Washington Notice from Employer to Employee Regarding Early Termination of Continuation Coverage
Description
How to fill out Notice From Employer To Employee Regarding Early Termination Of Continuation Coverage?
Are you in the location that necessitates documents for occasional organization or specific purposes every time.
There are numerous legal document templates accessible online, yet finding forms you can rely on isn't straightforward.
US Legal Forms provides a vast array of form templates, including the Washington Notice from Employer to Employee Regarding Early Termination of Continuation Coverage, designed to meet federal and state requirements.
Once you have obtained the correct form, just click Get now.
Select a convenient document format and download your copy.
- If you are already familiar with the US Legal Forms website and have an account, simply Log In.
- After that, you can download the Washington Notice from Employer to Employee Regarding Early Termination of Continuation Coverage template.
- If you don't have an account and wish to start using US Legal Forms, follow these steps.
- Find the form you need and make sure it is for the correct area/region.
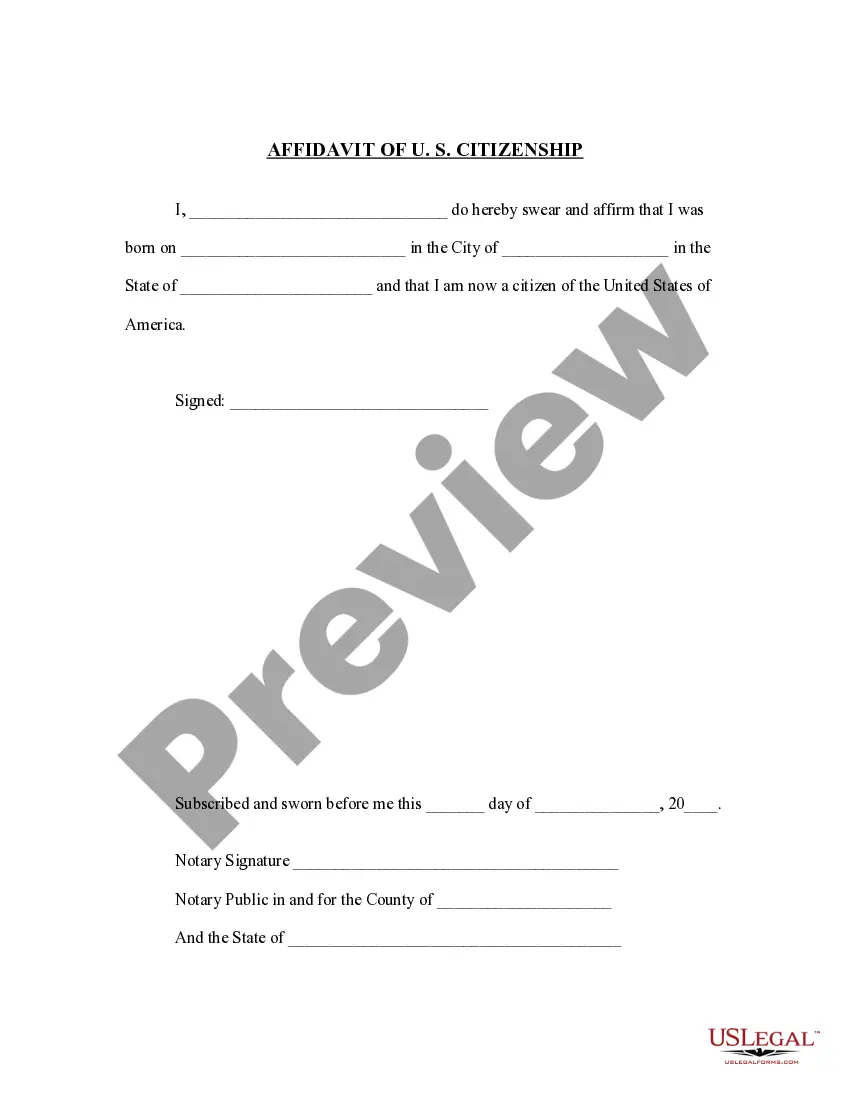
- Use the Review option to check the form.
- Examine the details to confirm that you have selected the correct form.
- If the form isn't what you're looking for, utilize the Search field to find the form that suits your needs.
Form popularity
FAQ
This type of program is commonly referred to as continuation coverage. Often related to the Washington Notice from Employer to Employee Regarding Early Termination of Continuation Coverage, continuation coverage ensures that laid-off employees can retain their health insurance benefits despite a loss of employment. It provides a crucial safety net during uncertain times.
This allows you and your eligible dependents to continue medical, dental, life, and accidental death and dismemberment (AD&D) insurance on a self-pay basis for up to 29 months.
The Consolidated Omnibus Budget Reconciliation Act (COBRA) gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss,
The Consolidated Omnibus Budget Reconciliation Act, known as COBRA, is a federal law that allows employees to continue their employer-provided health insurance after they are laid off or fired, or they otherwise become ineligible for benefits (for example, because they quit or their hours are reduced below the
The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) amended the Public Health Service Act, the Internal Revenue Code and the Employee Retirement Income Security Act (ERISA) to require employers with 20 or more employees to provide temporary continuation of group health coverage in certain situations
Typically, health insurance runs until the end of the month in which you quit. That means if your last day was March 3, you may have health insurance until March 31 of that same year. By law, any company with 20 or more employees must offer COBRA coverage to an employee who is leaving, no matter the reason.
The effective date of a separation is the day after the last day worked on the job except in the following circumstances. In the following cases, the effective date of separation is the day after the end of these events: an unpaid leave of absence for any reason.
If you are laid-off or quit your job, COBRA will pay your health care costs up until 18 months following termination of employment. However, you must have both dental and vision coverage while employed if you want them covered by Cobra after quitting.
Paying for COBRA coverage In fact, the law allows the employer to charge 102 percent of the premium, and to keep the 2 percent to cover your administrative costs. When an employee gets extended COBRA coverage due to disability, you can charge 150 percent of the premium for months 18 through 29.
You have only 60 days from the date you lost your employer coverage to purchase coverage directly from us or another health insurance carrier. If you do not enroll within 60 days, you must wait until the next open enrollment period to buy an individual health plan.