Contra Costa California Model COBRA Continuation Coverage Election Notice
Description
How to fill out Model COBRA Continuation Coverage Election Notice?
Drafting legal documents can be tedious. Moreover, if you choose to enlist a lawyer to create a business contract, ownership transfer documents, pre-nuptial agreement, divorce documents, or the Contra Costa Model COBRA Continuation Coverage Election Notice, it could end up costing you a lot.
So what is the optimal method to conserve time and money while preparing legitimate documents that fully comply with your state and local regulations? US Legal Forms serves as an excellent resource, whether you are in need of templates for personal or business purposes.
Don’t fret if the form doesn’t meet your needs—search for the appropriate one in the header. Click Buy Now once you locate the required template and select the most suitable subscription. Log In or create an account to complete your subscription payment. Make a payment via credit card or PayPal. Select the file format for your Contra Costa Model COBRA Continuation Coverage Election Notice and save it. Once done, you can print it out and fill it in manually or upload the document to an online editor for a quicker and more convenient completion. US Legal Forms allows you to utilize all the documents acquired multiple times—you can locate your templates in the My documents tab in your profile. Give it a try now!
- US Legal Forms represents the largest online collection of state-specific legal documents, offering users the latest and professionally validated forms for any scenario all gathered in one place.
- Thus, if you require the most current version of the Contra Costa Model COBRA Continuation Coverage Election Notice, you can readily find it on our platform.
- Acquiring the documents requires minimal time.
- Users with existing accounts should verify their subscription is active, Log In, and select the template using the Download button.
- If you do not have a subscription yet, here’s how to obtain the Contra Costa Model COBRA Continuation Coverage Election Notice.
- Browse the page and confirm that a template is available for your area.
- Review the form description and utilize the Preview option, if provided, to make sure it’s the template you are searching for.
Form popularity
FAQ
