Arkansas COBRA Continuation Coverage Election Notice
Description
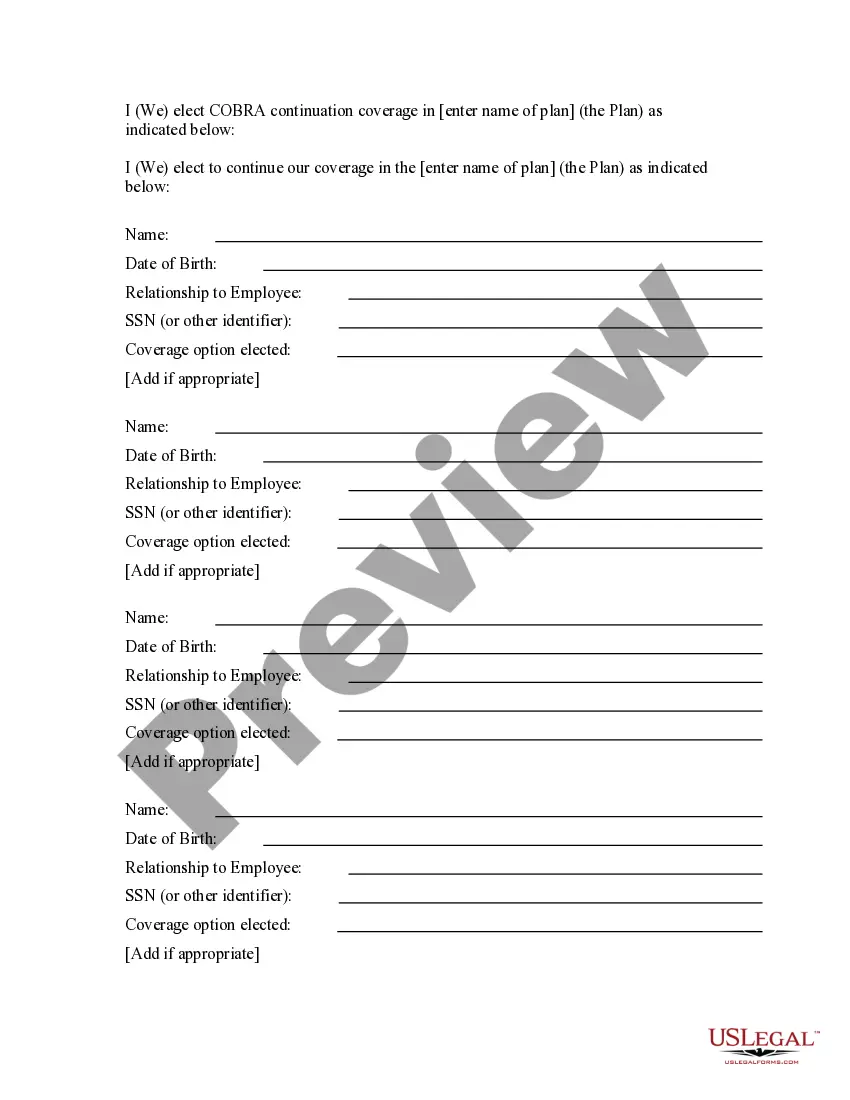
How to fill out COBRA Continuation Coverage Election Notice?
Are you in the placement that you require files for either business or specific functions virtually every working day? There are a variety of legal record layouts available online, but discovering types you can rely on is not effortless. US Legal Forms provides 1000s of kind layouts, much like the Arkansas COBRA Continuation Coverage Election Notice, that happen to be written to fulfill federal and state needs.
When you are already knowledgeable about US Legal Forms website and also have a free account, just log in. Next, you can download the Arkansas COBRA Continuation Coverage Election Notice web template.
If you do not come with an accounts and want to begin using US Legal Forms, abide by these steps:
- Discover the kind you want and make sure it is for your right area/state.
