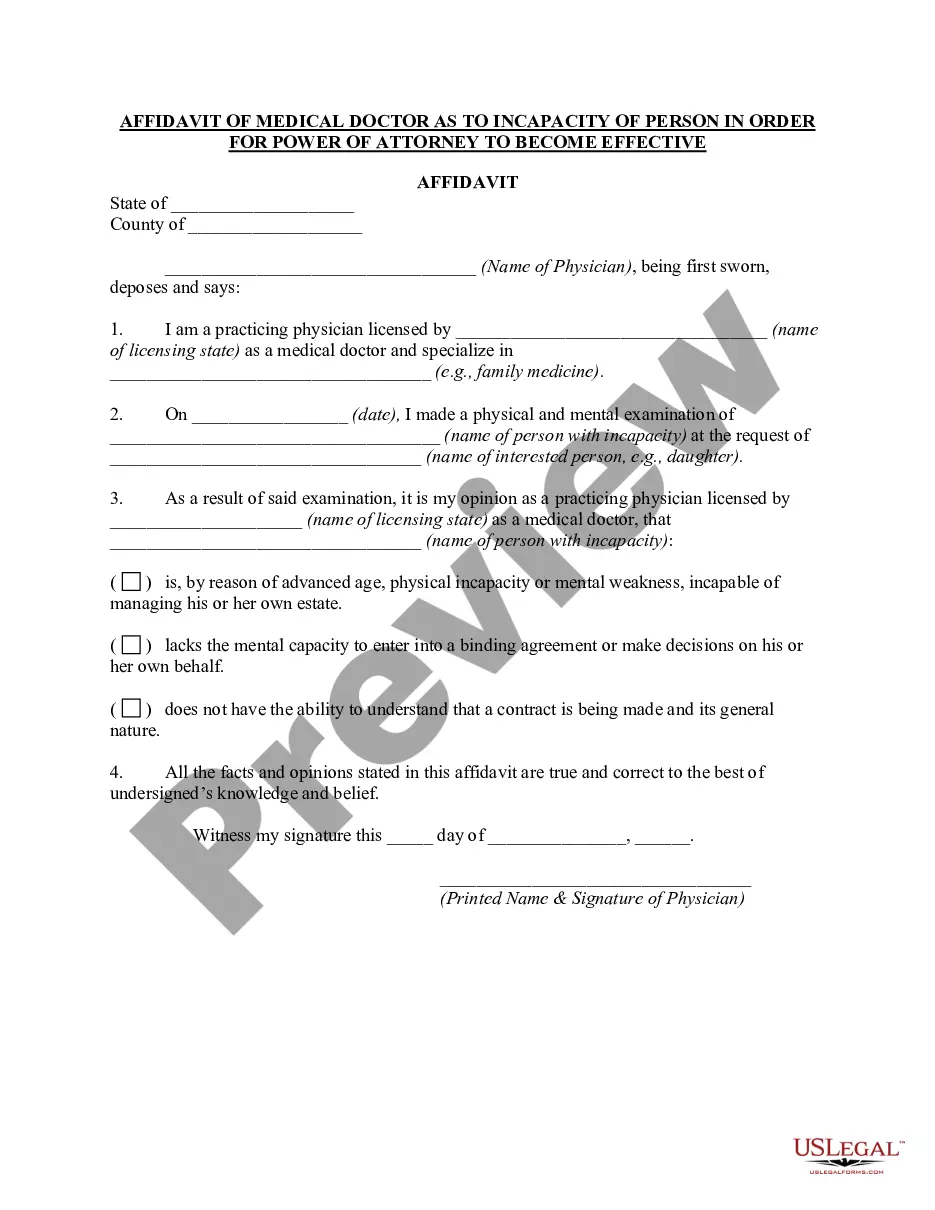
Incapacitated Doctors Note With Signature
Description
How to fill out California Affidavit Of Medical Doctor As To Incapacity Of Person In Order For Power Of Attorney To Become Effective?
Accessing legal document samples that meet the federal and regional regulations is a matter of necessity, and the internet offers many options to choose from. But what’s the point in wasting time looking for the right Incapacitated Doctors Note With Signature sample on the web if the US Legal Forms online library already has such templates collected in one place?
US Legal Forms is the largest online legal catalog with over 85,000 fillable templates drafted by lawyers for any business and life scenario. They are easy to browse with all documents grouped by state and purpose of use. Our specialists keep up with legislative changes, so you can always be sure your paperwork is up to date and compliant when getting a Incapacitated Doctors Note With Signature from our website.
Obtaining a Incapacitated Doctors Note With Signature is quick and easy for both current and new users. If you already have an account with a valid subscription, log in and download the document sample you need in the right format. If you are new to our website, adhere to the guidelines below:
- Take a look at the template utilizing the Preview option or through the text outline to make certain it fits your needs.
- Locate a different sample utilizing the search function at the top of the page if needed.
- Click Buy Now when you’ve found the suitable form and choose a subscription plan.
- Create an account or log in and make a payment with PayPal or a credit card.
- Pick the format for your Incapacitated Doctors Note With Signature and download it.
All documents you locate through US Legal Forms are reusable. To re-download and complete earlier purchased forms, open the My Forms tab in your profile. Benefit from the most extensive and easy-to-use legal paperwork service!
Form popularity
FAQ
Currently, sponsors who wish to have their incapacitated dependents remain eligible for benefits, are required to submit a complete financial dependency redetermination package (DD Form 137-5) every 4 years, to their uniformed service's DEERS/RAPIDS Project Office and or the supporting finance office.
The Medical Practitioner makes a declaration about the ability of the child to maintain himself or herself over 18 on the Form ICC2. This declaration must state that there is a reasonable expectation the degree of incapacity prevents the child from maintaining himself or herself over 18.
PRINCIPAL PURPOSE(S): The information provided on this form will be used to determine the relationship and dependency of an individual on the military member, for entitlement of authorized benefits.
A Dependency Determination is a document used to prove a Sponsor (military service member) is not only responsible for but does, in actuality, provide more than 50% of the support, or living expenses, of the dependent in question.
The DD Form 137-4, ?Dependency Statement ? Child Born Out of Wedlock Under Age 21,? is submitted to claim a child born out of wedlock for a USIP card.