There are several other scenarios that may explain why you received a COBRA continuation notice even if you've been in your current position for a long time: You may be enrolled in a new plan annually and, therefore, receive a notice each year. Your employer may have just begun offering a health insurance plan.
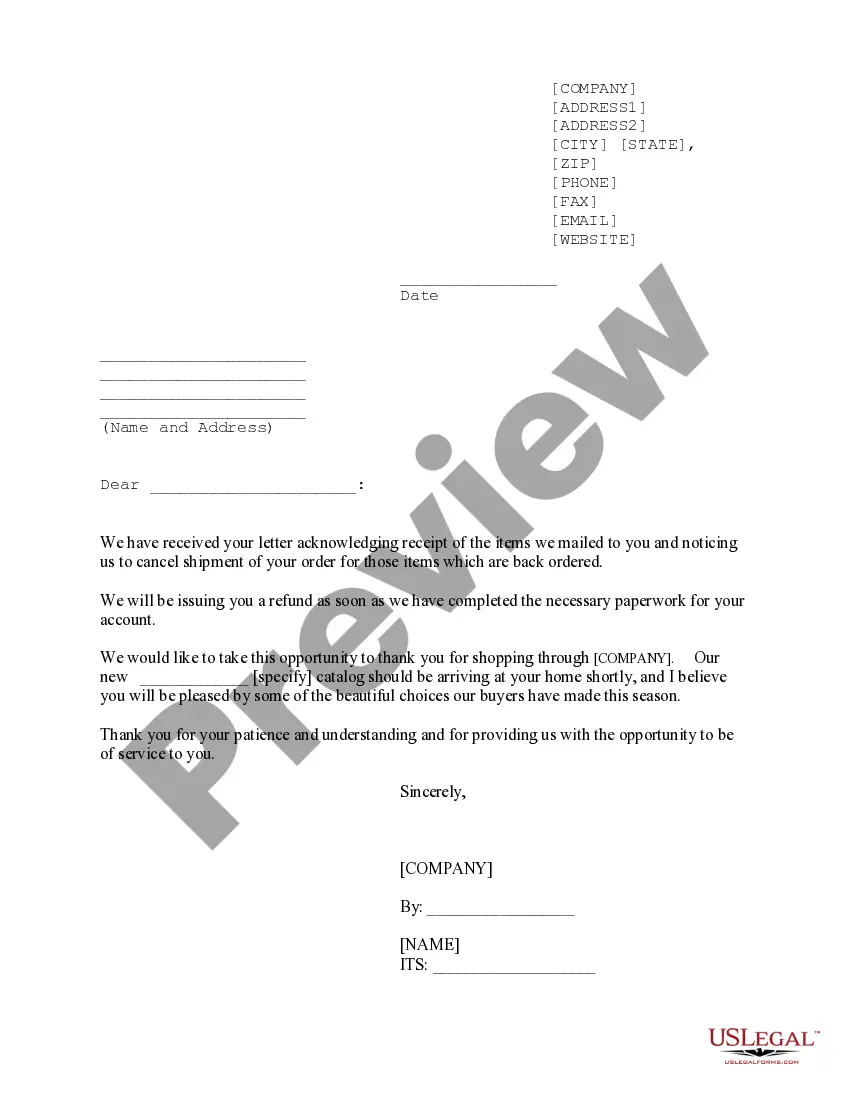
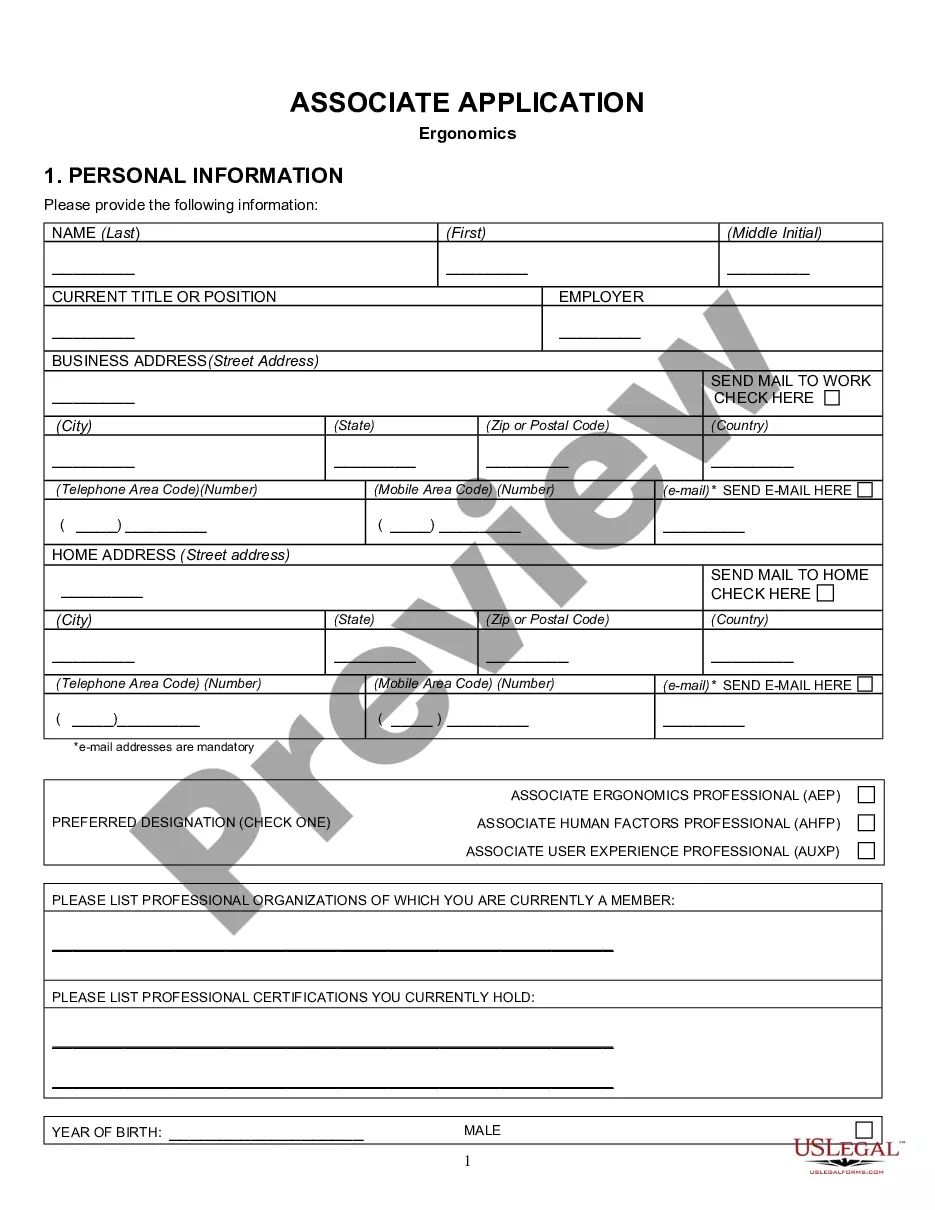
COBRA Election Notice The election notice describes their rights to continuation coverage and how to make an election. The election notice should include: 2022 The name of the plan and the name, address, and telephone number of the plan's COBRA.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) health benefit provisions amend the Employee Retirement Income Security Act, the Internal Revenue Code and the Public Health Service Act to require group health plans to provide a temporary continuation of group health coverage that otherwise might be
Meet the Deadlines You should get a notice in the mail about your COBRA and Cal-COBRA rights. You have 60 days after being notified to sign up. If you are eligible for Federal COBRA and did not get a notice, contact your employer. If you are eligible for Cal-COBRA and did not get a notice, contact your health plan.
The Department of Labor has developed a model Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) continuation coverage extended election notice that the Plan may use to provide the election notice to qualified beneficiaries currently enrolled in COBRA continuation coverage due to reduction in hours or
Time employee has to apply: 30 days after termination; 60 days if employer fails to give notice. Employers affected: All employers who offer group health insurance.
The COBRA election notice should describe all of the necessary information about COBRA premiums, when they are due, and the consequences of payment and nonpayment. Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
Adam's initial 60-day COBRA election deadline would generally be January 30, 2021 (i.e., 60 days from December 1, 2020). On December 31, 2020, Adam elects COBRA coverage retroactive to December 1, 2020.
Qualified beneficiaries have 60 calendar days from the date of loss of coverage or from the date of receiving the COBRA Election Notice to elect COBRA coverage, whichever date is later.