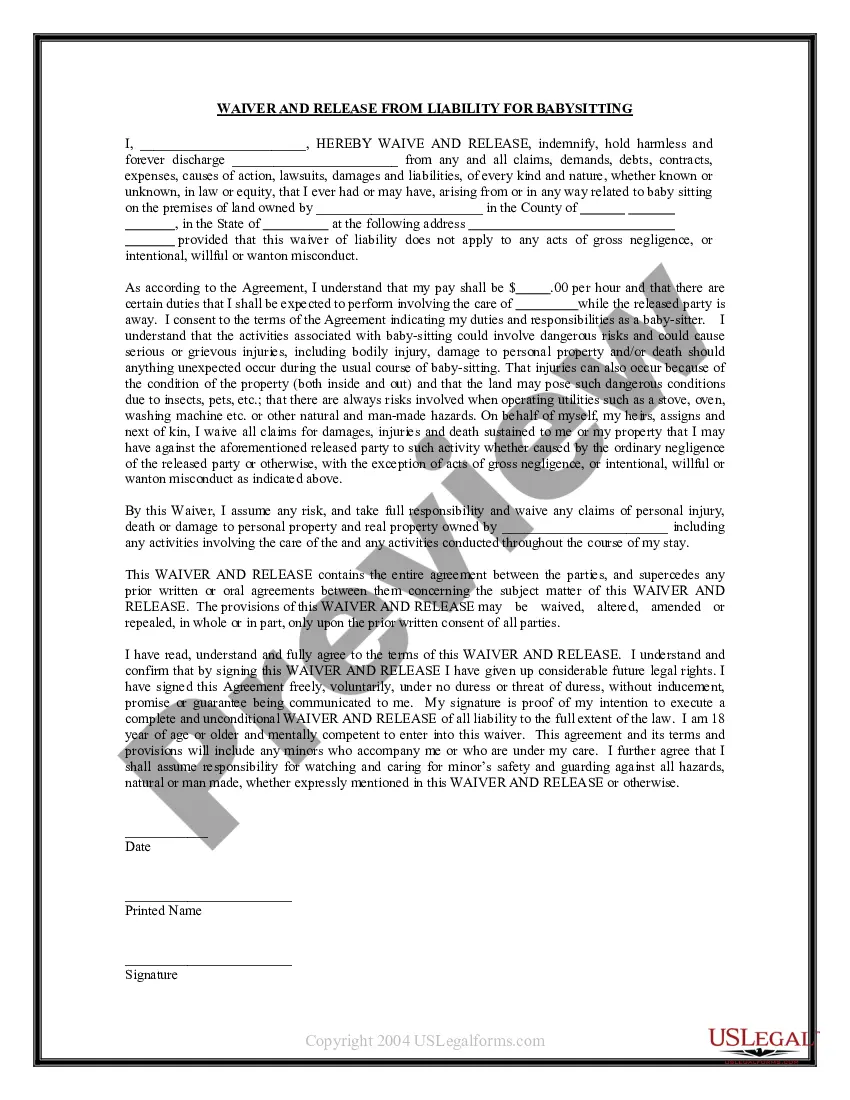
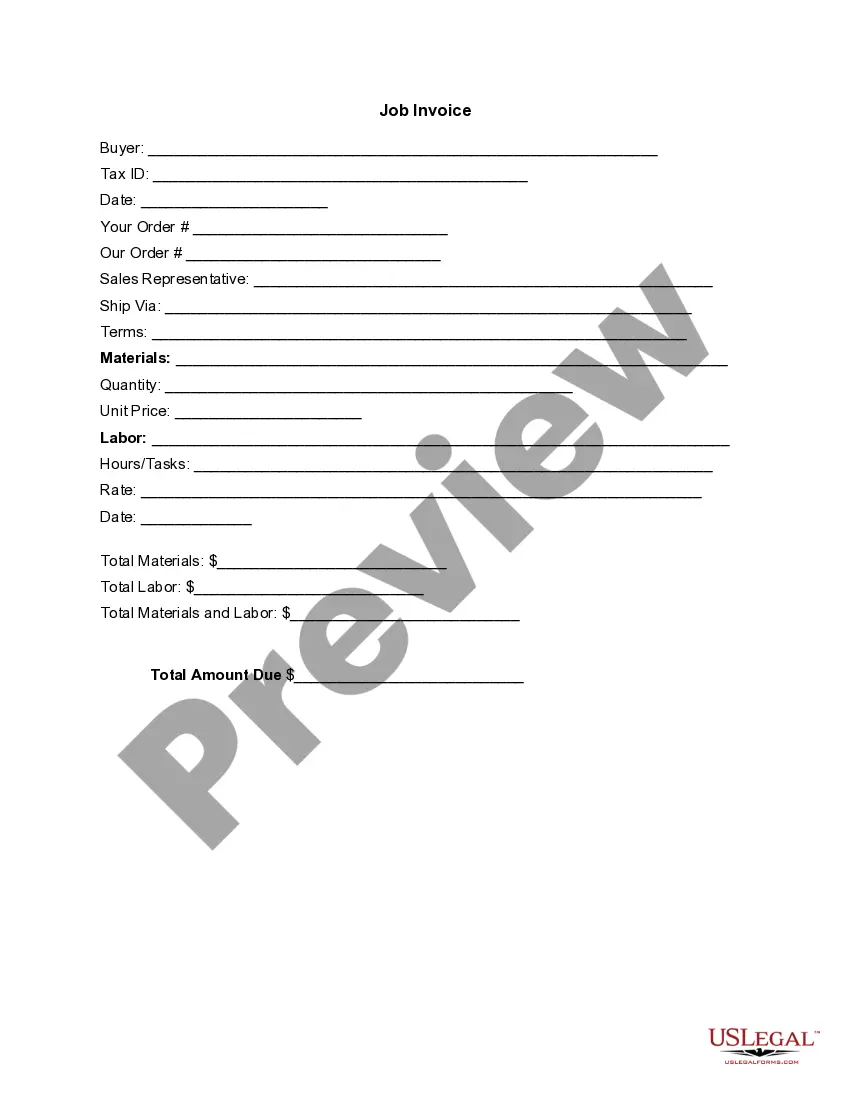
