Dallas Texas COBRA Continuation Coverage Election Form
Description
How to fill out COBRA Continuation Coverage Election Form?
Creating forms, such as the Dallas COBRA Continuation Coverage Election Form, to manage your legal matters is a demanding and lengthy endeavor.
Numerous situations necessitate the involvement of a lawyer, which further elevates the cost of this endeavor.
However, you can put your legal concerns into your own hands and address them independently.
You can retrieve it in the My documents section of your account - whether on desktop or mobile.
- US Legal Forms is here to assist.
- Our site features over 85,000 legal documents designed for an array of scenarios and life situations.
- We ensure every document complies with state laws, so you need not worry about any legal compliance issues.
- If you're already familiar with our site and hold a subscription with US, you understand how simple it is to acquire the Dallas COBRA Continuation Coverage Election Form template.
- Feel free to Log In to your account, download the template, and tailor it to your needs.
- Lost your document? No problem.
Form popularity
FAQ
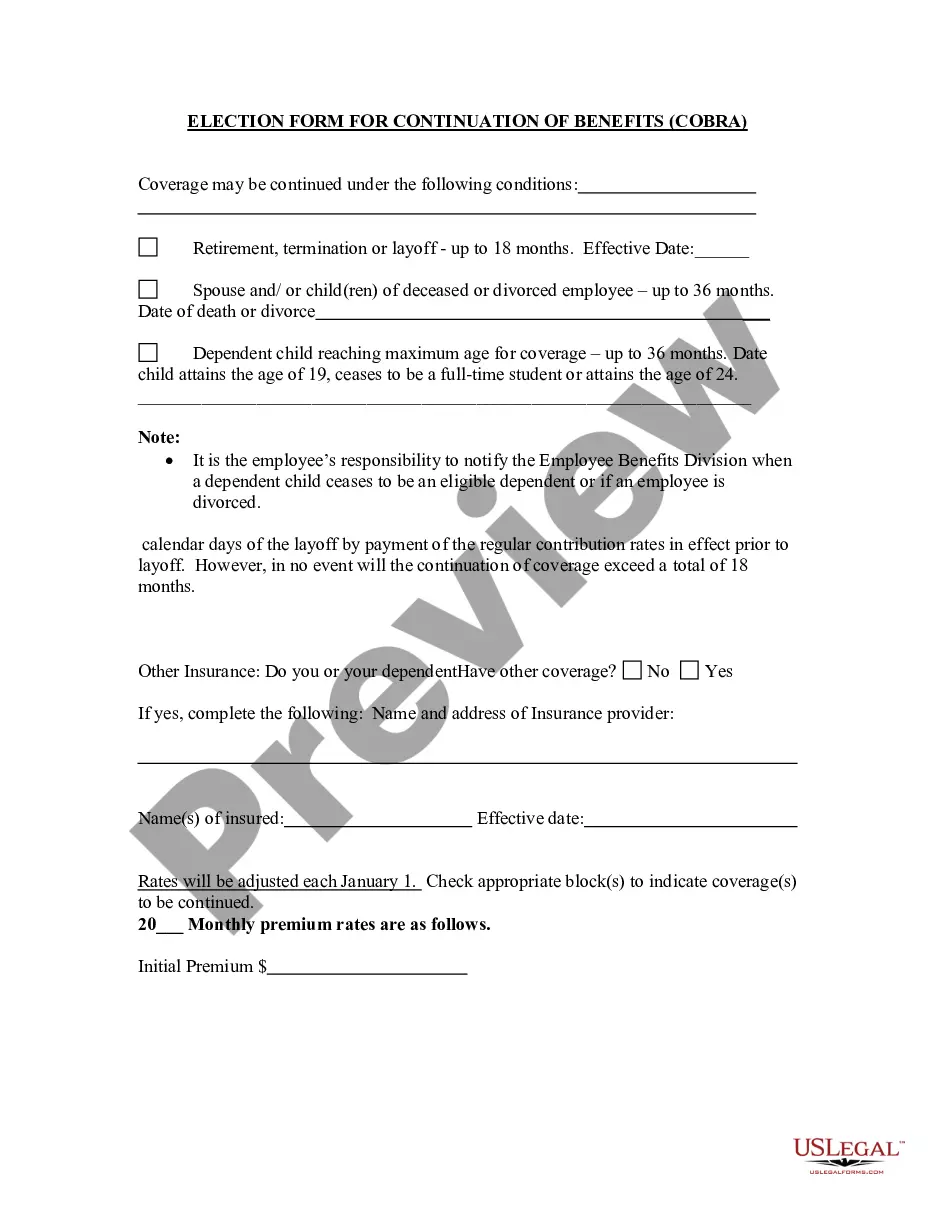
In most cases, COBRA provides for continuation of health plan coverage for up to 18 months following the work separation. COBRA rights accrue once a "qualifying event" occurs - basically, a qualifying event is any change in the employment relationship that results in loss of health plan benefits.
