Certificate Plan Coverage For Dependents
Description
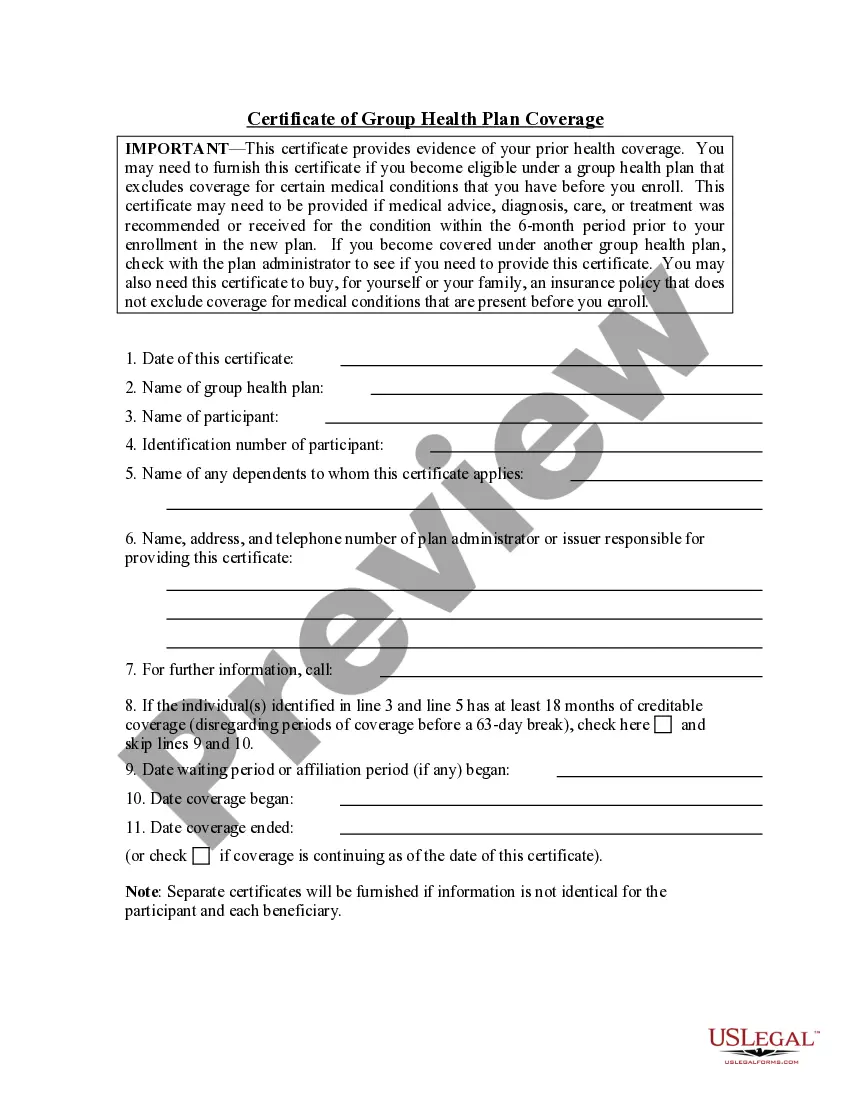
How to fill out Certificate Of Group Health Plan Coverage?
It’s no secret that you can’t become a legal expert overnight, nor can you learn how to quickly prepare Certificate Plan Coverage For Dependents without the need of a specialized set of skills. Creating legal forms is a long venture requiring a certain education and skills. So why not leave the creation of the Certificate Plan Coverage For Dependents to the pros?
With US Legal Forms, one of the most extensive legal template libraries, you can find anything from court paperwork to templates for in-office communication. We know how important compliance and adherence to federal and local laws and regulations are. That’s why, on our platform, all templates are location specific and up to date.
Here’s start off with our platform and obtain the form you need in mere minutes:
- Discover the document you need by using the search bar at the top of the page.