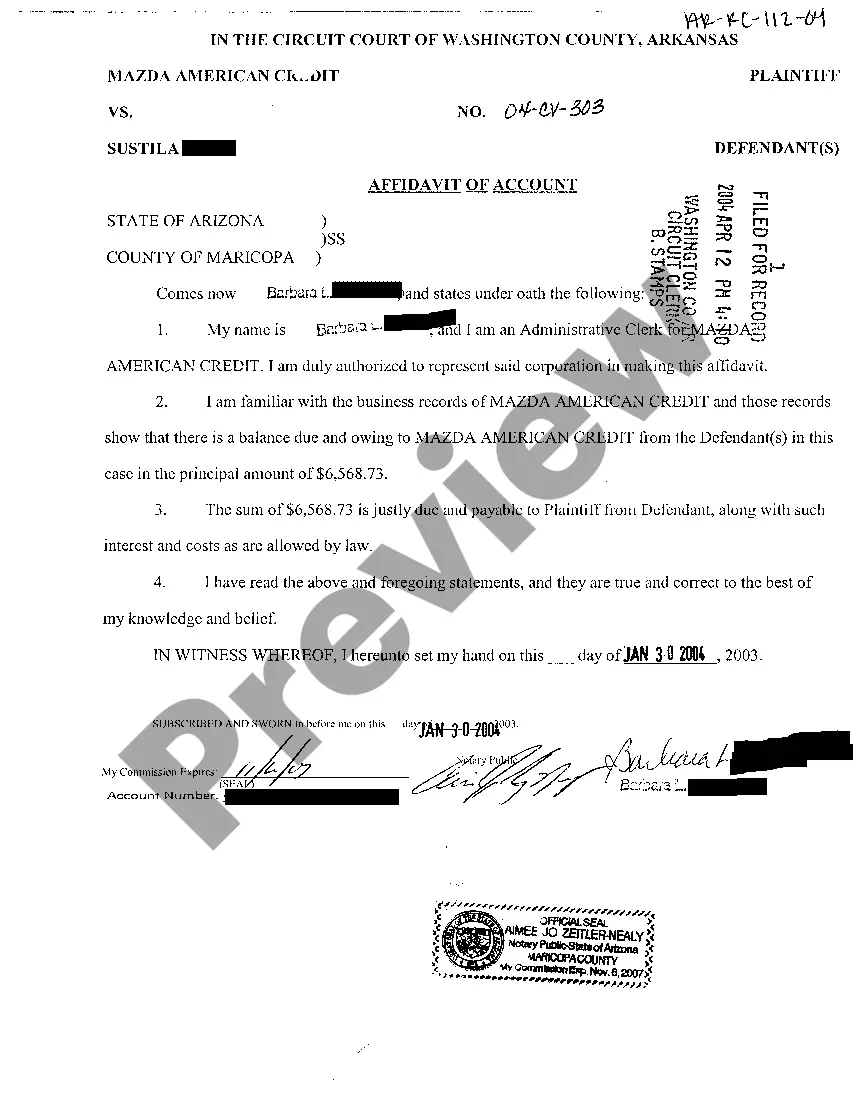
- Make use of the Review switch to review the shape.