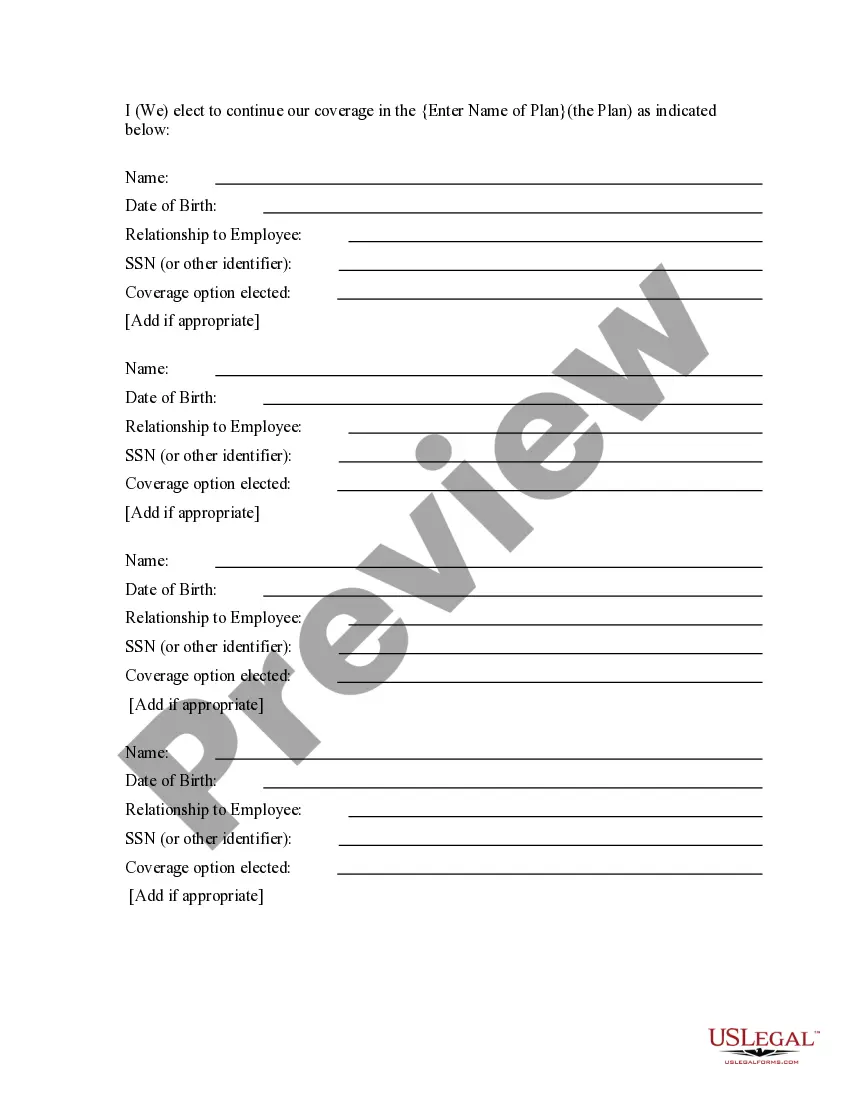
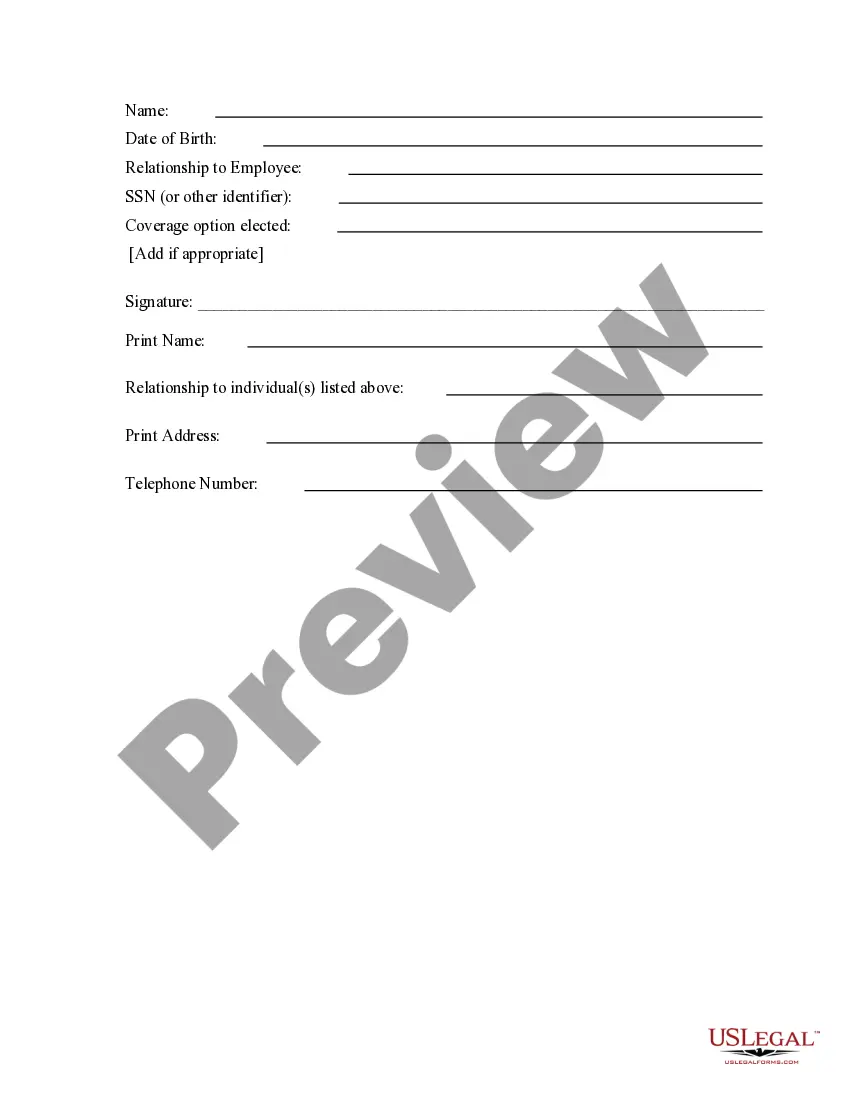
COBRA Election Form ("Form") The Employee should write the information of the member(s) to be covered under the COBRA policy. For COBRA coverage, Vantage must receive a copy of this Form within 60 days from the qualifying event.
The election notice should include the following information: The name of the plan and the name, address and telephone number of the plan's COBRA administrator. Identification of the qualifying event. Identification of the qualified beneficiaries (by name or by status).
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The Department of Labor has developed a model Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) continuation coverage extended election notice that the Plan may use to provide the election notice to qualified beneficiaries currently enrolled in COBRA continuation coverage due to reduction in hours or
For groups subject to COBRA, Texas law allows an additional six (6) months of coverage after COBRA ends. The law applies only to fully insured groups. COBRA participants are eligible for the additional six (6) months of continuation coverage after 18, 29, or 36 months of COBRA coverage.
COBRA Election Notice The election notice describes their rights to continuation coverage and how to make an election. The election notice should include: 2022 The name of the plan and the name, address, and telephone number of the plan's COBRA.
The COBRA election notice should describe all of the necessary information about COBRA premiums, when they are due, and the consequences of payment and nonpayment. Plans cannot require qualified beneficiaries to pay a premium when they make the COBRA election.
COBRA generally requires that group health plans sponsored by employers with 20 or more employees in the prior year offer employees and their families the opportunity for a temporary extension of health coverage (called continuation coverage) in certain instances where coverage under the plan would otherwise end.
COBRA (Consolidated Omnibus Budget Reconciliation Act of 1985) is a federal law that requires employers of 20 or more employees who offer health care benefits to offer the option of continuing this coverage to individuals who would otherwise lose their benefits due to termination of employment, reduction in hours or