Salt Lake Utah Summary of Rights and Obligations under COBRA
Description
How to fill out Summary Of Rights And Obligations Under COBRA?
How long does it typically take you to draft a legal document.
Given that each state has its own laws and regulations for every situation in life, locating a Salt Lake Summary of Rights and Obligations under COBRA that fulfills all local guidelines can be overwhelming, and hiring a professional lawyer for it can often be expensive.
Numerous online services provide the most sought-after state-specific documents for download, but utilizing the US Legal Forms collection is the most advantageous.
Create an account on the platform or Log In to continue to payment options. Proceed to pay via PayPal or credit card. Change the file format if required. Click Download to save the Salt Lake Summary of Rights and Obligations under COBRA. You can print the template or use any preferred online editor to fill it out electronically. Regardless of how often you need to use the obtained template, you can locate all the samples you’ve saved in your account by accessing the My documents section. Give it a shot!
- US Legal Forms is the largest online repository of templates, categorized by states and areas of application.
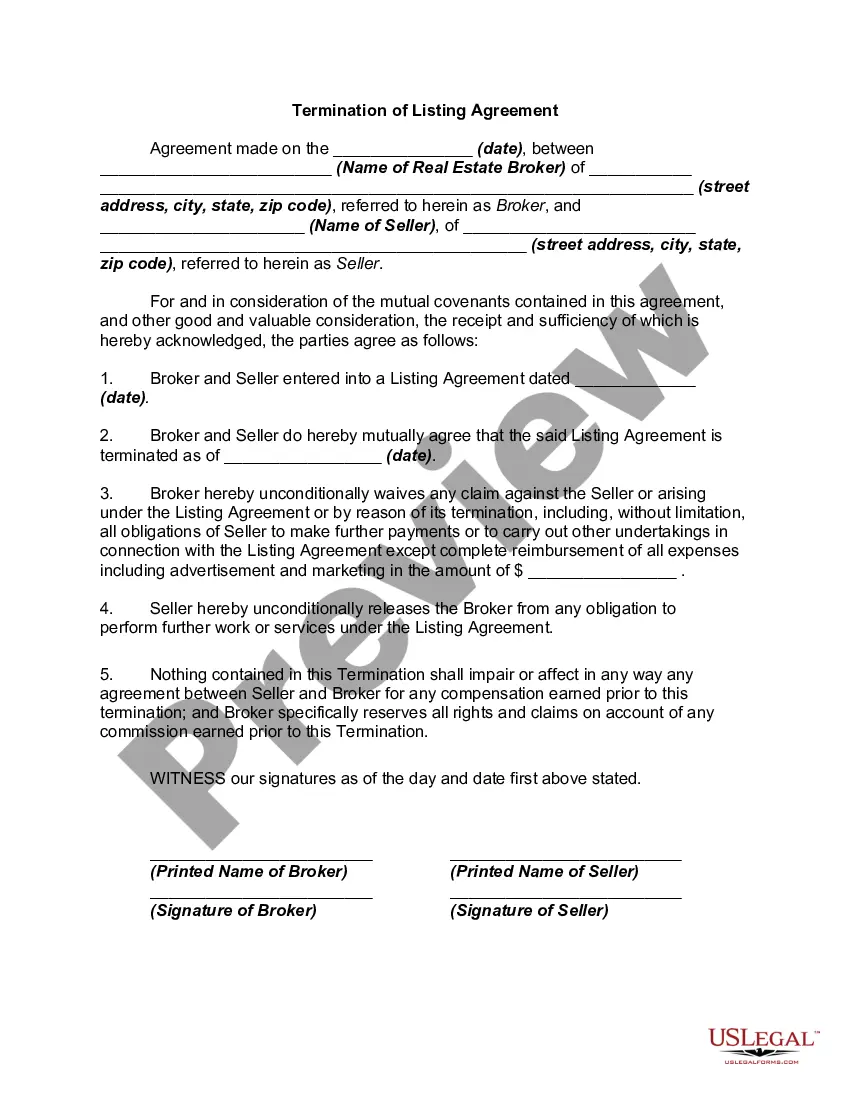
- In addition to the Salt Lake Summary of Rights and Obligations under COBRA, you can discover any specific form necessary to manage your business or personal matters, in accordance with your local regulations.
- All templates are validated by experts, ensuring you can complete your documentation correctly.
- Using the service is fairly straightforward.
- If you already possess an account on the platform and your subscription is active, you only need to Log In, select the desired sample, and download it.
- You can keep the file in your account for future access.
- If you are new to the platform, there will be additional steps to finish before you obtain your Salt Lake Summary of Rights and Obligations under COBRA.
- Review the information on the page you’re currently viewing.