- Look at the information to ensure that you have chosen the appropriate kind.
- In case the kind is not what you`re looking for, utilize the Lookup industry to find the kind that meets your requirements and needs.
- When you obtain the right kind, click Acquire now.
- Opt for the rates plan you need, fill out the required details to create your money, and pay money for an order making use of your PayPal or Visa or Mastercard.
- Pick a handy file file format and download your duplicate.
Find all the record layouts you possess purchased in the My Forms food list. You can obtain a extra duplicate of Arkansas COBRA Continuation Coverage Election Notice anytime, if necessary. Just click the required kind to download or printing the record web template.
Use US Legal Forms, one of the most extensive assortment of legal types, to conserve time as well as steer clear of faults. The support provides expertly manufactured legal record layouts which you can use for a range of functions. Generate a free account on US Legal Forms and initiate making your life a little easier.
Form popularity
FAQ
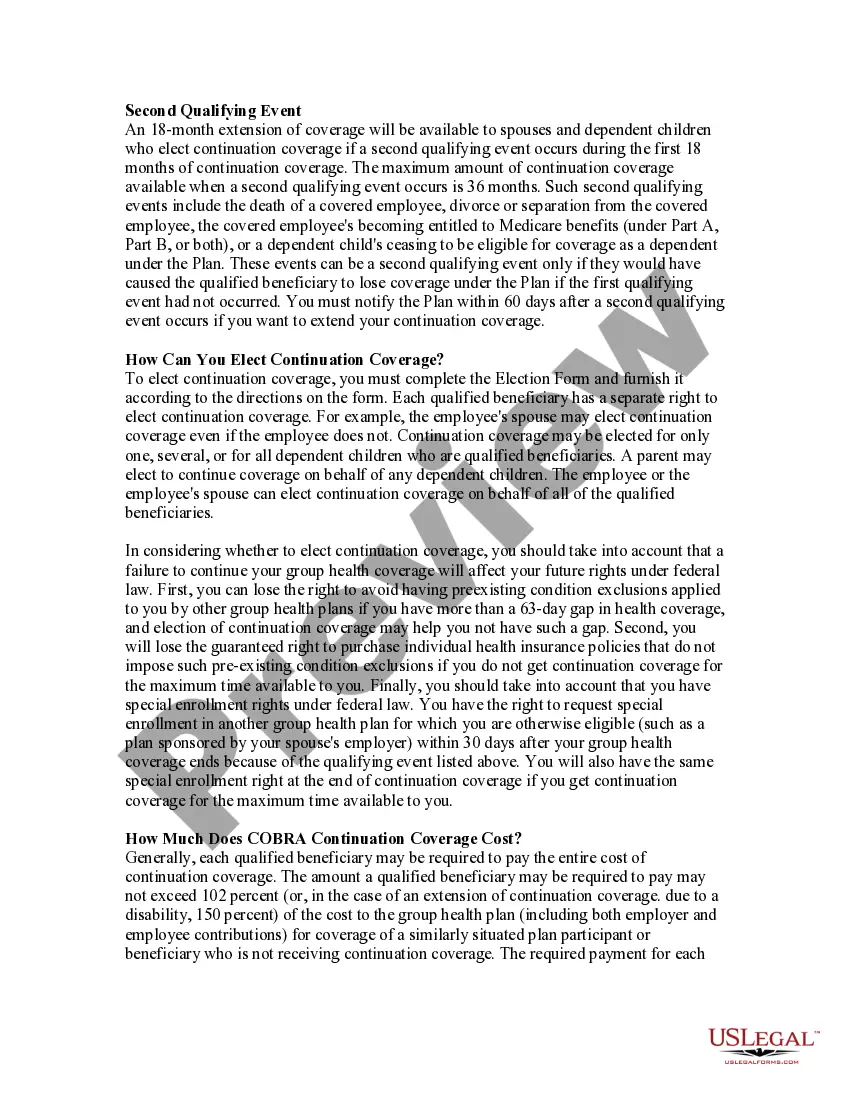
Arkansas has a mini-COBRA law that extends COBRA insurance plans for employees at companies with less than 20 employees. This means workers in Arkansas have a right to continue their workplace insurance, even if they quit their jobs or were involuntarily terminated (getting fired).