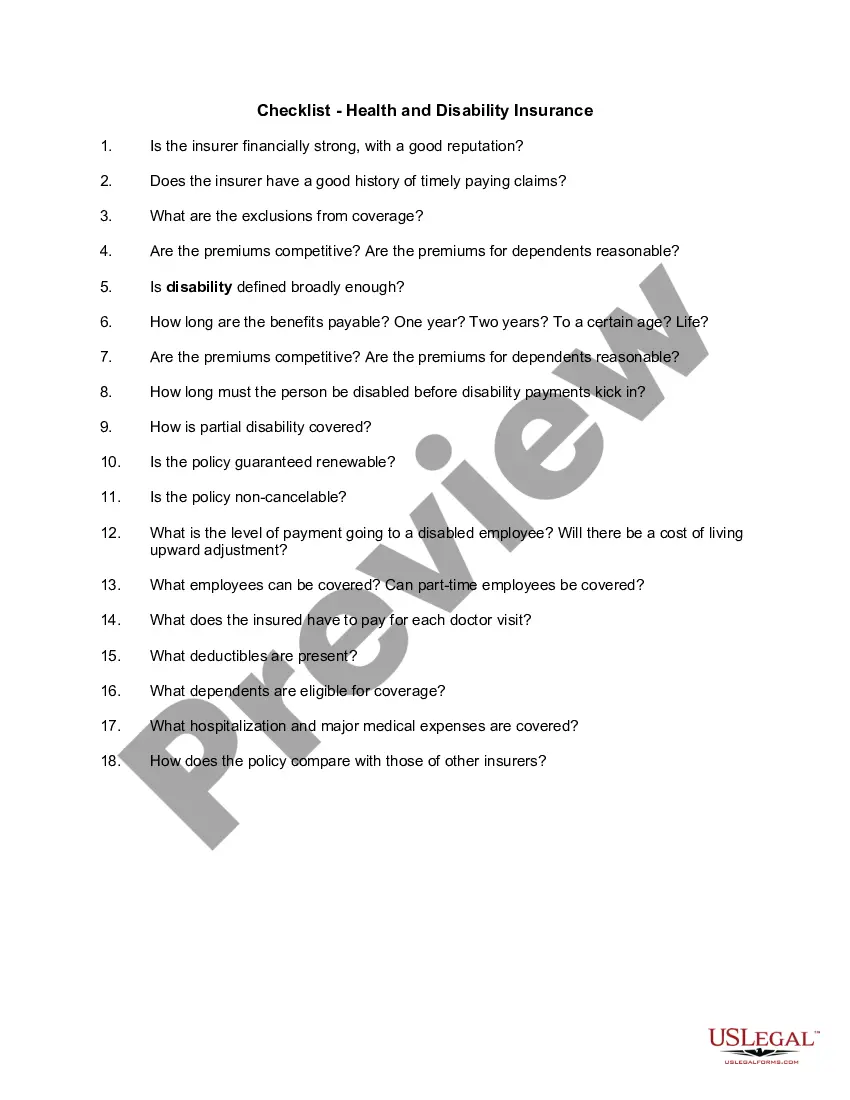
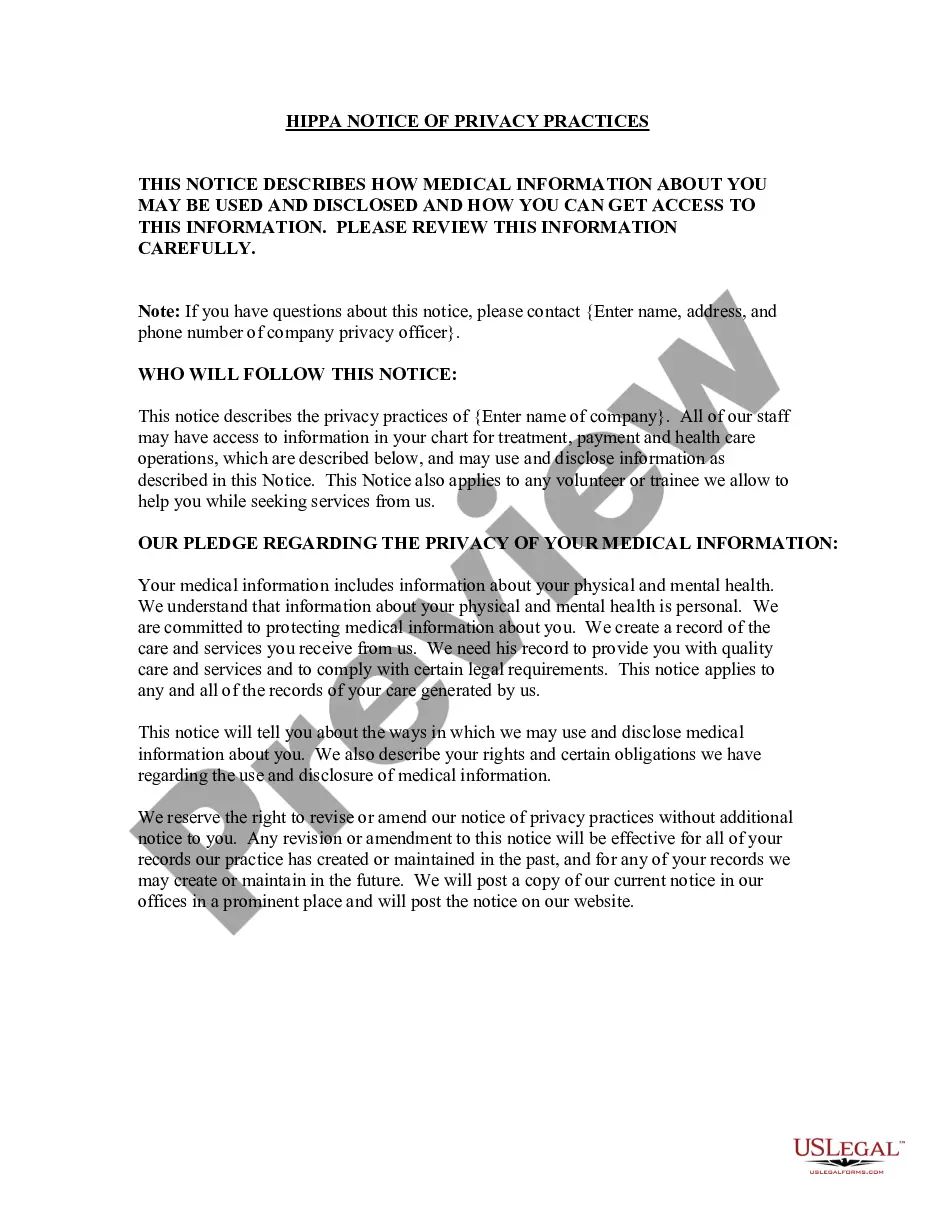
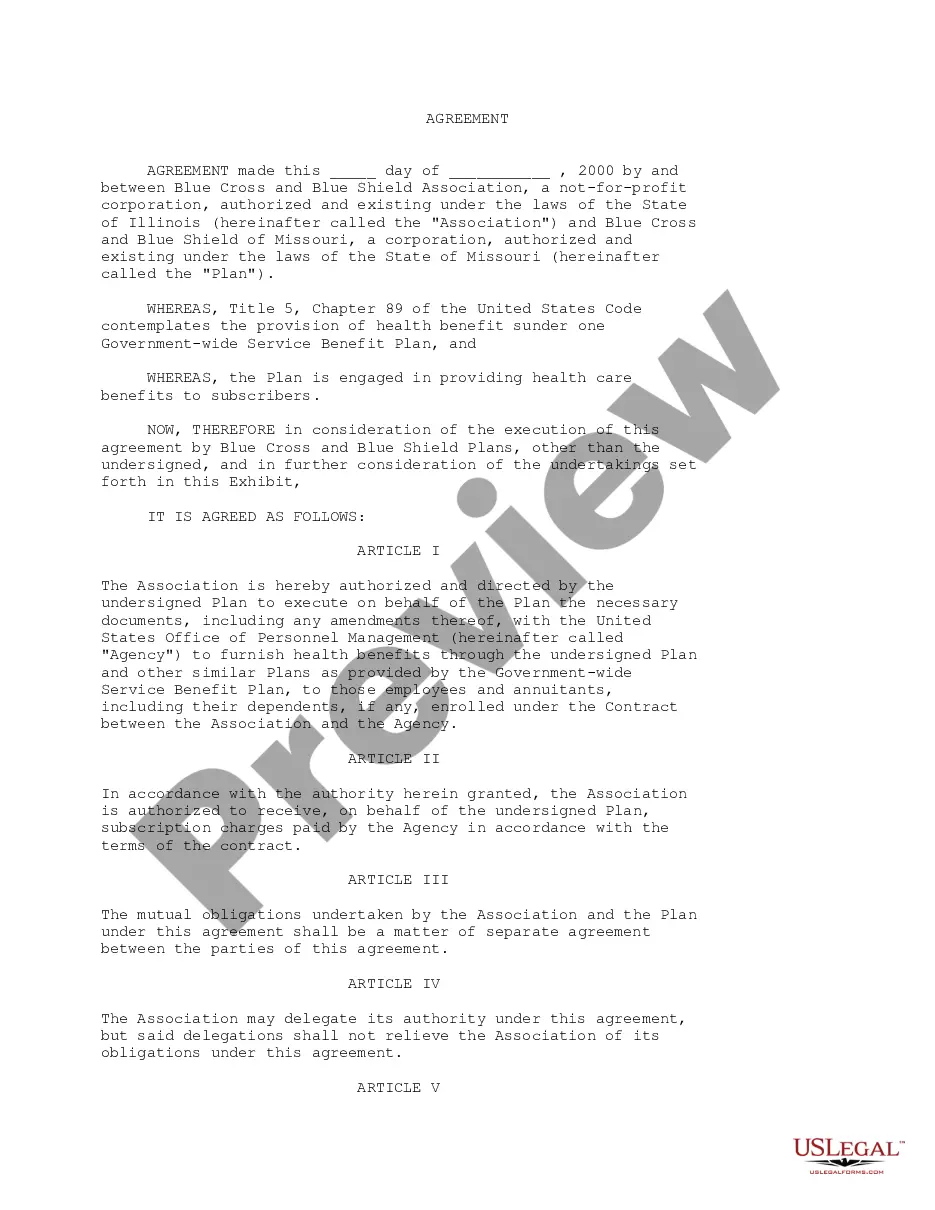
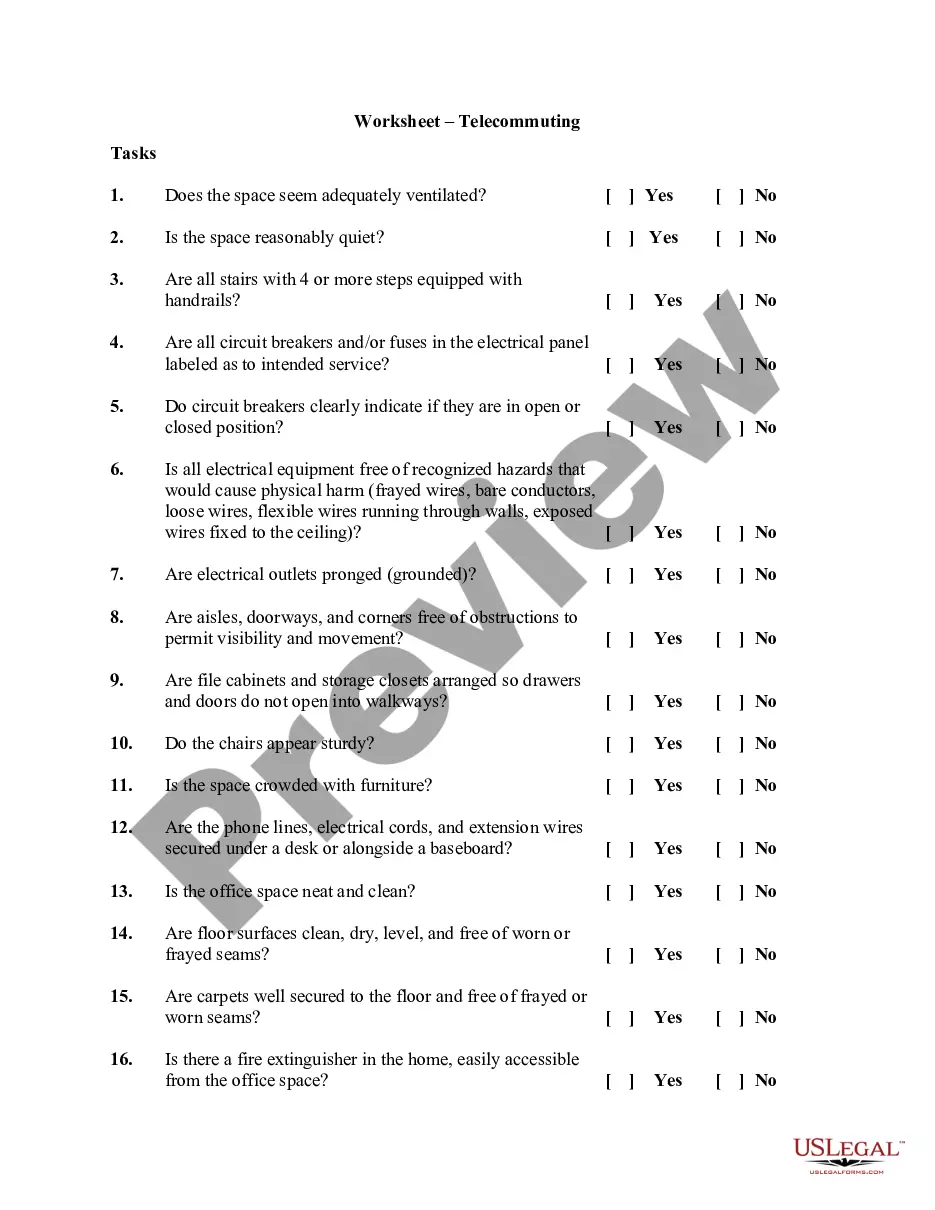
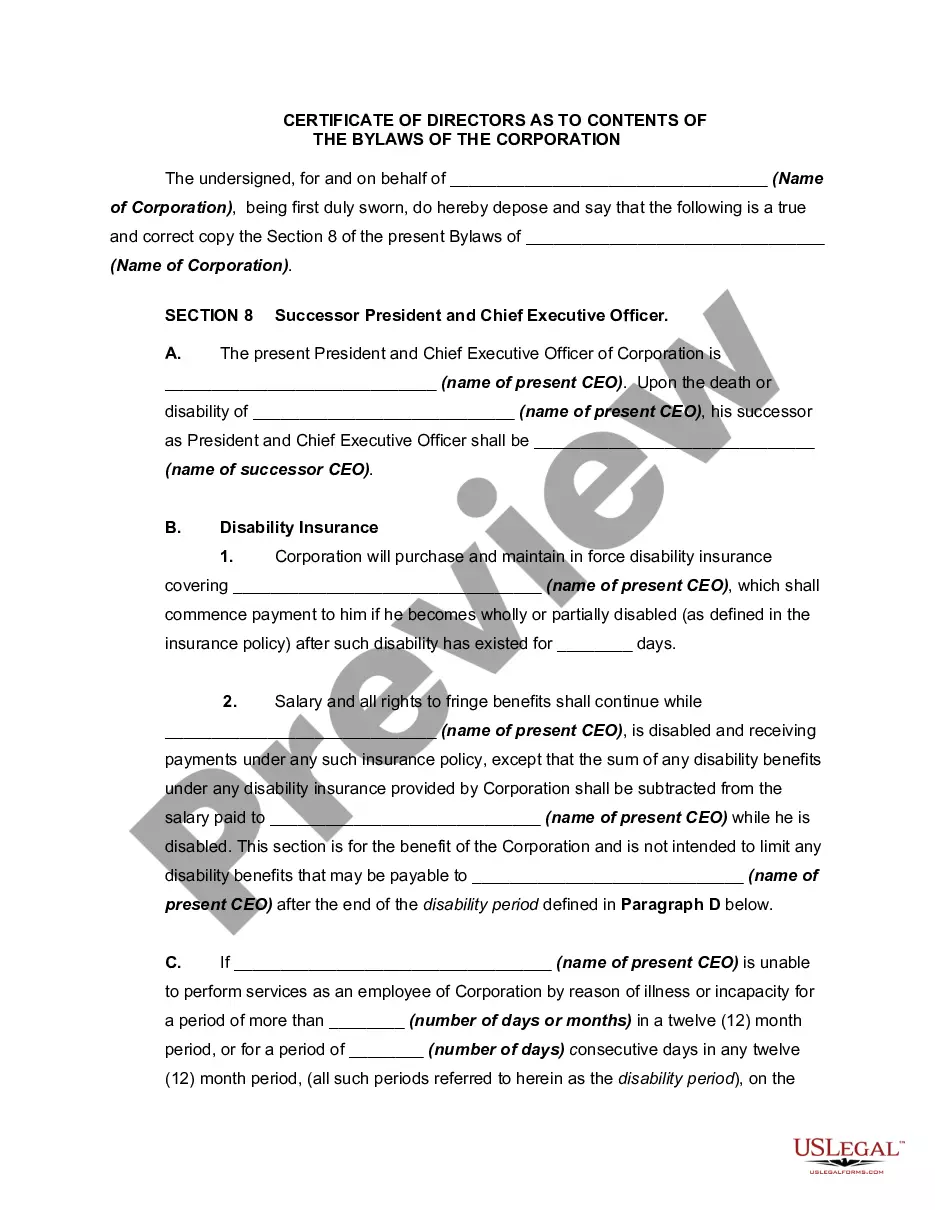
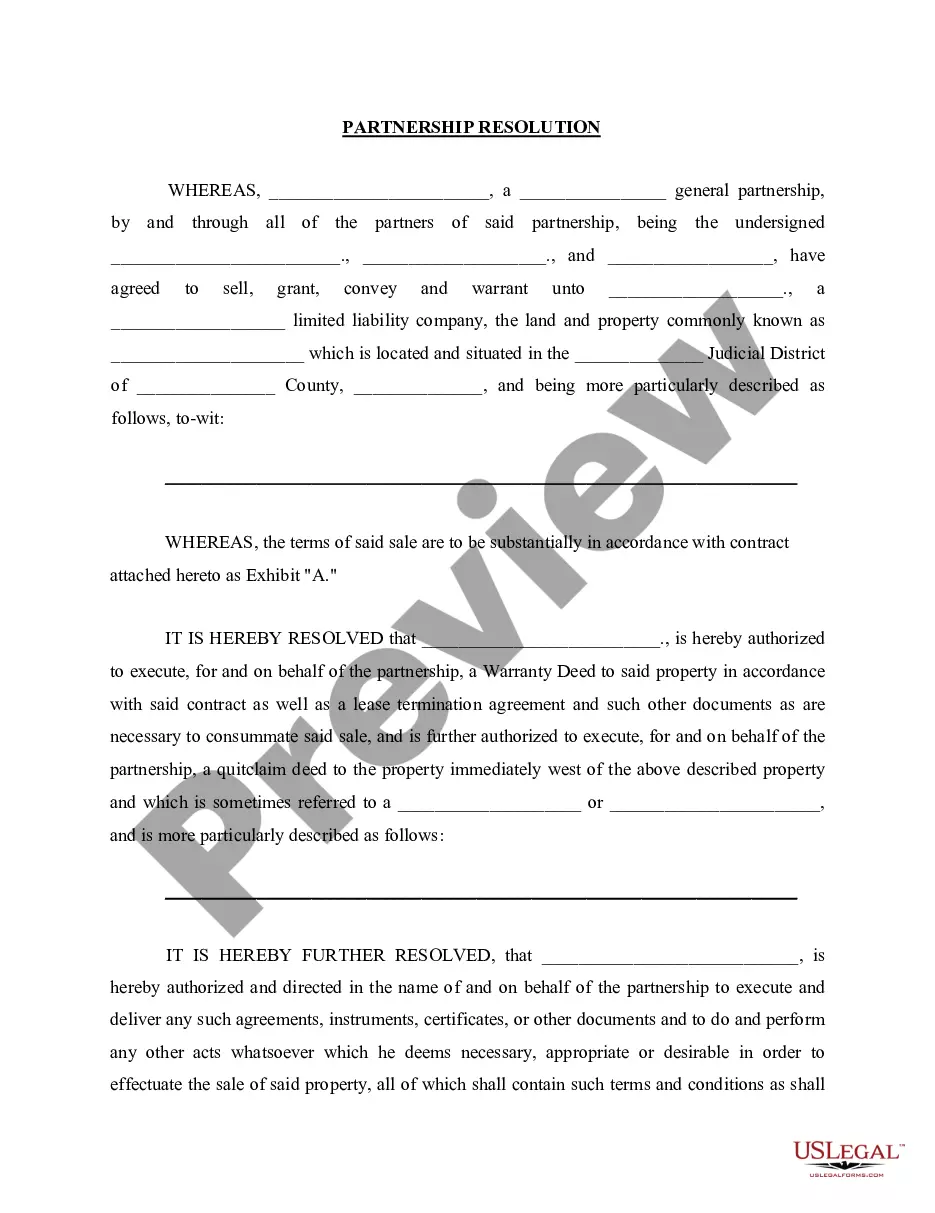
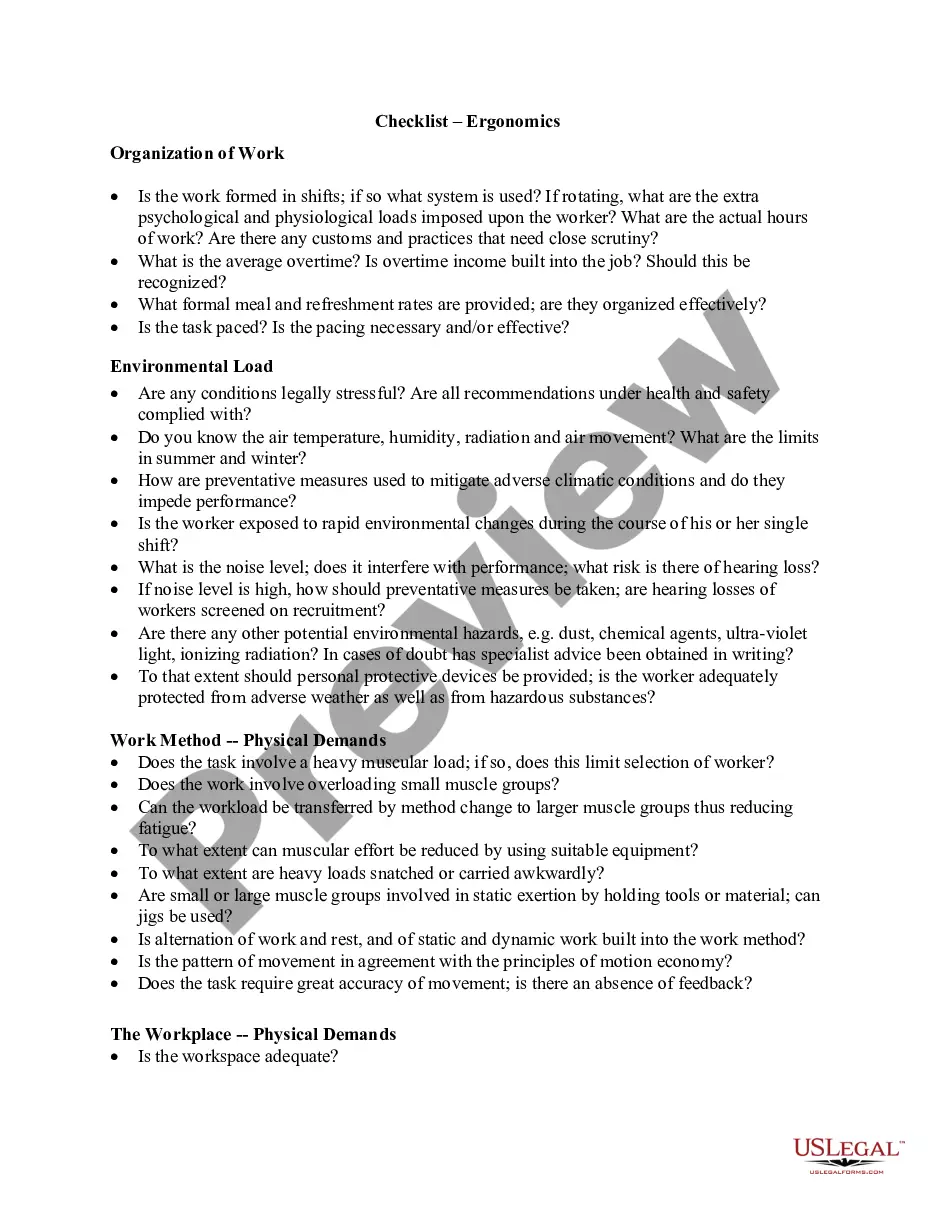
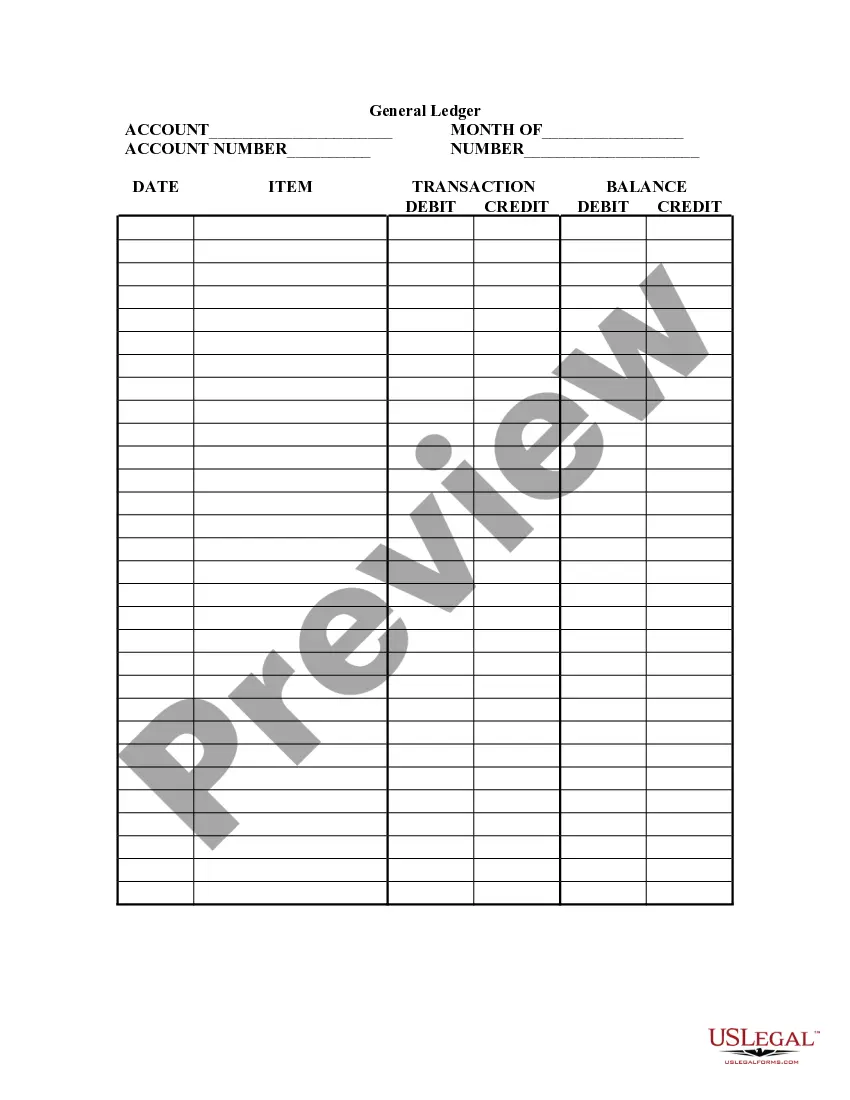