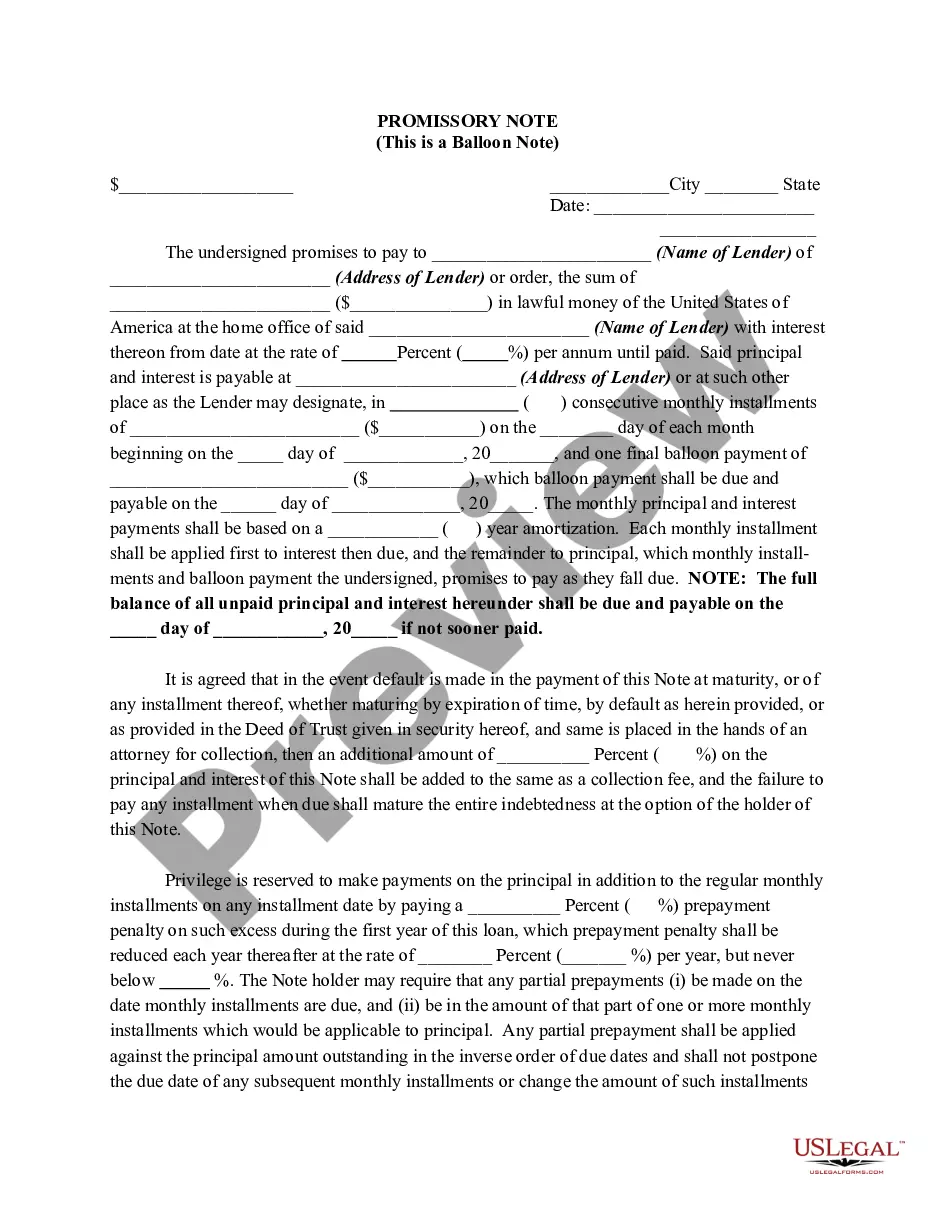
- Read the description of the template or Preview it (if available).
- Search for another form using the corresponding option in the header.
- Click Buy Now when you’re sure about the chosen file.
- Select the subscription plan that best fits your needs.
Form popularity
FAQ
You may be able to keep your job-based health plan through COBRA continuation coverage. COBRA is a federal law that may let you pay to stay on your employee health insurance for a limited time after your job ends (usually 18 months). You pay the full premium yourself, plus a small administrative fee.
Under COBRA, a person who has been terminated for gross misconduct may be denied COBRA. Gross misconduct is not specifically defined by COBRA, but when based on an employer's practice or policy it could include misrepresentation during the hiring process or falsifying information on a Form I-9.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
Voluntary or involuntary termination of the covered employee's employment for any reason other than gross misconduct. Reduction in the hours worked by the covered employee below plan eligibility requirements. Covered employee becoming entitled to Medicare. Divorce or legal separation of the covered employee.
Under federal law, employers with 20 or more full-time (or full-time-equivalent) employees must offer COBRA to their employees and their spouses/dependents. Under Utah law, employers with less than 20 full-time (or full-time equivalent) employees can offer COBRA to these employees and their spouses/dependents.
Q3: Which employers are required to offer COBRA coverage? COBRA generally applies to all private-sector group health plans maintained by employers that had at least 20 employees on more than 50 percent of its typical business days in the previous calendar year.
COBRA Is The Same Insurance You Had By using your COBRA right, you simply have the same employer-sponsored health plan you just had before you lost it. When you elect to stay on your employer's health insurance, you keep your same doctors, copays and prescription coverage.
Under the Employment Retirement Income Security Act of 1974 (ERISA), a penalty of up to $110 per day may be imposed for failing to provide a COBRA notice.
As an employer, you are responsible for notifying your former employee of the right to elect COBRA continuing health care coverage under your group plan. Most employers will include COBRA coverage information in the business employee handbook and as part of an employee's exit paperwork.
The general notice describes general COBRA rights and employee obligations. This notice must be provided to each covered employee and each covered spouse of an employee who becomes covered under the plan. The notice must be provided within the first 90 days of coverage under the group health plan.