COBRA is always effective the day after your active coverage ends. For most, active coverage terminates at the end of a month and COBRA is effective on the first day of the next month.
COBRA is a federal law about health insurance. If you lose or leave your job, COBRA lets you keep your existing employer-based coverage for at least the next 18 months. Your existing healthcare plan will now cost you more. Under COBRA, you pay the whole premium including the share your former employer used to pay.
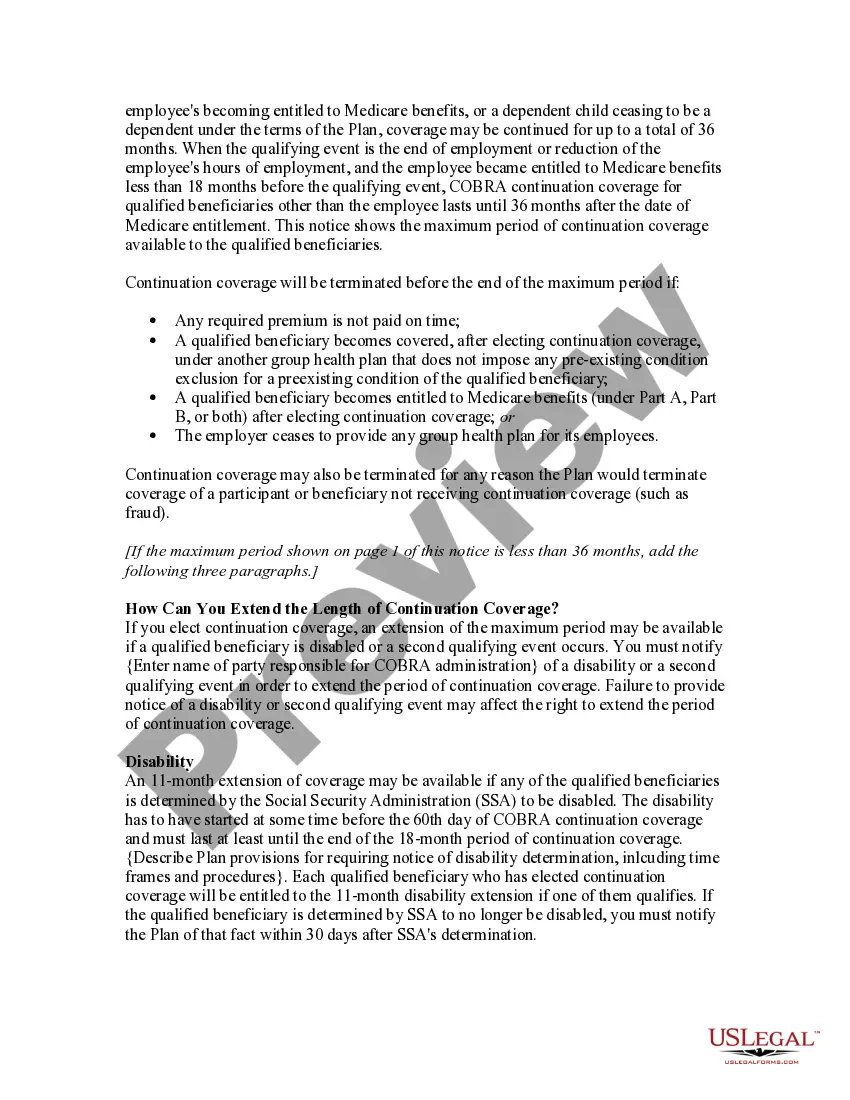
The following are qualifying events: the death of the covered employee; a covered employee's termination of employment or reduction of the hours of employment; the covered employee becoming entitled to Medicare; divorce or legal separation from the covered employee; or a dependent child ceasing to be a dependent under
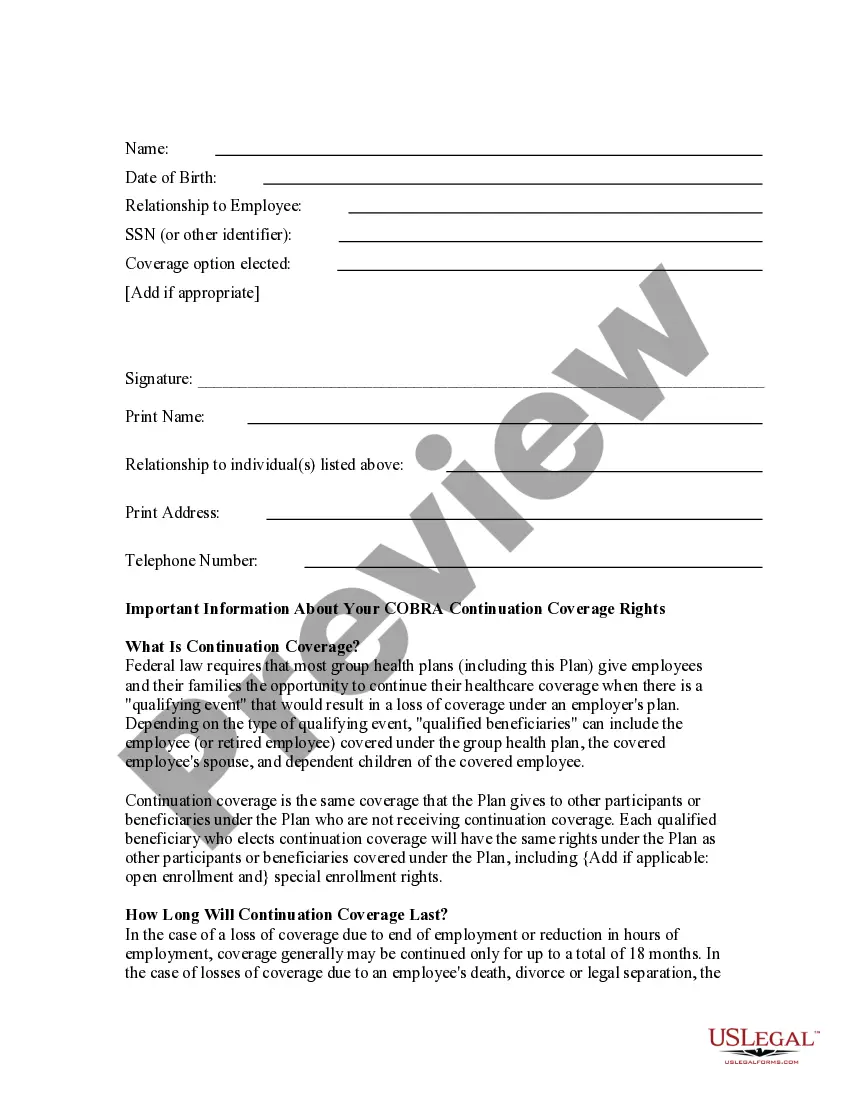
Federal law requires that most group health plans (including this Plan) give employees and their families the opportunity to continue their health care coverage through COBRA continuation coverage when there's a qualifying event that would result in a loss of coverage under an employer's plan.
COBRA the Consolidated Omnibus Budget Reconciliation Act -- requires group health plans to offer continuation coverage to covered employees, former employees, spouses, former spouses, and dependent children when group health coverage would otherwise be lost due to certain events.
Key Takeaways. COBRA provides a good option for keeping your employer-sponsored health plan for a while after you leave your job. Although, the cost can be high. Make an informed choice by looking at all your options during the 60-day enrollment period, and don't focus on the premium alone.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.
COBRA continuation rights are usually limited to either 18 or 36 months (with the exception of continued coverage under COBRA for a maximum period of: 1. 18 months if coverage would otherwise end due to: Termination, or 2022 Reduction of hours.