- Preview it (if this option available) and read the supporting description to determine whether Certificate Plan Coverage For Dependents is what you’re looking for.
- Start your search again if you need any other template.
- Register for a free account and select a subscription plan to purchase the template.
- Pick Buy now. Once the transaction is through, you can get the Certificate Plan Coverage For Dependents, complete it, print it, and send or send it by post to the necessary people or entities.
You can re-gain access to your documents from the My Forms tab at any time. If you’re an existing customer, you can simply log in, and find and download the template from the same tab.
No matter the purpose of your paperwork-be it financial and legal, or personal-our platform has you covered. Try US Legal Forms now!
Form popularity
FAQ
A Dependent Eligibility Verification (DEV) is simply the process by which you verify the relationship between the participant and their dependents to ensure they should in fact be eligible for coverage. Most participants do not intentionally carry ineligible dependents, they simply do not understand plan rules.
Copies of legal, government-issued documents are required to show your relationship to the dependent. These might include tax returns, marriage license, birth certificate and/or bank statements, based on the dependent you're covering (spouse, biological child, adopted child etc.).
A dependent is a person who is eligible for coverage under a policyholder's health insurance coverage. The policyholder is the individual who has primary eligibility for coverage ? for example, an employee whose employer offers health insurance benefits. A dependent may be a spouse, domestic partner, or child.
This Form 1095-B provides information about the individuals in your tax family (yourself, spouse, and dependents) who had certain health coverage (referred to as ?minimum essential coverage?) for some or all months during the year.
Beginning in 2023, a new state law allows adult children to add their dependent parent or stepparent to their health plan policy, as long as the dependent parent or stepparent is not eligible for or enrolled in Medicare and they live in the health plan's service area.